Abstract
Purpose of Review
Nosocomial extracardiac infections after cardiac surgery are a major public health issue affecting 3–8.2% of patients within 30–60 days following the intervention.
Recent Findings
Here, we have considered the most important postoperative infective complications that, in order of frequency, are pneumonia, surgical site infection, urinary tract infection, and bloodstream infection. The overall picture that emerges shows that they cause a greater perioperative morbidity and mortality with a longer hospitalization time and excess costs. Preventive interventions and corrective measures, diminishing the burden of nosocomial extracardiac infections, may reduce the global costs. A multidisciplinary team may assure a more appropriate management of nosocomial extracardiac infections leading to a reduction of hospitalization time and mortality rate.
Summary
The main and most current data on epidemiology, prevention, microbiology, diagnosis, and management for each one of the most important postoperative infective complications are reported. The establishment of an antimicrobial stewardship in each hospital seems to be, at the moment, the more valid strategy to counteract the challenging problems.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
After cardiac surgery, complications of various kinds, infectious and noninfectious, may affect several organs [1,2,3,4,5]. The overall prevalence of at least one of those complications is 66.6% [5], a really high percentage that also includes the nosocomial cardiac and extracardiac infections and gives us an idea of how important this issue is.
Narrowing our research, we are only discussing here the nosocomial extracardiac infections (NECI), which are all those not affecting the heart and whose onset is within two months from cardiac surgery intervention. These represent a major public health issue for a number of reasons: excess mortality (odds ratio 4.02), long-term hospitalization, greater risk of rehospitalization, and cost increase [6].
The high demand for cardiac surgical procedures, except for the recent decline due to the COVID-19 pandemic [7] and especially the fact that the major requests concern older and high-risk patients, explain why the trend of NECI is growing.
Obviously, patients’ risk factors and some types of bacteria involved have a greater influence on the severity of the NECI and consequently have a major impact on the hospitalization time and mortality rate in the first two months after the operation.
The implementation of the best practices in the management of patients affected by NECI is surely the most effective strategy to adopt in order to reduce its onset whose risk is estimated in a range between 3 and 8.2% within 30–60 days after cardiac surgery exposing the affected individuals to a 10–17-fold higher risk of postoperative mortality [8,9,10,11,12,13,14].
The management of patients undergoing cardiac surgery results in a number of problems that should be addressed with method.
In this review, we want to analyze all these key points and all the procedures put in place to counteract the occurrence of NECI and its clinical and socio-economic impact.
Nosocomial Extracardiac Infections
NECI may be of monomicrobial or polimicrobial origin, the latter being only found in less than 27% of cases [9, 15].
An interesting survey on NECI showed that Gram-negative bacteria were involved in 42.4% of cases versus 29.6% of Gram-positive bacteria and 28% of fungi [12]. The most frequently found bacteria among Gram-negative species were Acinetobacter baumannii (8.8%), Pseudomonas aeruginosa (8%), Escherichia coli (5.6%), and Klebsiella pneumoniae (4.8%). Among the Gram-positive bacteria, Staphylococcus aureus (8%), Staphylococcus epidermidis (7.2%), Staphylococcus pneumoniae (4%), and Enterococcus faecium (3.2%) were found. Fungi were so represented: Candida albicans (13.6%), Candida tropicalis (6.4%), Candida parapsilosis (4.8%) and Candida krusei (1.8%) [12].
According to this survey, the rates of NECI vary depending on the type of cardio surgery procedure as follows: 2.6% for congenital malformation repair, 5.5% for valve replacement, 13.6% for coronary artery bypass graft, 16.8% for aortic aneurysm and aortic dissection interventions [12].
A multicenter retrospective cohort study designed for examining the epidemiology, microbiology, and outcome of major postoperative infections, observed that Gram-negative bacteria and Staphylococcus aureus were independently associated with 30-day mortality, whereas coagulase-negative staphylococci were not [9].
These authors selected patients with bloodstream and chest wound infections within 30 days after cardiac surgery, coming to the conclusion that in these two groups, staphylococci were the most represented bacteria (52% of the infections) and S. aureus was the pathogen associated with the highest 30-day mortality [9].
According to a recent study, NECI represent the most important factor favoring mortality of patients undergoing cardiac surgery [16].
Risk Factors
Some studies covering thousands of patients, performed in the USA, Europe, and China [13, 17,18,19,20,21], allowed to obtain predictive models able to individualize the risk estimation and facilitate the clinical decision-making.
These models were based on the identification of modifiable independent risk factors linked to the specific clinical conditions of the patient, such as advanced preoperative anemia, low hematocrit, hypoalbuminemia, age > 60 years, hypertension, smoking history, diabetes, chronic obstructive pulmonary disease, poor cardiac function (NYHA class III-IV), BMI ≥ 24 kg/m2, previous cardiac surgery, cardiopulmonary bypass time > 120 min, peripheral vascular disease, high levels of serum creatinine, blood transfusion [13, 17,18,19,20,21].
Moreover, cardiosurgical patients undergoing extra-corporal circulation may more easily develop colonization and secondary multidrug-resistant (MDR) infection, with increased overall mortality [14].
Other risk factors with a great influence on the clinical outcome in patients subjected to cardiac surgery and affected by NECI are intubation for > 48 h after intervention, the presence of cerebrovascular accidents, and a recent immunosuppressive treatment [9, 14]. Intubation with an OR of 13.4 is one of the most important risk factors for NECI [14].
Previous or prolonged hospitalizations have proven to be at high risk for the development of MDR bacterial infections after heart transplantation [22].
Also, recent antibiotic administration, changing the commensal flora, makes it easier for the development of NECI with more antibiotic-resistant bacteria.
A risk factor stratification is shown in Table 1.
Interestingly, combined surgery, such as concomitant coronary artery bypass graft and/or aortic surgery, was identified as an independent risk factor for postoperative nosocomial pneumonia due to the fact that it is more complicated and time-consuming [13]. Indeed, during bypass, the blood perfusion is assured to the bronchial system but not to the lung that experiences a state of relative ischemia. After the cardiac surgery operation, the reperfusion of the lung may develop ischemia–reperfusion injury mediated by a proinflammatory/proapoptotic state [23]. Generally speaking, a prolonged operation time represents a favorable condition for the contamination of the surgical field.
Furthermore, the type of surgical incision, a long stillness, the choice to use multiple invasive monitoring lines with the possibility of their contamination, the maintenance of urinary catheter, the mechanical ventilation, and the overall hospital stay, play a key role in the development of NECI [15, 24].
Interestingly, a higher mortality rate (32.2%) is observed in patients with infections related to invasive devices in comparison to those without infections (2.9%) [25].
We will be covering here the common causes of NECI that, in order of frequency, are pneumonia, surgical site infection, and urinary tract and bloodstream infections [16].
Postoperative Pneumonia
Epidemiology
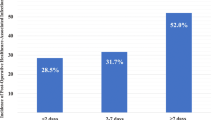
Nosocomial pneumonia is one of the main infective complications after cardiac surgery (1.2–20%) [5, 15, 26, 27] and, especially when ventilator-associated, may lead to serious clinical problems in more than 35% of patients intubated for over 48 h [26].
Furthermore, in patients requiring mechanical ventilation, the time spent in the hospital is surely prolonged, and so, because of all of this, costs are driving up [26].
We must take into account that it causes a significantly higher hospital mortality rate (28% vs 6.2%) and a higher mortality once the follow-up is over (53% vs 19%) [27].
