Abstract
Purpose of the Review
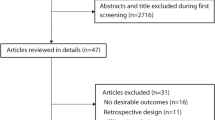
To assess the relationship between sodium intake and hypertension risk in cohort studies, based on a systematic review up to January 21, 2022, that also employed a dose–response meta-analysis.
Recent Findings
Dose–response analysis of available cohort studies (n = 11), using a dietary intake or urinary sodium excretion of 2 g/day as the reference category, showed an excess risk starting at 3 g/day. However, we found a linear relationship across the entire range of sodium exposure in an analysis restricted to studies that used 24 h urinary sodium excretion information and had a low risk of bias.
Summary
This review confirms prior findings based on experimental studies and identified an almost linear relationship between sodium intake/excretion and hypertension risk in cohort studies, reinforcing the validity of recommendations to prevent cardiovascular disease through the reduction of sodium intake in both normotensive and hypertensive adults.




Similar content being viewed by others
Data Availability
All supporting data are available within the article and its supplemental material.
Code Availability
All details of statistical command used for data analysis are provided in the Methods section.
References
Papers of particular interest, published recently, have been highlighted as: (with reasons) •• Of major importance
•• Carey RM, Whelton PK. New findings bearing on the prevention, detection and management of high blood pressure. Curr Opin Cardiol. 2021;36(4)429:435. https://doi.org/10.1097/HCO.0000000000000864. This report reviews the most recent findings and implications for the prevention, detection, and management of high BP and prevetion of CVD reinforcing the 2017 ACC/AHA BP guideline recommendations.
GBD. Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2015;388(10053):1545–602. https://doi.org/10.1016/S0140-6736(16)31678-6.
Lawes CM, Vander Hoorn S, Rodgers A. International Society of Hypertension. Global burden of blood-pressure-related disease. Lancet. 2008;371(9623):1513–8. https://doi.org/10.1016/S0140-6736(08)60655-8.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365(9455):217–23. https://doi.org/10.1016/S0140-6736(05)17741-1.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50. https://doi.org/10.1161/CIRCULATIONAHA.115.018912.
He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. https://doi.org/10.1136/bmj.f1325.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2018;138(17):e426–83. https://doi.org/10.1161/cir.0000000000000597.
Jones DW, Whelton PK, Allen N, Clark D 3rd, Gidding SS, Muntner P, et al. Management of stage 1 hypertension in adults with a low 10-year risk for cardiovascular disease: Filling a guidance gap: A scientific statement from the American Heart Association. Hypertension. 2021;77(6):e58–67. https://doi.org/10.1161/HYP.0000000000000195.
WHO. Guideline: Sodium intake for adults and children. Geneva: World Health Organization; 2012. https://www.who.int/publications/i/item/9789241504836.
•• Filippini T, Malavolti M, Whelton PK, Naska A, Orsini N, Vinceti M. Blood pressure effects of sodium reduction: Dose-response meta-analysis of experimental studies. Circulation. 2021;43(16)1542-67. https://doi.org/10.1161/CIRCULATIONAHA.120.050371. Recent dose-response meta-analysis on experimental studies showing a linear relatiponship between lowering of sodium intake and reduction of blood pressure levels in both hypertensive and normotensive subjects.
Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, Engell RE, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371(7):624–34. https://doi.org/10.1056/NEJMoa1304127.
Jayedi A, Ghomashi F, Zargar MS, Shab-Bidar S. Dietary sodium, sodium-to-potassium ratio, and risk of stroke: A systematic review and nonlinear dose-response meta-analysis. Clin Nutr. 2019;38(3):1092–100. https://doi.org/10.1016/j.clnu.2018.05.017.
Wang YJ, Yeh TL, Shih MC, Tu YK, Chien KL. Dietary sodium intake and risk of cardiovascular disease: A systematic review and dose-response meta-analysis. Nutrients. 2020;12(10):2934. https://doi.org/10.3390/nu12102934.
•• EFSA Panel on Nutrition; Novel Foods and Food Allergens (NDA), Turck D, Castenmiller J, de Henauw S, Hirsch-Ernst K-I, Kearney J, et al. Dietary reference values for sodium. EFSA J. 2019;17(9):e05778. https://doi.org/10.2903/j.efsa.2019.5778. This review provides updated evidence that a sodium intake of 2.0 g/day represents a safe and adequate intake to reduce risk of CVD in the general European population of adults.
WHO. Tackling NCDs: ‘Best buys' and other recommended interventions for the prevention and control of noncommunicable diseases. Geneva: WHO 2017 Contract No.: WHO/NMH/NVI/17.9.
