Abstract
Narcolepsy in children is a serious disorder marked by a chronic course and lifelong handicap in school performance and choice of employment, by free time activity limitation, and by behavior and personality changes, all of which constitute a major influence on the quality of life. Increased daytime sleepiness may be the only sign at the disease onset, with attacks of sleep becoming longer and lasting up to hours. Also present may be confusional arousals with features of sleep drunkenness. Paradoxically, preschool and young children may show inattentiveness, emotional lability, and hyperactive behavior. Cataplexy may develop after onset of sleepiness and affect mainly muscles of the face. Hypnagogic hallucinations and sleep paralysis are seldom present. Multiple Sleep Latency Test criteria are not available for children younger than 6 years. The haplotype (HLA-DQB1:0602) can be associated with the disorder; however, the best predictor of narcolepsy–cataplexy is hypocretin deficiency. The treatment generally used in adults is regarded as off-label in childhood, which is why the management of pediatric narcolepsy is difficult .
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
McKenna C, McNicholas F. Childhood onset narcolepsy. A case report. Eur Child Adolesc Psychiatry. 2003;1:43–7.
Morish E, King MA, Smith IE, Shneerson JM. Factors associated with a delay in the diagnosis of narcolepsy. Sleep Med. 2004;5:37–41.
Guilleminault C, Pelayo R. Narcolepsy in prepubertal children. Ann Neurol. 1998;43:135–42.
Serra L, Montagna P, Mignot E, Lugaresi E, Plazzi G. Cataplexy features in childhood narcolepsy. Mov Disord. 2008;23:858–65.
Nevsimalova S, Pretl M, Vankova J, Blazejova K, Sonka K. Narcolepsy in children and adolescents. In: Evrard P, Richelme C, Tardieu M, editors. 3rd EPNS congress. Bologna: Monduzzi; 1999. p. 73–7.
Einen MA, Aran A, Mignot E, Nishino S. Pre-versus post-pubertal narcolepsy in children. Sleep. 2009;32(Suppl):A249–50.
Dauvilliers Y, Montplaisir J, Cochen V, Desautels A, Einen M, Lin L, et al. Post-H1NH1 narcolepsy-cataplexy. Sleep. 2010;33:1428–30.
Han F, Lin L, Warby SC, Faraco J, Li J, Dong SX, et al. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Ann Neurol. 2011;70:410–7. Narcolepsy onset is highly correlated with seasonal and annual patterns of upper airway infections, including H1N1 influenza. In 2010, the peak seasonal onset of narcolepsy was phase-delayed by 6 months relative to winter H1N1 infections, and the correlation was independent of H1N1 vaccination in most of the sample.
Partinen M, Saarenpää-Heikkilä O, Ilveskoski I, Hublin C, Linna M, Olsén P, et al. Increased incidence and clinical picture of childhood narcolepsy following the 2009 H1N1 pandemic vaccination campaign in Finland. PLoS One. 2012;7:e33723. A sudden increase in the incidence of abrupt childhood narcolepsy was observed in Finland in 2010. Pandemrix vaccination together with other environmental factors likely contributed to this increase in the number of genetically susceptible children.
Nohynek H, Jokinen J, Partinen M, Vaarala O, Kirjavainen T, Sundman J, et al. AS03 adjuvanted AH1N1 vaccine associated with an abrupt increase in the incidence of childhood narcolepsy in Finland. PLoS One. 2012;7:e33536.
Szakács A, Darin N, Hallböök T. Increased childhood incidence of narcolepsy in western Sweden after H1N1 infuenza vaccination. Neurology. 2013;80:1315–21.
Heier MS, Gautvik KM, Wannag E, Bronder KH, Midtlyng E, Kamaleri Y, et al. Incidence of narcolepsy in Norwegian children and adolescents after vaccination against H1N1 influenza A. Sleep Med. 2013;14:867–71.
Dauvilliers Y, Montplaisir J, Molinari N, Carlander V, Ondze B, Besset A, et al. Age at onset of narcolepsy in two large populations of patients in France and Quebeck. Neurology. 2001;57:2029–33.