Prevention
According to some authors, patients with more than 2 of ASA (American Society of Anesthesiologists) score are at high risk for developing nosocomial pneumonia following cardiac surgery [15].
To prevent this event, some measures are worth mentioning; it should be recommended the preoperative vaccination against seasonal influenza for all patients and immunization against S. pneumoniae in all patients older than 65 years or younger but affected by chronic diseases of liver, heart, lung, or affected by diabetes and alcoholism [28].
Oral health care that has demonstrated to give benefit in the reduction of ventilator-associated pneumonia [29], may be a valid strategy in these patients before and after cardiac surgery. Second-generation cephalosporins are the antibiotics of choice for an appropriate prophylactic treatment.
The use of prophylactic steroids is controversial, although when combined and time prolonged surgery is planned, it might be useful to reduce the inflammatory cascade due to ischemia/reperfusion injury of the lung [30,31,32]. The emerging antibiotic resistance, an important issue that prolongs hospitalization and consequently increases the costs, can be contained paying attention to avoid unjustified antibiotic treatments, in patients undergoing cardiac surgery, in the days immediately preceding.
An interesting meta-analysis in patients after cardiac surgery has demonstrated the important role of non-invasive ventilation, compared to invasive, to reduce the risk of endotracheal intubation and of hospital mortality and to protect versus major clinical complications [33].
Other simple rationale measures should be adopted such as that of keeping the head of the bed raised, or motivating the patient to take the sitting position leaving the bed for the chair (at least during the meal) or favoring his deambulation once discharged from the anesthesia care unit. Not less important, it is also to push the patient to have deep breathing and use incentive spirometry [33].
Moreover, the placement of a nasogastric tube and the excessive administration of blood and platelet transfusion have to be avoided.
Indeed, patients receiving blood transfusion have an increased risk of 29% of developing major infection when each red blood cell unit is transfused [34].
Moreover, an increased risk of pneumonia of 3.4-fold is reported in postoperative patients receiving blood transfusion [35]; interestingly, the mechanism through which adverse outcomes, such as pneumonia, occur, in patients undergoing cardiac surgery, concerns the blunting of postoperative factor-1 alpha (HIF-1α) response after blood transfusion [36].
All of this strongly suggests to use a restrictive transfusion strategy after cardiac surgery, when possible, to decrease nosocomial pneumonia [37].
Microbiology
Some authors found in Enterobacteriaceae (32.8%), P. aeruginosa (28.6%), and S. aureus (27.1%) the main types of microorganisms responsible for nosocomial pneumonia following cardiac surgery [18]. In a retrospective study, except for a lower percentage of methicillin-susceptible S. aureus found in non-ventilator compared to ventilator pneumonia, the percentage of causative agents isolated in both groups was comparable [Enterobacteriaceae (35%), P. aeruginosa (20.2%), and Haemophilus spp. (20.2%)] [38]. Other authors observed that Acinetobacter baumannii (39% of cases) and Pseudomonas aeruginosa (22.5% of cases) [39] were the most common pathogens. Others emphasized the role played by P. aeruginosa, K. pneumoniae, and Enterobacter cloacae as the bacteria most often involved in nosocomial pneumonia [26], while still others found in Haemophilus influenzae the most commonly isolated microorganism [15, 40].
Fungi such as C. albicans, even if more rarely, are described to play a role especially in patients with unhealthy nutrition, diabetes, or subjected to a prolonged use of extended-spectrum antibiotics.
This different prevalence of the causative agents of nosocomial pneumonia following cardiac surgery in diverse hospitals might be linked to the lack of uniform preventive strategy and also to different monitoring and surveillance programs of health-related infections and antibiotic resistance.
Finally, in this pandemic era, several viral postoperative cases of pneumonia have been ascribed to COVID-19 in patients that resulted RT-PCR test negative before cardiac surgery; immunologic disorders by the use of extracorporeal circulation, physiologic distress, and anesthesia would be responsible for COVID-19 activation during the incubation period [41].
The right choice of the initial empirical antibiotic treatment in patients with nosocomial pneumonia is of the utmost importance in order to avoid a future occurrence of antimicrobial resistance towards the more virulent pathogens such as A. baumannii, P. aeruginosa, or K. pneumoniae, able to cause clinical conditions extremely uneasy to cure and potentially fatal [42,43,44].
Diagnosis
The following clinical signs: dyspnea, onset of cough, change in the character of the sputum or purulent secretions, desaturation, fever (> 38 ℃) without other apparent causes, leukocytosis, (> 12,000 cells/µl) or leukopenia (< 4000 cells/µl), elevated serum levels of C-reactive protein, and erythrocyte sedimentation rate, are highly suggestive for the diagnosis of pneumonia. The finding of progressive pulmonary infiltrates on chest radiography or computed tomography (CT) patently confirms the clinical diagnosis.
The most insidious ventilator-associated pneumonia takes advantage of the following diagnostic criteria which can be summarized as a worsening in respiratory dynamics after a period of stability or improvement, and in laboratory evidence of respiratory infection [45, 46]:
-
1.
A sustained increase in the daily minimum positive end-expiratory pressure (PEEP) of ≥ 3 cmH2O following a period of stability or improvement on the ventilator.
-
2.
A sustained increase in the daily minimum FiO2 of ≥ 20% following a period of stability or improvement on the ventilator.
-
3.
Bacterial isolation through semiquantitative cultures from endotracheal aspiration or bronchoalveolar lavage of lower respiratory tract secretions (sensitivity of 71.1% and specificity of 79.6%), lung tissue, protected specimen brush; the presence of purulent respiratory secretions (from the lungs, bronchi, or trachea containing ≥ 25 neutrophils and ≤ 10 squamous epithelial cells per low power field) represent additional diagnostic means.
-
4.
Pathogen identification in pleural fluid (obtained during thoracentesis or within 24 h of chest tube placement).
-
5.
Lung parenchyma evidence of abscess formation or invasion by fungi or positive immunohistochemical assays, cytology, or microscopy performed on lung tissue for viral pathogens.
-
6.
Positive test for Legionella species
-
7.
Positive diagnostic test on respiratory secretions for viral pathogens
Management
Postoperative pneumonia requires to be treated as a hospital-acquired pneumonia with a careful look both to the causative agents and to the antibiotic resistance patterns most frequently detected.
The use of appropriate and early empiric antibiotic therapy significantly decreases the mortality, while delay in starting the treatment is associated with poor outcomes [38].
The treatment should consist of a broad-spectrum beta-lactam antibiotic (piperacillin/tazobactam) or carbapenems targeting Gram-negative bacilli; in the case of ventilator-associated pneumonia, the antibiotic choice should be directed against S. aureus or methicillin-resistant S. Aureus (MRSA), using vancomycin, teicoplanin, or daptomycin [38]. Due to multidrug-resistant (86% resistance to imipenem and 62% resistance to piperacillin‑tazobactam), patients with critical infection caused by A. baumannii, should be treated with a therapy based on colistin/tigecycline also combined with other antibiotics such as carbapenems, sulbactams, fluoroquinolones, or minocycline [24, 47].
Surgical Site Infection
Epidemiology
A surgical site infection starts when the bacterial contamination exceeds the host defense.
system. In the majority of the cases, it is classified as superficial infection, and with an incidence ranging between 1.4 and 17 l%, it covers 1/6–1/7 of all NECI [48,49,50]; however, in the 0.5–5% of cardiac surgery procedures, the wound infection may become deep in the sternal surgical site and sometimes is able to involve also sternal bones and mediastinal space. This latter dangerous variant, termed mediastinitis, is a serious life-threatening complication of the deep surgical site infection, defined as a deep sternal wound infection with sternal osteomyelitis with or without infected retrosternal space. It may cause sepsis, with multisystem organ failure [51], may also affect the bone, inducing sternal osteomyelitis [52, 53], and is characterized by a high morbidity and mortality (increased 1-year mortality of 10.7% vs 2.5% in patients without) [54,55,56,57].