•• National Academy of Sciences (US). The National Academies Collection: Reports funded by National Institutes of Health. In: Oria M, Harrison M, Stallings VA, editors. Dietary reference intakes for sodium and potassium. Washington (DC): National Academies Press (US). Copyright 2019 by the National Academy of Sciences. All rights reserved. 2019. This report updates the Dietary Reference Intakes for sodium and potassium including consideration of chronic disease endpoints, and outlines research gaps to address the uncertainties identified in the process of deriving the reference values and evaluating public health implications.
Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: Observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007;334(7599):885–8. https://doi.org/10.1136/bmj.39147.604896.55.
Whelton PK. Sodium, potassium, blood pressure, and cardiovascular disease in humans. Curr Hypertens Rep. 2014;16(8):465. https://doi.org/10.1007/s11906-014-0465-5.
Whelton PK, Campbell NRC, Lackland DT, Parati G, Ram CVS, Weber MA, et al. Strategies for prevention of cardiovascular disease in adults with hypertension. J Clin Hypertens (Greenwich). 2020;22(2):132–4. https://doi.org/10.1111/jch.13797.
Campbell NRC, Ordunez P, DiPette DJ, Giraldo GP, Angell SY, Jaffe MG, et al. Monitoring and evaluation framework for hypertension programs. A collaboration between the Pan American Health Organization and World Hypertension League. J Clin Hypertens (Greenwich). 2018;20(6):984–90. https://doi.org/10.1111/jch.13307.
He FJ, Campbell NRC, Woodward M, MacGregor GA. Salt reduction to prevent hypertension: The reasons of the controversy. Eur Heart J. 2021;45(25):2501–5. https://doi.org/10.1093/eurheartj/ehab274.
Whelton PK. Sodium, blood pressure, and cardiovascular disease. Hypertension. 2021;77(6):2138–9. https://doi.org/10.1161/HYPERTENSIONAHA.121.17223.
•• He FJ, MacGregor GA. Hypertension: Salt: flawed research should not divert actions to reduce intake. Nat Rev Nephrol. 2016;12(9):514–5. https://doi.org/10.1038/nrneph.2016.97. This review confirms that reduction in salt intake lowers BP levels, alleviates burden of CVD and other chronic diseases, and point out that paradoxical findings from methodologically flawed studies should not be used to refute the strong evidence on the benefits of salt reduction.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89. https://doi.org/10.1016/j.jclinepi.2021.03.001.
Morgan RL, Thayer KA, Santesso N, Holloway AC, Blain R, Eftim SE, et al. A risk of bias instrument for non-randomized studies of exposures: A users’ guide to its application in the context of GRADE. Environ Int. 2019;122:168–84. https://doi.org/10.1016/j.envint.2018.11.004.
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 2011. The Cochrane Collaboration.
Adani G, Filippini T, Wise LA, Halldorsson TI, Blaha L, Vinceti M. Dietary intake of acrylamide and risk of breast, endometrial and ovarian cancers: A systematic review and dose-response meta-analysis. Cancer Epidemiol Biomarkers Prev. 2020;29(6):1095–106. https://doi.org/10.1158/1055-9965.EPI-19-1628.
Filippini T, Hatch EE, Rothman KJ, Heck JE, Park AS, Crippa A, et al. Association between outdoor air pollution and childhood leukemia: A systematic review and dose-response meta-analysis. Environ Health Perspect. 2019;127(4):46002. https://doi.org/10.1289/EHP4381.
Filippini T, Hatch EE, Vinceti M. Residential exposure to electromagnetic fields and risk of amyotrophic lateral sclerosis: A dose-response meta-analysis. Sci Rep. 2021;11(1):11939. https://doi.org/10.1038/s41598-021-91349-2.
Urbano T, Vinceti M, Wise LA, Filippini T. Light at night and risk of breast cancer: A systematic review and dose-response meta-analysis. Int J Health Geogr. 2021;20(1):44. https://doi.org/10.1186/s12942-021-00297-7.
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: Examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175(1):66–73. https://doi.org/10.1093/aje/kwr265.
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S76–99. https://doi.org/10.1161/01.cir.0000437740.48606.d1.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953–2041. https://doi.org/10.1097/HJH.0000000000001940.
Crippa A, Discacciati A, Bottai M, Spiegelman D, Orsini N. One-stage dose-response meta-analysis for aggregated data. Stat Methods Med Res. 2019;28(5):1579–96. https://doi.org/10.1177/0962280218773122.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Batis C, Gordon-Larsen P, Cole SR, Du S, Zhang B, Popkin B. Sodium intake from various time frames and incident hypertension among Chinese adults. Epidemiology. 2013;24(3):410–8. https://doi.org/10.1097/EDE.0b013e318289e047.