Ohayon MM, Priest RG, Zulley J, Smirne S, Paiva T. Prevalence of narcolepsy symptomatology and diagnosis in the European general population. Neurology. 2002;58:1826–33.
Silber MH, Krahn LE, Olson E, Pankratz VS. The epidemiology of narcolepsy in Olmsted County, Minnesota: a population-based study. Sleep. 2002;25:197–202.
Challamel MJ, Mazzola ME, Nevšímalová S, Cannard C, Louis J, Revo S, et al. Sleep. 1994;17 Suppl 8:S17–20.
Dauvilliers Y, Gosselin A, Paquet J, Touchon J, Billiard M, Montplaisir J. Effect of age on MSLT results in patients with narcolepsy-cataplexy. Neurology. 2004;62:46–50.
Nevsimalova S, Buskova J, Kemlink D, Sonka K, Skibova J. Does age at the onset of narcolepsy influence the course and severity of the disease? Sleep Med. 2009;10:967–72.
Nevsimalova S, Jara C, Prihodova I, Kemlink D, Sonka K, Skibová J. Clinical features of childhood narcolepsy. Can cataplexy be foretold? Eur J Paediatr Neurol. 2011;15:320–5.
Vendrame M, Havaligi N, Matedeen-Ali C, Adams R, Kothare SV. Narcolepsy in children: a single-center clinical experience. Pediatr Neurol. 2008;38:314–20.
Andlauer O, Moore H, Rico T, Einen M, Kornum BR, Kanbayashi, et al. Predictors of hypocretin (orexin) deficiency in narcolepsy without cataplexy. Sleep. 2012;35:1247–55. Objective (HLA typing and sleep studies) but not subjective (symptomatic assessment) features predicted low CSF hcrt-1 levels in patients with narcolepsy without cataplexy.
American Academy of Sleep Medicine. International classification of sleep disorders. Diagnostic and coding manual, Electronic version. 3rd ed. Westchester: American Academy of Sleep Medicine; 2014. The new classification distinguishes between two basic forms of narcolepsy—narcolepsy type 1 (with hcrt-1 deficiency) and narcolepsy type 2 (without hcrt-1 deficiency).
Kotagal S. Hypersomnia in children: interface with psychiatric disorders. Child Adolesc Psychiatr Clin N Am. 2009;18:967–77.
Peterson PC, Husain AM. Pediatric narcolepsy. Brain Dev. 2008;30:609–23.
Challamel MJ. Hypersomnia in children. In: Billiard M, editor. Sleep-physiology, investigation and medicine. New York: Kluwer/Plenum; 2003. p. 457–68.
Nevsimalova S. Narcolepsy in children and adolescents. In: Bassetti C, Billiard M, Mignot E, editors. Narcolepsy and hypersomnia. New York: Informa Healthcare USA; 2007. p. 67–75.
Nevsimalova S. Narcolepsy in childhood. Sleep Med Rev. 2009;13:169–80.
Wise MS. Childhood narcolepsy. Neurology. 1998;50 Suppl 1:S37–42.
Stores G, Montgomery P, Wiggs L. The psychosocial problems of children with narcolepsy and those with excessive daytime sleepiness of uncertain origin. Pediatrics. 2006;118:1116–23.
Aran A, Einen M, Lin L, Plazzi G, Nishino S, Mignot E. Clinical and therapeutic aspects of childhood-narcolepsy-cataplexy: a retrospective study of 51 children. Sleep. 2010;33:1457–64.
Pizza F, Franceschini C, Peltola H, Vandi S, Finotti E, Ingravallo F, et al. Clinical and polysomnographic course of childhood narcolepsy with cataplexy. Brain. 2013;136:3787–95. Childhood narcolepsy–cataplexy is characterized at onset by an abrupt increase in total sleep over 24 h, and by generalized hypotonia and motor overexcitability. Hypotonic phenomena and selected facial movements decreased over time and, tested against the disease duration and age, appeared as age-dependent.
Plazzi G, Pizza F, Palaia V, Franceschini C, Poli F, Moghadam KV, et al. Complex movement disorders at disease onset in childhood narcolepsy with cataplexy. Brain. 2011;134:3480–92. Patients with narcolepsy–cataplexy displayed a complex array of “negative” (hypotonia) and “active” (ranging from perioral movements to dyskinetic-dystonic movements or stereotypes) motor disturbances. A complex movement disorder at the onset may disappear later in the course of the disease.