Prevention
The reduction of this type of infection has been obtained in England by means of a care pathway model based on the control practices of the surgical site by a multidisciplinary team [48] with different roles and tasks.
-
Some team members should care for the preoperative management of the patients giving them exhaustive information leaflets containing all explanations to change their habits (smoke cessation at least 30 days before cardiac surgery for smokers, encouragement to lose weight for obese or overweight patients, eradication of S. aureus in nasal carriers with topical mupirocin treatment for 5 days) and for preoperative skin preparation and postoperative wound care;
-
Others should control the body temperature in the perioperative period with the aim to avoid hypothermia;
-
Still, others should care for patient education to become actively involved in his healing process throughout the postoperative course (patient collaboration, where possibile, is crucial to prevent NECI and obtain quick clinical improvements);
-
Others, finally, should deal with the continuous monitoring of the incidence of surgical site infection that is the best standard of surveillance, since it provides overall information on incidence rate, microbiological trend, and antibiotic resistance [58].
Different opinions exist among centers on the means used to remove the hairs; according to some authors, depilatory creams should be safer than other depilatory means by lowering the hypersensitivity reactions, whereas others believe that it is not the case [59, 60].
Importantly, there is agreement on the fact that the surgical site infection is less likely when the hairs are removed on the day of surgery rather than the day before [61].
Then, it is strongly recommended the use of chlorhexidine gluconate for skin decolonization followed by a new addition of 2% chlorhexidine gluconate in 70% alcohol immediately before skin incision [48].
Remarkable is also the choice of the right time for giving the antibiotic prophylaxis (preferentially cephalosporins in patients at low risk of MRSA colonization) that should be administered within 60 min from surgical incision [62]; indeed, the first few hours after bacterial contamination are most likely to cause an infection [59]. In this context, it should be recalled that the administration of cefazolin or cefuroxime should be repeated, due to short half-lives, besides procedures lasting more than 4 h or when there is a prolonged or excessive bleeding [62]. On the other hand, vancomycin should be administered in patients with proven or at high risk for MRSA colonization or in patients with IgE-mediated reactions to beta-lactams, together with aminoglycoside for Gram-negative coverage [62].
Important also is the control of temperature, glycemia, and oxygenation [59].
It is known that hypothermia causes vasoconstriction that, in turn, lowers the oxygen tension, both thus favoring the occurrence of infection in the surgical site.
According to a recent meta-analysis, active warming methods to keep a good temperature, are recommended, although it is unclear if they can really prevent the infection of the surgical site [63].
It is equally important the maintenance of the glycemic stability; indeed, systematic reviews of several studies investigating control protocols (through the use of continuous insulin infusion) to maintain an optimal range of glycemia (< 140 mg/dl or 7.8 mmol/L), demonstrated fewer potential complications in patients with diabetes undergoing cardiac surgery [64, 65].
Microbiology
A high bacterial count, estimated at about 105 microorganisms per gram of tissue, is needed to induce the development of surgical site infection.
Gram-positive bacteria have long been considered the commonest microorganisms (89%) in surgical site infections following cardiac surgery, while Gram-negative bacteria are the causative agents only in 10% of cases [9]; however, recent findings give evidence of changes in microbiology with an increased role of Gram-negative bacteria (24.5% of cases) and a relative lower role of Gram-positive bacteria (75.5% of cases) [66].
Among Gram-positive bacteria, coagulase-negative staphylococci are most frequently isolated (56% of cases) while S. aureus is found in 24% [9, 57]; some of them may develop antibiotic resistance [58].
Staphylococcus epidermidis and the other endogenous bacterial flora of the skin have to be classified as potential pathogens causing contamination after skin incision and developing multi-resistance antibiotic spectrum requiring extended antibiotic therapy [59, 67].
Diagnosis
In front of clinical signs such as cellulitis and wound discharge, dehiscence, tenderness, and sternal instability, as well as systemic inflammatory findings (elevated C-reactive protein, erythrocyte sedimentation rate, and white blood cells) at times accompanied by tachycardia and hypotension, the likelihood of a deep infection is high and a quick management is needed.
At least one of these criteria must be present to make certain the diagnosis [54]:
-
1.
Deep incision dehiscence, spontaneous or opened or aspirated by a surgeon, or organism culture identification performed for clinical diagnosis or treatment;
-
2.
Hypothermia or fever (> 38 °C), chest pain or tenderness or sternal instability, and concurrent purulent discharge or positive microbiological culture;
-
3.
Gross anatomical or histopathologic exam, or imaging test showing the presence of abscess or deep infection.
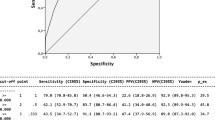
To confirm the presence of mediastinitis and properly handle any problem, both blood cultures and CT scan are strongly recommended, thanks to their ability to determine the causative agent, the former, and to evaluate the widening of the mediastinum, potential presence of mediastinal air–fluid levels, pneumomediastinum, and pleural effusion, the latter. [56, 57]. Magnetic resonance imaging may be useful when diagnosis of osteomyelitis is uncertain, or to evaluate for concomitant soft tissue abscess; the presence of a low T1 signal (compared to the T1 signal of the skeletal muscle) and a high signal on fluid-sensitive images, with post-contrast enhancement, are highly specific and suggestive (95.6% sensitivity and 80.7% specificity) [68, 69]. Also, single-photon emission computed tomography (85.1% sensitivity and 92.7% specificity) and positron emission tomography (95% sensitivity, 82% specificity) have a high diagnostic accuracy and may play an important role especially in helping ensure an adequate debridement thanks to the localization of the disease sites [57, 69].
Management
For an adequate management of this complication, particularly welcome is the involvement of a multidisciplinary team of cardiothoracic and plastic surgeons, infectivologists, microbiologists, and intensive care physicians [57]. They can set the most correct management planning an early and proper debridement and suggest a targeted antibiotic therapy [57]. Some sort of deal exists between various authors on the safety and efficacy of a short course of treatment for uncomplicated bacterial infections and of a longer course for deep surgical site infections with the clear purpose to control more closely the clinical response and biomarkers [70].
In the absence of bacterial isolation, an empirical antibiotic therapy against the commonest bacteria isolated in that hospital should be started focusing on the use of piperacillin/tazobactam, imipenem, or meropenem when Gram-negative bacteria are prevalent and MRSA are rare and vancomycin, teicoplanin, or daptomycin in presence of a high prevalence of MRSA [57]. Indeed, resistance of staphylococci to amoxicillin + clavulanate combination was reported in 43% of cases and to linezolid in 77% but high sensitivity to vancomycin and teicoplanin was observed [24].
A strong consensus is found on the use of long-acting lipoglycopeptide antibiotics in patients with MRSA infection such as dalbavancin and oritavancin since they have long half-lives and a single dose covers the entire antimicrobial course, improving adherence and avoiding the need for daily treatments [70].
Urinary Tract Infection
Epidemiology
With an incidence rate ranging from 1.1 to 8% in the adults [12, 16, 71] and 7% in the children [71], the urinary tract infection is the third commonest cause of NECI.
Since urinary catheters are associated with a 3–10% of bacteriuria and a 10–25% risk of infection, patients in need of long-term urinary catheterization are more likely to develop infection [16, 72].
Moreover, a significantly higher mortality rate was found in patients with catheter-associated urinary tract infection than in patients without (10.9% vs. 3.2%) [73].
Prevention
The most risky situation for the development of future urinary tract infections, with an odds ratio (OR) of 7.9, is that which provides the catheter insertion in the ward, followed by the placement of the catheter in the cystoscopy room (OR 3.52), emergency department (OR 2.9), and operating room (OR 1) [74]. Diabetes mellitus also with an OR of 2.04 is one of the most important and manageable risk factors manageable [73].
A reduction of incidence of urinary tract infection is made possible by adopting a few measures such as application of a checklist and training packages for a proper urinary catheter insertion (hand hygiene with 2% chlorhexidine, connection of the collection bag to the catheter before its insertion) [75], teach a group of nurses to remove nonessential urinary catheters [76, 77]. Since a period of urinary catheterization of more than 4 days significantly increases the risk of infection [74], if possible, it would be appropriate to remove the catheters before.
Microbiology
In a single center study, the most prevalent pathogens isolated in children after cardiac surgery were K. pneumoniae (24%), E. coli (21%), Pseudomonas (14%), E. faecium (14%), C. albicans (14%), and E. cloacae (10%) [72]. Another study on adult patients highlighted that the commonest agents were in 73.4% bacteria (E. cloacae and E.coli) and in 26.6% fungi (C.albicans) [73]. Still another study showed that E. coli was the most frequently isolated bacterium (37% of cases) [24].
Diagnosis
The main accompanying symptoms of urinary tract infection after cardiac surgery are fever, leukocytosis or leukopenia, vomiting, dyspnea or apnea, and bradycardia or tachycardia. In these patients, the presence of a positive urine culture (with > 10.000 colony-forming units per milliliter of no more than two different species collected in an aseptic technique, 48 h after the intervention) is sufficient for the diagnosis. In asymptomatic patients, the diagnosis is certain when a positive urine culture with > 100,000 colony-forming units per milliliter is present [78].
Management
According to some authors, the empirical treatment of the catheter-associated urinary tract infections should be reserved for emergency situations, while for all others, you have to wait for the antibiogram [74].
Knowledge of local prevalence of antibiotic-resistant bacteria is also an important consideration to choose the most appropriate antibiotic. Indeed, some studies found high resistance of E. coli to amoxicillin–clavulanate, amikacin, ciprofloxacin, and cefotaxime [24, 79].
The antimicrobial therapy should be given for 7 days in patients with catheter-associated urinary tract infection, prolonged to 14 days after a clinical response fails.
Bloodstream Infection
Epidemiology
The overall incidence of bloodstream infection is estimated to be approximately 2.6–3.4% proving to be the fourth commonest cause of NECI with a crude mortality rate of 33.3% [16, 80].
Immunosuppressed and malnourished patients and those with devices have a high risk of developing bloodstream infection [47].
In a prospective study, bacteremia originated in 27.6% from an identifiable source and in 16.4% from catheter, while 56% of the cases remained unknown [80].
Conflicting results exist about the incidence rate of the infections related to the central venous catheter with percentages ranging between 1 and 25% [10, 24, 81, 82].
S. aureus bloodstream infection has an incidence of 0.57% in patients undergoing cardiac surgery and its outbreak is more common after this procedure than after others (orthopedic, neurologic, and plastic surgery) [83]. A prospective randomized study showed that bacteremia from E. faecalis, Enterobacter spp., and Acinetobacter occurs in 3% of catheter insertions while catheter colonization is present in 24% of cases [84].
A clinical investigation showed that Gram-positive cocci (Staphylococcus and Enterococcus) were the most common causative agents in bloodstream infections [47], whereas in a retrospective study, Pseudomonas was the leading isolated bacteria [24].
A retrospective multicenter study demonstrated that both high New York Heart Association class III or IV and previous broad-spectrum antibiotic therapy (carbapenems and fluoroquinolones) were independent predictors of candidemia in cardiac surgery patients with prolonged postoperative stay in the intensive care unit [85]. The incidence of candidemia in these patients was 0.2%, and 65% of cases were caused by C. albicans, while only 14 and 9% by C. parapsilosis and C. glabrata, respectively [85].
Prevention
An active surveillance system of hospital surgical personnel in order to identify nasal carriers of S. aureus and proceed to its eradication is desirable since it would allow to monitor and control outbreaks of staphylococcal infection, hence minimizing its hospital incidence [86, 87]. This program should be extended to patients undergoing cardiac surgery, who are carriers of S aureus, by giving them topical mupirocin treatment for 5 days, a solution that could help decrease the incidence of staphylococcal bloodstream infection.
As for the prevention of catheter-related bloodstream infection, a good hand hygiene and an appropriate aseptic technique before inserting the catheter are recommended, as well as skin disinfection using 2% chlorhexidine (CHG)–alcohol [88, 89]. Moreover, when it is possible, it would be preferable to use a single-lumen than a multilumen central venous catheter due to a lower risk of infection [90].
Finally, as demonstrated in a multicenter randomized controlled study comparing all types of catheters, the femoral site of insertion should not be the first choice site since colonization occurs most frequently here than anywhere else [91]; instead, the preferential choice site for central catheter insertion should be that of the subclavian vein and the ultrasound guidance is recommended to reduce the number of attempts for cannulation and the resulting mechanical complications [89].
Since the intense and prolonged use of broad-spectrum antibiotics is an independent predictor of candidemia in cardiac surgery patients with prolonged postoperative stay in the intensive care unit [84], extensive antimicrobial treatments should be avoided, unless absolutely necessary, in patients candidates for cardiac surgery in the days before the operation.
Microbiology
Migration of skin organisms at the insertion site into the cutaneous catheter tract with colonization of the catheter tip is the most common route of infection.
A prospective cohort study in children undergoing cardiac surgery showed that bloodstream infection was due to Gram-negative bacteria in 67% of cases, Gram-positive in 26%. and fungi in only 7% [92].
Among Gram-negative bacteria, the most prevalent were Pseudomonas (28%), Enterobacter (22%), and Klebsiella (11%), while Gram-positive bacteria were represented by coagulase-negative Staphylococcus (86%) and MRSA (14%) [92].
On the contrary, according to a prospective study, in adult patients, the leading causative agents of bloodstream infection following cardiac surgery were staphylococci (37.7%) [80].
Diagnosis
An early diagnosis of bloodstream infection is of paramount importance since the isolation of the causative agent allows to choose a specific antibiotic therapy [93].
Established diagnostic tools are the blood and intravascular cannula tip cultures methods; other modalities based on nucleic acid amplification technologies to identify the causative agent are promising but not-standardized and expensive.
Among the biomarkers to diagnose the sepsis, the only one with a some specificity for the infections and a great accuracy to detect a severe inflammatory state is procalcitonin (PCT). The serum levels of PCT, a peptide, derived from the parafollicular cells of the thyroid and from the neuroendocrine cells of the lung and the bowel, are undetectable in healthy subjects and very high in those with bacterial infections [94]. This promises to be a valuable biomarker to distinguish between bacterial infection and systemic inflammatory response syndrome [95].
Management
The timing of an early and proper antibiotic treatment increases the probabilities of survival and prevents the development of septic shock [94]; for a correct management and to set up an effective treatment we should be aware of:
-
The source of infection;
-
The prevalence and susceptibility of various pathogens in that hospital;
-
The patient’s clinical conditions.