Aran A, Lin L, Nevsimalova S, Plazzi G, Hong SC, Weiner K, et al. Elevated anti-streptococcal antibodies in patients with recent narcolepsy onset. Sleep. 2009;32:979–83.
Natarajan N, Jain SV, Chaudhry H, Hallinan BE, Simakajornboon N. Narolepsy-cataplexy: is streptococcal infection a trigger? J Clin Sleep Med. 2013;9:269–70.
Nevsimalova S, Roth B, Zouhar A, Zemanova H. The occurrence of narcolepsy-cataplexy and periodic hypersomnia in early childhood. In: Koella WP, Obal F, Schulz H, Wisser P, editors. Sleep ‘86. Stuttgart: Fisher; 1988. p. 399–401.
Guilleminault C, Pelayo R. Narcolepsy in children. A practical guide to its diagnosis, treatment and follow-up. Paediatr Drug. 2000;2:1–9.
Droogleever-Fortuyn H, Lappenschaar M, Nienhuis F, Furer J, Hodiamont P, Rijnders C, et al. Hypnagogic hallucinations and “psychotic” symptoms in narcolepsy: a comparison with control subjects and schizophrenic patients. Sleep. 2009;32(Suppl):A244–5.
American Academy of Sleep Medicine. International classification of sleep disorders. Diagnostic and coding Manual. 2nd ed. Westchester: American Academy of Sleep Medicine; 2005.
Pisko J, Pastorek L, Buskova J, Sonka K, Nevsimalova S. Nightmares in narcolepsy: underinvestigated symptom? Sleep Med. 2014. doi:10.1016/j.sleep.2014.03.006.
Vernet C, Arnulf A. Narcolepsy with long sleep time: a specific entity? Sleep. 2009;32:1229–35.
Nevsimalova S, Vankova J, Pretl M, Bruck D. Narcolepsy in children and adolescents – clinical and psychosocial aspects (in Czech). Ces Slov Neurol Neurochir. 2002;65:169–74.
Inocente CO, Gustin MP, Lauvault S, Perret AG, Christol N, et al. Quality of life in children with narcolepsy. CNS Neurosci Ther. 2014. doi:10.1111/cns.12291. Narcoleptic children and adolescents were at high risk of poor health-related quality of life. Depressive symptoms had a major impact on affected children’s quality of life.
Dahl RE, Holttum J, Trubnick L. A clinical picture of child and adolescent narcolepsy. J Am Acad Child Adolesc Psychiatry. 1994;33:834–41.
Kotagal S, Krahn LE, Slocumb N. A putative link between childhood narcolepsy and obesity. Sleep Med. 2004;5:147–50.
Inocente CO, Lavault S, Lecendreux M, Dauvilliers Y, Reimao R, Gustin MP, et al. Impact of obesity in children with narcolepsy. CNS Neurosci Ther. 2013;19:521–8. Obesity affects more than 50 % of narcoleptic children, mostly younger at disease onset, and has a deleterious impact on sleep quality as well as on school attendance.
Dahmen N, Bierbrauer J, Kasten M. Increased prevalence of obesity in narcoleptic patients and relatives. Eur Arch Psychiatry Clin Neurosci. 2001;251:85–9.
Kok SW, Overeem S, Visscher TL, Lammers GJ, Seidell JC, Pijl H, et al. Hypocretin deficiency in narcoleptic humans is associated with abdominal obesity. Obes Res. 2003;11:1147–54.
Lammers GJ, Pijl H, Iestra J, Buunk G, Meinders AE. Spontaneous food choice in narcolepsy. Sleep. 1996;19:75–6.
Schuld A, Beitinger PA, Dalal M, Geller F, Wetter TC, Albert ED, et al. Increased body mass index (BMI) in male narcoleptic patients, but not in HLA-DR2-positive healthy male volunteers. Sleep Med. 2002;3:335–9.
Nishino S, Ripley B, Overeem S, Nevsimalova S, Lammers GJ, Vankova J, et al. Low cerebrospinal fluid hypocretin (orexin) and altered energy homeostasis in human narcolepsy. Ann Neurol. 2001;50:381–8.