If infection is suspected, it is recommended to remove the central catheter as soon as possible [47].
A broader antibiotic coverage represents the first choice until the pathogen is isolated and the treatment can be more specific based on the antibiogram [94]. Due to high resistance rate to methicillin (87% of cases) and fluoroquinolones and clindamycin (66% and 55%, respectively), the administration of vancomycin, linezolid, and daptomycin should be preferred against Gram-positive bacteria [47].
Instead, the fungal infection of the blood responds to treatment with fluconazole and voriconazole but echinocandins are needed for definite and severe fungal infections [47].
The optimization of the antibiotic therapy is crucial and requires a careful assessment that should be made by a multidisciplinary team of cardiothoracic surgeons, infectivologists, and intensive care physicians especially in patients undergoing extracorporeal interventions. Indeed, the use of any extracorporeal membrane oxygenation (ECMO) and/or renal replacement therapy (RRT), increasing the volume of distribution of protein-bound and/or lipophilic antibiotics, changes the patient drug exposure, leading to therapeutic failure or antimicrobial toxicity [96]. The use of therapeutic drug monitoring might be a way to ensure that antimicrobials are given to the proper therapeutic dosage; unfortunately, this antimicrobial plasma concentration might not match the concentration at the site of infection since it is influenced by a number of factors and might not be an accurate measure of the protein unbound concentration. Therefore, the final decision on the increase or reduction of the antibiotic dosage is a challenge for the infectivologists who must give consideration to the advice above [96].
Costs
A number of studies [6, 12, 97,98,99] have analyzed the cost aspects of NECI; the increased utilization of specific hospital resources prolongs the hospitalization time also because of the occurrence of other noninfectious complications and raises the problem of the readmissions. It is estimated that NECI increase the hospitalization time up to about 2 weeks with a cost increase by about 60% [12].
In the USA, the median cost of patients affected by NECI was $59,300 vs $37,600 in patients without infection with an incremental increase of $23,000 (95% CI, $20,900 to $25,200) [6].
This cost analysis depended on the type of infection and was as follows: $24,500 (95% CI, $23,100 to $26,000) for pulmonary infections and $8300 (95% CI, $7500 to $9100) for urinary infections [6].
Pulmonary infections lead to an overall annual cost burden estimated at $121.8 million (95% CI, $102.2 to $142.9 million) [6]. In England, the estimated cost per patient undergoing cardiac surgery for treating ventilator-associated pneumonia is £8829 [40].
Instead, the cost of the infection of the surgical site was estimated at £17,000 for patients in England and $62,773 in the USA, when these infections get complicated with mediastinitis [45, 98, 99].
A separate discussion deserves the clinical impact of the multidrug-resistant that worsens the length of hospital stay with additional costs estimated in Italy at 11,549 euros per patient [100].
Since NECI, as we have seen, greatly increase the costs, various authors came to the conclusion that a reduction of them is an economic necessity.
They, strongly suggest to find preventive interventions or corrective measures to diminish the burden of NECI, improve patient outcomes and thus reduce the costs [97,98,99,100,101,102,103].
Conclusions
Usually, after cardiac surgery, the cardiac complications receive more attention than other clinical situations, with the clear risk to neglect the possible onset of NECI until the infection becomes grave and manifest.
We wanted to underline that NECI represent an important public health issue associated with a greater perioperative morbidity and mortality; they increase the resource utilization because of a longer hospitalization time and create excess costs. As a number of cases could be potentially preventable, it is our duty that NECI receive all the attention and care mentioned above. There is certainly a need to establish an effective antimicrobial stewardship to address the challenges we are facing every day to reduce the number of MDR bacteria, adopting conscious decisions on the best antibiotic choice, dosage, and treatment duration.
BMI, body mass index; CABG, coronary artery bypass graft; CLD, chronic liver disease; COPD, chronic obstructive pulmonary disease; CVC, central venous catheter; NECI, nosocomial extracardiac infections; NYHA, New York Heart Association; OR, odds ratio.
Change history
01 December 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11908-022-00792-3
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hrdlicka CM, Wang J, Selim M. Neurological complications of cardiac procedures. Semin Neurol. 2021;41(4):398–410.
Maranta F, Cianfanelli L, Grippo R, Alfieri O, Cianflone D, Imazio M. Post-pericardiotomy syndrome: insights into neglected postoperative issues. Eur J Cardiothorac Surg. 2021:ezab449.
Silva TFD, Silva KRDC, Nepomuceno CM, Corrêa CSM, Godoy JPM, Santos ATLD, et al. Incidence of acute kidney injury post cardiac surgery: a comparison of the AKIN and KDIGO criteria. Braz J Anesthesiol. 2021;71(5):511–516.
Harrogate SR, Cooper JA, Zawadka M, Anwar S. Seven-year follow-up of persistent postsurgical pain in cardiac surgery patients: a prospective observational study of prevalence and risk factors. Eur J Pain. 2021;25(8):1829–38.
Pahwa S, Bernabei A, Schaff H, Stulak J, Greason K, Pochettino A, et al. Impact of postoperative complications after cardiac surgery on long-term survival. J Card Surg. 2021;36(6):2045–52.
• Hadaya J, Downey P, Tran Z, Sanaiha Y, Verma A, Shemin RJ, et al. Impact of Postoperative Infections on Readmission and Resource Use in Elective Cardiac Surgery. Ann Thorac Surg. 2021;S0003–4975(21):00705. An extensive and comprehensive study providing the impact of postoperative infections on costs and existing variation in cardiac surgical care in the United States.
Beckmann A, Meyer R, Lewandowski J, Markewitz A, Gummert J. German Heart Surgery Report 2020: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular Surgery. Thorac Cardiovasc Surg. 2021;69(4):294–307.
Gelijns AC, Moskowitz AJ, Acker MA, et al. Management practices and major infections after cardiac surgery. J Am Coll Cardiol. 2014;64:372–81.
Chen LF, Arduino JM, Sheng S, Muhlbaier LH, Kanafani ZA, Harris AD, et al. Epidemiology and outcome of major postoperative infections following cardiac surgery: risk factors and impact of pathogen type. Am J Infect Control. 2012;40(10):963–8.
Michalopoulos A, Geroulanos S, Rosmarakis ES, Falagas ME. Frequency, characteristics, and predictors of microbiologically documented nosocomial infections after cardiac surgery. Eur J Cardiothorac Surg. 2006;29:456–60.
Kelava M, Robich M, Houghtaling PL, Sabik JF 3rd, Gordon S, Mihaljevic T, et al. Hospitalization before surgery increases risk for postoperative infections. J Thorac Cardiovasc Surg. 2014;148(4):1615–21.
Jiang WL, Hu XP, Hu ZP, Tang Z, Wu HB, Chen LH, et al. Morbidity and mortality of nosocomial infection after cardiovascular surgery: a report of 1606 cases. Curr Med Sci. 2018;38(2):329–35.
Wang DS, Huang XF, Wang HF, Le S, Du XL. Clinical risk score for postoperative pneumonia following heart valve surgery. Chin Med J (Engl). 2021;134(20):2447–56.
Massart N, Mansour A, Ross JT, Piau C, Verhoye JP, Tattevin P, et al. Mortality due to hospital-acquired infection after cardiac surgery. J Thorac Cardiovasc Surg. 2020;S0022–5223(20):32486–7.
Alsulami OA, Konkar AE, Alalyani AA, Alghamdi MS, Eid SM, Alsulami HA, et al. Postoperative pneumonia following open heart surgery. Cureus. 2020;12(9).
de la Varga-Martínez O, Gómez-Sánchez E, Muñoz MF, Lorenzo M, Gómez-Pesquera E, Poves-Álvarez R, et al. Impact of nosocomial infections on patient mortality following cardiac surgery. J Clin Anesth. 2021;69.
•• Wang D, Huang X, Wang H, Le S, Yang H, Wang F, et al. Risk factors for postoperative pneumonia after cardiac surgery: a prediction model. J Thorac Dis. 2021;13(4):2351–2362. An interesting retrospective, observational study providing information on risk factors and types of bacteria involved in postoperative pneumonia after cardiac surgery.
Hortal J, Giannella M, Perez MJ, et al. Incidence and risk factors for ventilator-associated pneumonia after major heart surgery. Intensive Care Med. 2009;35:1518–25. https://doi.org/10.1007/s00134-009-1523-3.
Kinlin LM, Kirchner C, Zhang H, et al. Derivation and validation of a clinical prediction rule for nosocomial pneumonia after coronary artery bypass graft surgery. Clin Infect Dis. 2010;50:493–501. https://doi.org/10.1086/649925.
Kilic A, Ohkuma R, Grimm JC, et al. A novel score to estimate the risk of pneumonia after cardiac surgery. J Thorac Cardiovasc Surg. 2016;151:1415–20.
Strobel RJ, Liang Q, Zhang M, et al. A preoperative risk model for postoperative pneumonia after coronary artery bypass grafting. Ann Thorac Surg. 2016;102:1213–9.
•• Karruli A, de Cristofaro J, Andini R, Iossa D, Bernardo M, Amarelli C, et al. Risk Factors and Outcome of Multidrug-Resistant Infections after Heart Transplant: A Contemporary Single Center Experience. Microorganisms. 2021;9(6):1210. A retrospective, observational study on risk factors, prevalence, prevention, and outcome of multidrug-resistant infections in patients who underwent heart transplantation.
Ng CS, Wan S, Arifi AA, Yim AP. Inflammatory response to pulmonary ischemia-reperfusion injury. Surg Today. 2006;36(3):205–14.
Sahu MK, Siddharth B, Choudhury A, Vishnubhatla S, Singh SP, Menon R, et al. Incidence, microbiological profile of nosocomial infections, and their antibiotic resistance patterns in a high volume cardiac surgical intensive care unit. Ann Card Anaesth. 2016;19(2):281–7.
Álvarez Lerma F, Carrasco M, Otal JJ, Palomar M, Olaechea P, Peris X, et al. Grupo de Estudio ENVIN-HELICS. Invasive device-related infections after heart surgery. Med Intensiva. 2013;37(9):584–92.
Tanner TG, Colvin MO. Pulmonary complications of cardiac surgery. Lung. 2020;198(6):889–96.
Ibañez J, Riera M, Amezaga R, Herrero J, Colomar A, Campillo-Artero C, et al. Long-term mortality after pneumonia in cardiac surgery patients: a propensity-matched analysis. J Intensive Care Med. 2016;31(1):34–40.
Martin TJ, Eltorai AEM, Kennedy K, Sellke F, Ehsan A. Seasonality of postoperative pneumonia after coronary artery bypass grafting: a national inpatient sample study. J Card Surg. 2020;35(6):1258–66.
Winning L, Lundy FT, Blackwood B, McAuley DF, El Karim I. Oral health care for the critically ill: a narrative review. Crit Care. 2021;25(1):353.
Cappabianca G, Rotunno C, de Luca Tupputi Schinosa L, Ranieri VM, Paparella D. Protective effects of steroids in cardiac surgery: a meta-analysis of randomized double-blind trials. J Cardiothorac Vasc Anesth. 2011;25(1):156–65.
Akhtar MI, Gautel L, Lomivorotov V, Neto CN, Vives M, El Tahan MR, et al. Multicenter international survey on cardiopulmonary bypass perfusion practices in adult cardiac surgery. J Cardiothorac Vasc Anesth. 2021;35(4):1115–24.
Whitlock RP, Dieleman JM, Belley-Cote E, Vincent J, Zhang M, Devereaux PJ, et al. The effect of steroids in patients undergoing cardiopulmonary bypass: an individual patient meta-analysis of two randomized trials. J Cardiothorac Vasc Anesth. 2020;34(1):99–105.
Zhu G, Huang Y, Wei D, Shi Y. Efficacy and safety of noninvasive ventilation in patients after cardiothoracic surgery: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2016;95(38).
Horvath KA, Acker MA, Chang H, Bagiella E, Smith PK, Iribarne A, et al. Blood transfusion and infection after cardiac surgery. Ann Thorac Surg. 2013;95(6):2194–201.
Likosky DS, Paone G, Zhang M, Rogers MA, Harrington SD, Theurer PF, et al. Michigan society of thoracic and cardiovascular surgeons quality collaborative. Red blood cell transfusions impact pneumonia rates after coronary artery bypass grafting. Ann Thorac Surg. 2015;100(3):794–800.
Viikinkoski E, Jalkanen J, Gunn J, Vasankari T, Lehto J, Valtonen M, et al. Red blood cell transfusion induces abnormal HIF-1α response to cytokine storm after adult cardiac surgery. Sci Rep. 2021;11(1):22230.
LaPar DJ, Crosby IK, Ailawadi G, Ad N, Choi E, Spiess BD, et al. Investigators for the virginia cardiac surgery quality initiative. Blood product conservation is associated with improved outcomes and reduced costs after cardiac surgery. J Thorac Cardiovasc Surg. 2013;145(3):796–803.
Allou N, Allyn J, Snauwaert A, Welsch C, Lucet JC, Kortbaoui R, et al. Postoperative pneumonia following cardiac surgery in non-ventilated patients versus mechanically ventilated patients: is there any difference? Crit Care. 2015;19(1):116.
Hamidi AA, Kescioglu S. Identification of factors affecting mortality in late-onset ventilator-associated pneumonia. Eurasian J Med. 2020;52(3):254–8.
Luckraz H, Manga N, Senanayake EL, Abdelaziz M, Gopal S, Charman SC, et al. Cost of treating ventilator-associated pneumonia post cardiac surgery in the National Health Service: results from a propensity-matched cohort study. J Intensive Care Soc. 2018;19(2):94–100.
Uysal A, Erturk E, Abacilar AF, Duman U, Dogan OF. The outcomes of patients incidentally confirmed with COVID-19 after cardiac surgery. Heart Surg Forum. 2021;24(6):E940–6.
Almomani BA, McCullough A, Gharaibeh R, Samrah S, Mahasneh F. Incidence and predictors of 14-day mortality in multidrug-resistant Acinetobacter baumannii in ventilator-associated pneumonia. J Infect Dev Ctries. 2015;9(12):1323–30.
Ding C, Yang Z, Wang J, Liu X, Cao Y, Pan Y, et al. Prevalence of Pseudomonas aeruginosa and antimicrobial-resistant Pseudomonas aeruginosa in patients with pneumonia in mainland China: a systematic review and meta-analysis. Int J Infect Dis. 2016;49:119–28.
Man MY, Shum HP, Li KC, Yan WW. Impact of appropriate empirical antibiotics on clinical outcomes in Klebsiella pneumoniae bacteraemia. Hong Kong Med J. 2021;27(4):247–57.
Klompas M, Magill S, Robicsek A, Strymish JM, Kleinman K, Evans RS, et al. CDC Prevention Epicenters Program. Objective surveillance definitions for ventilator-associated pneumonia. Crit Care Med. 2012;40(12):3154–61.