Beuckmann CT, Yanagisawa M. Orexins: from neuropeptides to energy homeostasis and sleep/wake regulation. J Mol Med. 2002;80:329–42.
Crocker A, Espana RA, Papadopoulou M, Saper CB, Faraco J, Sakurai T, et al. Concomitant loss of dynorphin, NARP, and orexin in narcolepsy. Neurology. 2005;65:1184–8.
Arnulf I, Lin L, Zhang J, Russel J, Ripley B, Einen M, et al. CSF versus serum leptin in narcolepsy: is there an effect of hypocretin deficiency? Sleep. 2006;29:1017–24.
Chabas D, Foulon C, Gonzales J, Nasr M, Caen OL, Willer JC, et al. Eating disorder and metabolism in narcoleptic patients. Sleep. 2007;30:1267–73.
Plazzi G, Parmeggiani A, Mignot E, Lin L, Scano MC, Posar A, et al. Narcolepsy-cataplexy associated with precocious puberty. Neurology. 2006;66:1577–9.
Poli F, Pizza F, Mignot E, Ferri R, Pagotto U, Taheri S, et al. High prevalence of precocious puberty and obesity in childhood narcolepsy with cataplexy. Sleep. 2013;36:175–81. Narcolepsy–cataplexy occurring during prepubertal age is frequently accompanied by precocious puberty and overweight/obesity, suggesting an extended hypothalamic dysfunction.
Nishino S, Kanbayashi T. Symptomatic narcolepsy, cataplexy and hypersomnia, and their implication in the hypothalamic hypocretin/orexin system. Sleep Med Rev. 2005;9:269–310.
Marcus CL, Trescher WH, Halbower AC, Lutz J. Secondary narcolepsy in children with brain tumors. Sleep. 2002;25:435–9.
Vankova J, Stepanova I, Jech R, Elleder M, Lin L, Mignot E, et al. Sleep disturbance and hypocretin deficiency in Niemann-Pick disease type C. Sleep. 2003;26:427–30.
Smit LS, Lammers GL, Catsman-Berrevoets CE. Cataplexy leading to the diagnosis of Niemann-Pick disease. Pediatr Neurol. 2006;35:82–4.
Nevsimalova S. Genetic disorders and sleepiness. In: Thorpy MJ, Billiard M, editors. Sleepiness: causes, consequences and symptoms. Cambridge: Cambridge University Press; 2011. p. 335–50.
Walters AS, Silvestri R, Zucconi M, Chandrashekariah R, Konofal E. Review of the possible relationship and hypothetical links between attention deficit hyperactivity disorder (ADHD) and simple sleep related movement disorders, parasomnias, hypersomnias and circadian rhythm disorders. J Clin Sleep Med. 2008;4:591–600.
Dorris L, Zuberi SM, Scott N, Moffat C, McArthur I. Psychosocial and intellectual functioning in childhood narcolepsy. Dev Neurorehabil. 2008;11:187–94.
Zeman A, Douglas N, Aylward R. Narcolepsy mistaken for epilepsy. BMJ. 2001;322:216–8.
Macleod S, Ferrie C, Zuberi SM. Symptoms of narcolepsy in children misinterpretend as epilepsy. Epileptic Disord. 2005;7:13–7.
Bouvier E, Arnulf I, Claustrat B, Kocher L, Bastuji H, Lecendreux M, et al. Do children with idiopathic narcolepsy have a long sleep time? Sleep. 2009;32(Suppl):A97.
Kotagal S, Hartse KM, Walch JK. Characteristics of narcolepsy in pre-teenaged children. Pediatrics. 1990;85:205–9.
Han F, Lin L, Li J, Aran A, Dong SX, An P, et al. Presentation of primary hypersomnia in Chinese children. Sleep. 2011;5:627–32. Of children presenting with primary hypersomnia, 86% (361 of 417) met the criteria for narcolepsy–cataplexy. Puberty did not affect positivity on the MSLT as a diagnostic feature. Sleep paralysis was the only symptom that increased with increasing age. The age at onset appeared to be younger than usually reported in other studies.