Al-Omari B, McMeekin P, Allen AJ, Akram AR, Graziadio S, Suklan J, et al. Systematic review of studies investigating ventilator associated pneumonia diagnostics in intensive care. BMC Pulm Med. 2021;21(1):196.
• Liu Z, Zhang X, Zhai Q. Clinical investigation of nosocomial infections in adult patients after cardiac surgery. Medicine (Baltimore). 2021;100(4):e24162. An important retrospective study providing the characteristics of the distribution of pathogens, antibiotic resistance, and independent risk factors for nosocomial infections in patients after open-heart surgery and giving some suggestions for clinical practice.
Chiwera L, Wigglesworth N, McCoskery C, Lucchese G, Newsholme W. Reducing adult cardiac surgical site infections and the economic impact of using multidisciplinary collaboration. J Hosp Infect. 2018;100(4):428–36.
• Martinez-Sobalvarro JV, Júnior AAP, Pereira LB, Baldoni AO, Ceron CS, Dos Reis TM. Antimicrobial stewardship for surgical antibiotic prophylaxis and surgical site infections: a systematic review. Int J Clin Pharm. 2021. https://doi.org/10.1007/s11096-021-01358-4. A comprehensive and extensive systematic review of randomized and non-randomized clinical trials on the effectiveness of antimicrobial stewardship in promoting adherence to surgical antibiotic prophylaxis protocols in hospitalized patients.
Taylor AH, Mitchell AE, Mitchell IM. A 15-year study of the changing demographics and infection risk in a new UK cardiac surgery unit. Interact Cardiovasc Thorac Surg. 2012;15(3):390–4.
Chan M, Yusuf E, Giulieri S, Perrottet N, Von Segesser L, Borens O, et al. A retrospective study of deep sternal wound infections: clinical and microbiological characteristics, treatment, and risk factors for complications. Diagn Microbiol Infect Dis. 2016;84(3):261–5.
Chin YT, Krishnan M, Burns P, Qamruddin A, Hasan R, Dodgson AR. Brucella melitensis sternal osteomyelitis following median sternotomy. J Infect Chemother. 2014;20(9):574–6.
Abboud CS, Miglioli L, Romero AP, Ibanes AS, Della Togna D, Pereira RC, et al. First report of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae sternum osteomyelitis relapsing 6 years after mediastinitis following cardiac surgery. Int J Antimicrob Agents. 2017;49(2):262–263.
Inui T, Bandyk DF. Vascular surgical site infection: risk factors and preventive measures. Semin Vasc Surg. 2015;28(3–4):201–7.
El Oakley RM, Wright JE. Postoperative mediastinitis: classification and management. Ann Thorac Surg. 1996;61:1030–6.
Bouza E, de Alarcón A, Fariñas MC, Gálvez J, Goenaga MÁ, Gutiérrez-Díez F, et al. Prevention, diagnosis and management of post-surgical mediastinitis in adults consensus guidelines of the Spanish Society of Cardiovascular Infections (SEICAV), the Spanish Society of Thoracic and Cardiovascular Surgery (SECTCV) and the Biomedical Research Centre Network for Respiratory Diseases (CIBERES). J Clin Med. 2021;10(23):5566.
Yusuf E, Chan M, Renz N, Trampuz A. Current perspectives on diagnosis and management of sternal wound infections. Infect Drug Resist. 2018;16(11):961–8.
Wilcox MH, Dryden M. Update on the epidemiology of healthcare-acquired bacterial infections: focus on complicated skin and skin structure infections. J Antimicrob Chemother. 2021;76(Suppl 4):iv2-iv8.
Dohmen PM, Konertz W. A review of current strategies to reduce intraoperative bacterial contamination of surgical wounds. GMS Krankenhhyg Interdiszip. 2007;2(2):Doc38.
Shi D, Yao Y, Yu W. Comparison of preoperative hair removal methods for the reduction of surgical site infections: a meta-analysis. J Clin Nurs. 2017;26(19–20):2907–14.
Tanner J, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2021;8(8):CD004122.
•• Phoon PHY, Hwang NC. Deep sternal wound infection: diagnosis, treatment and prevention. J Cardiothorac Vasc Anesth. 2020;34(6):1602–13. A compehensive and extensive review on incidence, microbiology, risk factors, preventive measures and management of deep sternal wound infection after median sternotomy performed in cardiac surgery.
Poveda VB, Oliveira RA, Galvão CM. Perioperative body temperature maintenance and occurrence of surgical site infection: a systematic review with meta-analysis. Am J Infect Control. 2020;48(10):1248–54.
Hweidi IM, Zytoo AM, Hayajneh AA. Tight glycaemic control and surgical site infections post cardiac surgery: a systematic review. J Wound Care. 2021;30(Sup12):S22–8.
Jin X, Wang J, Ma Y, Li X, An P, Wang J, et al. Association between perioperative glycemic control strategy and mortality in patients with diabetes undergoing cardiac surgery: a systematic review and meta-analysis. Front Endocrinol (Lausanne). 2020;17(11).
Wojnarski CM, Elgudin Y, Rubelowsky JJ, Wilson BM, Donskey CJ, Cmolik BL. Emerging trends in mediastinitis: National Veterans Health Administration experience with methicillin-resistant Staphylococcus aureus prevention. J Thorac Cardiovasc Surg. 2021;162(4):1125-1130.e1.
Spindler N, Biereigel C, Pieroh P, Schroeter T, Misfeld M, Josten C, et al. Clinical and microbiological analysis of deep sternal wound infections in fifty-two consecutive patients. Surg Infect (Larchmt). 2020;21(4):370–7.
Alaia EF, Chhabra A, Simpfendorfer CS, Cohen M, Mintz DN, Vossen JA, et al. MRI nomenclature for musculoskeletal infection. Skeletal Radiol. 2021;50(12):2319–47.
Llewellyn A, Jones-Diette J, Kraft J, Holton C, Harden M, Simmonds M. Imaging tests for the detection of osteomyelitis: a systematic review. Health Technol Assess. 2019;23(61):1–128.
Sganga G, Baguneid M, Dohmen P, Giamarellos-Bourboulis EJ, Romanini E, et al. Management of superficial and deep surgical site infection: an international multidisciplinary consensus. Updates Surg. 2021;73(4):1315–25.
O’Keefe S, Williams K, Legare JF. Hospital-acquired infections after cardiac surgery and current physician practices: a retrospective cohort study. J Clin Med Res. 2017;9(1):10–6.
Kabbani MS, Ismail SR, Fatima A, Shafi R, Idris JA, Mehmood A, et al. Urinary tract infection in children after cardiac surgery: incidence, causes, risk factors and outcomes in a single-center study. J Infect Public Health. 2016;9(5):600–10.
Gillen JR, Isbell JM, Michaels AD, Lau CL, Sawyer RG. Risk factors for urinary tract infections in cardiac surgical patients. Surg Infect (Larchmt). 2015;16(5):504–8.
Barbadoro P, Labricciosa FM, Recanatini C, Gori G, Tirabassi F, Martini E, et al. Catheter-associated urinary tract infection: role of the setting of catheter insertion. Am J Infect Control. 2015;43(7):707–10.
Shadle HN, Sabol V, Smith A, Stafford H, Thompson JA, Bowers M. A Bundle-based approach to prevent catheter-associated urinary tract infections in the intensive care unit. Crit Care Nurse. 2021;41(2):62–71.
Andrioli ER, Furtado GH, Medeiros EA. Catheter-associated urinary tract infection after cardiovascular surgery: Impact of a multifaceted intervention. Am J Infect Control. 2016;44(3):289–93.
• Pajerski DM, Harlan MD, Ren D, Tuite PK. A clinical nurse specialist-led initiative to reduce catheter-associated urinary tract infection rates using a best practice guideline. Clin Nurse Spec. 2022;36(1):20–8. An interesting clinical nurse specialist initiative demonstrating that the use of a best practice guideline reduced the catheter-associated urinary tract infection rates and device utilization ratio.
Cove ME, Spelman DW, MacLaren G. Infectious complications of cardiac surgery: a clinical review. J Cardiothorac Vasc Anesth. 2012;26(6):1094–100.
Ding JG, Sun QF, Li KC, Zheng MH, Miao XH, Ni W, et al. Retrospective analysis of nosocomial infections in the intensive care unit of a tertiary hospital in China during 2003 and 2007. BMC Infect Dis. 2009;25(9):115.
Trethon A, Prinz G, Varga A, Kocsis I. Characteristics of nosocomial bloodstream infections at a Hungarian cardiac surgery centre. Acta Microbiol Immunol Hung. 2012;59(2):271–83.
Lola I, Levidiotou S, Petrou A, Arnaoutoglou H, Apostolakis E, Papadopoulos GS. Are there independent predisposing factors for postoperative infections following open heart surgery? J Cardiothorac Surg. 2011;14(6):151.
Lex DJ, Tóth R, Cserép Z, Breuer T, Sápi E, Szatmári A, et al. Postoperative differences between colonization and infection after pediatric cardiac surgery-a propensity matched analysis. J Cardiothorac Surg. 2013;2(8):166.
Anderson DJ, Arduino JM, Reed SD, Sexton DJ, Kaye KS, Grussemeyer CA, et al. Variation in the type and frequency of postoperative invasive Staphylococcus aureus infections according to type of surgical procedure. Infect Control Hosp Epidemiol. 2010;31(7):701–9.
Dhawan B, Chaudhry R, Hote M, Bhan A, Venugopal P. Infective complications of central venous catheters in cardiac surgical patients. Indian J Pathol Microbiol. 2001;44(2):125–9.
Giacobbe DR, Salsano A, Del Puente F, Miette A, Vena A, Corcione S, et al. Risk factors for candidemia after open heart surgery: results from a multicenter case-control study. Open Forum Infect Dis. 2020;7(8):ofaa233.
Fraser TG, Fatica C, Scarpelli M, Arroliga AC, Guzman J, Shrestha NK, et al. Decrease in Staphylococcus aureus colonization and hospital-acquired infection in a medical intensive care unit after institution of an active surveillance and decolonization program. Infect Control Hosp Epidemiol. 2010;31(8):779–83.
Fang S, Skeete D, Cullen JJ. Preoperative risk factors for postoperative Staphylococcus aureus nosocomial infections. Surg Technol Int. 2004;13:35–8.
Bacuzzi A, Cecchin A, Del Bosco A, Cantone G, Cuffari S. Recommendations and reports about central venous catheter-related infection. Surg Infect (Larchmt). 2006;7(Suppl 2):S65–7.
Timsit JF, Baleine J, Bernard L, Calvino-Gunther S, Darmon M, Dellamonica J, et al. Expert consensus-based clinical practice guidelines management of intravascular catheters in the intensive care unit. Ann Intensive Care. 2020;10(1):118.
Dezfulian C, Lavelle J, Nallamothu BK, Kaufman SR, Saint S. Rates of infection for single-lumen versus multilumen central venous catheters: a meta-analysis. Crit Care Med. 2003;31(9):2385–90.
Arvaniti K, Lathyris D, Clouva-Molyvdas P, Haidich AB, Mouloudi E, Synnefaki E, et al. Catheter-Related Infections in ICU (CRI-ICU) Group. Comparison of Oligon catheters and chlorhexidine-impregnated sponges with standard multilumen central venous catheters for prevention of associated colonization and infections in intensive care unit patients: a multicenter, randomized, controlled study. Crit Care Med. 2012;40(2):420–9.
Abou Elella R, Najm HK, Balkhy H, Bullard L, Kabbani MS. Impact of bloodstream infection on the outcome of children undergoing cardiac surgery. Pediatr Cardiol. 2010;31(4):483–9.
Abdul-Aziz MH, Driver E, Lipman J, Roberts JA. New paradigm for rapid achievement of appropriate therapy in special populations: coupling antibiotic dose optimization rapid microbiological methods. Expert Opin Drug Metab Toxicol. 2018;14(7):693–708.
Lazzaro A, De Girolamo G, Filippi V, Innocenti GP, Santinelli L, Ceccarelli G, et al. The interplay between host defense, infection, and clinical status in septic patients: a narrative review. Int J Mol Sci. 2022;23(2):803.
Pérez SB, Rodríguez-Fanjul J, García IJ, Hernando JM, Iriondo SM. Procalcitonin is a better biomarker than C-reactive protein in newborns undergoing cardiac surgery: the PROKINECA study. Biomark Insights. 2016;3(11):123–9.
Chai MG, Cotta MO, Abdul-Aziz MH, Roberts JA. What are the current approaches to optimising antimicrobial dosing in the intensive care unit? Pharmaceutics. 2020;12(7):638.
Greco G, Shi W, Michler RE, Meltzer DO, Ailawadi G, Hohmann SF, et al. Costs associated with health care-associated infections in cardiac surgery. J Am Coll Cardiol. 2015;65(1):15–23.
Mazzeffi M, Gammie J, Taylor B, Cardillo S, Haldane-Lutterodt N, Amoroso A, et al. Healthcare-associated infections in cardiac surgery patients with prolonged intensive care unit stay. Ann Thorac Surg. 2017;103(4):1165–70.
Tweddell S, Loomba RS, Cooper DS, Benscoter AL. Health care-associated infections are associated with increased length of stay and cost but not mortality in children undergoing cardiac surgery. Congenit Heart Dis. 2019;14(5):785–90.
Giraldi G, Montesano M, Napoli C, Frati P, La Russa R, Santurro A, et al. Healthcare-associated infections due to multidrug-resistant organisms: a surveillance study on extra hospital stay and direct costs. Curr Pharm Biotechnol. 2019;20(8):643–52.
Jenks PJ, Laurent M, McQuarry S, Watkins R. Clinical and economic burden of surgical site infection (SSI) and predicted financial consequences of elimination of SSI from an English hospital. J Hosp Infect. 2014;86(1):24–33.
Speir AM, Kasirajan V, Barnett SD, Fonner E Jr. Additive costs of postoperative complications for isolated coronary artery bypass grafting patients in Virginia. Ann Thorac Surg. 2009;88(1):40–5.
Masud F, Vykoukal D. Preventing healthcare-associated infections in cardiac surgical patients as a hallmark of excellence. Methodist Debakey Cardiovasc J. 2011;7(2):48–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Enrico M Zardi, Massimo Chello, Domenico M Zardi, Raffaele Barbato, Omar Giacinto, Ciro Mastroianni, and Mario Lusini declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Healthcare Associated Infections
The original online version of this article was revised due to the error in 6th Author's Family Name.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zardi, E.M., Chello, M., Zardi, D.M. et al. Nosocomial Extracardiac Infections After Cardiac Surgery. Curr Infect Dis Rep 24, 159–171 (2022). https://doi.org/10.1007/s11908-022-00787-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11908-022-00787-0