Jambhekar SK, Com G, Jones E, Jackson R, Castro MM, Knight F, et al. Periodic limb movements during sleep in children with narcolepsy. J Clin Sleep Med. 2011;7:597–601.
Nevsimalova S, Prihodova I, Kemlink D, Lin L, Mignot E. REM behavior disorder (RBD) can be one of the first symptoms of childhood narcolepsy. Sleep Med. 2007;8:784–6.
Carskadon MA, Dement WC, Mitler M, Roth T, Westbrook P, Keenan S. Guidelines for the Multiple Sleep Latency Test (MSLT): a standard measure of sleepiness. Sleep. 1986;9:519–24.
Carskadon MA, Harvey K, Duke P, Anders TF, Litt IF, Dement WC. Pubertal change in daytime sleepiness. Sleep. 1980;3:453–60.
Kubota H, Kanbayashi T, Tanabe Y, Ito M, Takanashi J, Kohno Y, et al. Decreased cerebrospinal fluid hypocretin-1 levels near the onset of narcolepsy in 2 prepubertal children. Sleep. 2003;26:555–7.
Nevsimalova S, Mignot E, Sonka K, Arrigoni JL. Familial aspects of narcolepsy-cataplexy in the Czech Republic. Sleep. 1997;20:1021–6.
Mignot E, Lammers GJ, Ripley B, Okun M, Nevsimalova S, Overeem S, et al. The role of cerebrospinal fluid hypocretin in the diagnosis of narcolepsy and other hypersomnias. Arch Neurol. 2002;59:1553–62.
Savvidou A, Knudsen S, Olsson-Engman M, Gammeltoft S, Jennum P, Palm L. Hypocretin deficiency develops during onset of human narcolepsy with cataplexy. Sleep. 2013;36:147–8.
Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Pietro B. The pediatric daytime sleepiness scale (PDSS): sleep habits and school outcome in middle-school children. Sleep. 2003;26:455–8.
Snow A, Gozal E, Malhotra A, Tiosano D, Perlman R, Vega C, et al. Severe hypersleepiness after pituitary/hypothalamic surgery in adolescents: clinical characteristics and potential mechanisms. Pediatrics. 2002;110:e74.
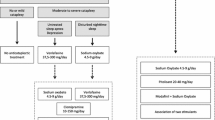
Murali H, Kotagal S. Off-label treatment of severe childhood narcolepsy-cataplexy with sodium oxybate. Sleep. 2006;29:1025–9.
Shankar R, Jalihal V, Walker M, Zeman A. Pseudocataplexy and transient functional paralysis: a spectrum of psychogenic motor disorder. J Neuropsychiatry Clin Neurosci. 2010;4:445–50.
Krahn LE, Hansen MR, Shepard JW. Pseudocataplexy. Psychosomatics. 2001;42:356–8.
Krahn LE. Reevaluating spells initially identified as cataplexy. Sleep Med. 2005;6:537.
Billiard M. Idiopathic hypersomnia. In: Thorpy MJ, Billiard M, editors. Sleepiness: causes, consequences and treatment. Cambridge: Cambridge University Press; 2011. p. 126–35.
Huang YS, Guilleminault C, Chen CH, Lai PC, Hwang FM. Narcolepsy-cataplexy and schizophrenia in adolescents. Sleep Med. 2014;15:15–22.
Guilleminault C, Cao MT. Narcolepsy: diagnosis and management. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 5th ed. Philadelphia: Elsevier Saunders; 2011. p. 957–68.
Lecendreux M, Bruni O, Franco P, Gringras P, Konofal E, Nevsimalova S, et al. Clinical experience suggests that modafinil is an effective and safe treatment for paediatric narcolepsy. J Sleep Res. 2012;21:481–3. Two-hundred five children and adolescents with narcolepsy were treated with modafinil, the age range was 4-18 years, and the prescribed dose varied from 50 to 600 mg. The patients had been treated for more than 10 years. The most frequent side effects were headache (13.7%), nervousness and irritability (6.5%), and loss of appetite (2.2%). No severe hypersensitivity reactions and no severe skin reactions were reported.
Davies M, Wilton L, Shakir S. Safety profile of modafinil across a range of prescribing indications, including off-label use, in a primary care setting in England. Drug Saf. 2013;36:237–46. More than 2.400 questionnaires (nine patients aged 16 years or younger) with narcolepsy treated with modafinil were evaluated. No serious skin reactions were reported.
Guilleminault C, Fromherz S. Narcolepsy. diagnosis and management. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 4th ed. Philadelphia: Elsevier Saunders; 2007. p. 780–90.
Greenhil LL, Pliszka S, Dulcan MK, Bernet W, Arnold V, Beitchman J, et al. Practice parameter for the use of stimulant medication in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry. 2002;41(Suppl2):26S–49S.
Ivanenko A, Tauman R, Gozal D. Modafinil in the treatment of excessive daytime sleepiness in children. Sleep Med. 2003;4:579–82.
Moller LR, Ostergaard JR. Treatment with venlafaxine in six cases of children with narcolepsy and with cataplexy and hypnagogic hallucinations. J Child Adolesc Psychopharmacol. 2009;19:197–201.
Lecendreux M, Poli F, Oudertte D, Benazzouz F, Donjacour CEHM, Franceschini C, et al. Tolerance and efficacy of sodium oxybate in childhood narcolepsy with cataplexy: a retrospective study. Sleep. 2012;35:709–11. Twenty-seven children with narcolepsy–cataplexy ranging from 6 to 16 years, evaluated retrospectively, had been treated with off-label sodium oxybate. Good efficacy and tolerability was documented in most of the patients.
Mansukhani MP, Kotagal S. Sodium oxybate in the treatment of childhood narcolepsy-cataplexy: a retrospective study. Sleep Med. 2012;13:606–10. Fifteen children and adolescents with narcolepsy–cataplexy treated with sodium oxybate had a mean age at diagnosis of 11 years (range 3-17). The treatment was effective in alleviating sleepiness and cataplexy, and the therapeutic response was sustained over time and without development of tolerance.
Lecendreux M, Maret S, Bassetti C, Mouren MC, Tafti M. Clinical efficacy of high-dose intravenous immunoglobulins near the onset of narcolepsy in a 10-year-old-boy. J Sleep Res. 2003;12:1–2.
DauvilliersY Y, Carlander B, River F, Touchon J, Tafti M. Successful management of cataplexy with intravenous immunoglobulins at narcolepsy onset. Ann Neurol. 2004;56:905–8.
Plazzi G, Poli F, Franceschini C, Parmeggiani A, Pirazzoli P, Bernardi F, et al. Intravenous high-dose immunoglobulin treatment in recent onset childhood narcolepsy with cataplexy. J Neurol. 2008;255:1549–54.
Hecht M, Lin L, Kushida CA, Umetsu DT, Taheri S, Einen M, et al. Immunosuppression with prednisone in an 8-year-old boy with an acute onset of hypocretin deficiency/narcolepsy. Sleep. 2003;26:809–10.
Chen W, Black J, Call P, Mignot E. Late-onset narcolepsy presenting as rapidly progressing muscle weakness: response to plasmapheresis. Ann Neurol. 2005;58:489–90.
Acknowledgments
Sona Nevsimalova was supported by PRVOUK-P26/LF1/4 and IGA MZ CR NT 13238-4/2012.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Sona Nevsimalova has received a grant from First Faculty of Medicine, Charles University, and the Grant Agency of the Ministry of Health, Czech Republic.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Sleep
Electronic supplementary material
Below is the link to the electronic supplementary material.
A sleep attack in a 7-year-old girl falling asleep to the ground even while playing with her toys. Her awakening is difficult and prolonged, with features of sleep drunkenness. Cataplectic attacks are evoked by a funny TV story and affect predominantly face muscles. Hypotonia of mimic muscles can be confused for a severe sleepiness (MPG 19793 kb)
Rights and permissions
About this article
Cite this article
Nevsimalova, S. The Diagnosis and Treatment of Pediatric Narcolepsy. Curr Neurol Neurosci Rep 14, 469 (2014). https://doi.org/10.1007/s11910-014-0469-1
Published:
DOI: https://doi.org/10.1007/s11910-014-0469-1