Chien KL, Hsu HC, Chen PC, Su TC, Chang WT, Chen MF, et al. Urinary sodium and potassium excretion and risk of hypertension in Chinese: Report from a community-based cohort study in Taiwan. J Hypertens. 2008;26(9):1750–6. https://doi.org/10.1097/HJH.0b013e328306a0a7.
Ford ES, Cooper RS. Risk factors for hypertension in a national cohort study. Hypertension. 1991;18(5):598–606. https://doi.org/10.1161/01.hyp.18.5.598.
Forman JP, Scheven L, de Jong PE, Bakker SJ, Curhan GC, Gansevoort RT. Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of developing hypertension. Circulation. 2012;125(25):3108–16. https://doi.org/10.1161/CIRCULATIONAHA.112.096115.
He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension. 2000;35(2):544–9. https://doi.org/10.1161/01.hyp.35.2.544.
Hirayama A, Konta T, Hozawa A, Kawasaki R, Watanabe T, Shibata Y, et al. Slight increase in urinary albumin excretion within the normal range predicts incident hypertension in a community-based Japanese population: The Takahata study. Hypertens Res. 2015;38(1):56–60. https://doi.org/10.1038/hr.2014.117.
Hypertension Prevention Trial Research Group. The Hypertension Prevention Trial: Three-year effects of dietary changes on blood pressure. Hypertension Prevention Trial Research Group. Arch Intern Med 1990;150(1):153–62. https://doi.org/10.1001/archinte.1990.00390130131021.
Lee S, Kim SH, Shin C. Interaction according to urinary sodium excretion level on the association between ATP2B1 rs17249754 and incident hypertension: The Korean genome epidemiology study. Clin Exp Hypertens. 2016;38(4):352–8. https://doi.org/10.3109/10641963.2015.1116544.
Lelong H, Blacher J, Baudry J, Adriouch S, Galan P, Fezeu L, et al. Individual and combined effects of dietary factors on risk of incident hypertension: Prospective analysis from the NutriNet-Sante cohort. Hypertension. 2017;70(4):712–20. https://doi.org/10.1161/HYPERTENSIONAHA.117.09622.
Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerova J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA. 2011;305(17):1777–85. https://doi.org/10.1001/jama.2011.574.
Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA. 1997;277(20):1624–32.
He FJ, Tan M, Ma Y, MacGregor GA. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(6):632–47. https://doi.org/10.1016/j.jacc.2019.11.055.
Cook NR. Sodium and cardiovascular disease. N Engl J Med. 2014;371(22):2134. https://doi.org/10.1056/NEJMc1412113.
Oparil S. Low sodium intake–cardiovascular health benefit or risk? N Engl J Med. 2014;371(7):677–9. https://doi.org/10.1056/NEJMe1407695.
Cobb LK, Frieden TR, Appel LJ. No U-turn on sodium reduction. J Clin Hypertens (Greenwich). 2020;22(11):2156–60. https://doi.org/10.1111/jch.14021.
•• Whelton SP, McEvoy JW, Shaw L, Psaty BM, Lima JAC, Budoff M, et al. Association of normal systolic blood pressure level with cardiovascular disease in the absence of risk factors. JAMA Cardiol. 2020;5(9):1011-18. https://doi.org/10.1001/jamacardio.2020.1731. This study highlights the importance of primordial prevention to maintain optimal SBP levels and other traditional atherosclerotic cardiovascular disease also in subjects with BP conventionally considered within the normal ranges.
Hunt SC, Stephenson SH, Hopkins PN, Williams RR. Predictors of an increased risk of future hypertension in Utah. A screening analysis Hypertension. 1991;17(6 Pt 2):969–76. https://doi.org/10.1161/01.hyp.17.6.969.
Sun Z, Zheng L, Detrano R, Zhang X, Xu C, Li J, et al. Incidence and predictors of hypertension among rural Chinese adults: Results from Liaoning province. Ann Fam Med. 2010;8(1):19–24. https://doi.org/10.1370/afm.1018.
Takase H, Sugiura T, Kimura G, Ohte N, Dohi Y. Dietary sodium consumption predicts future blood pressure and Incident hypertension in the Japanese normotensive general population. J Am Heart Assoc. 2015;4(8):e001959. https://doi.org/10.1161/JAHA.115.001959.
Zhang LF, Zhao LC, Zhou BF, Li Y, Wu YF. A cohort study on the relationship between nutrients intake and the incidence of hypertension in middle-aged Chinese. Zhonghua Xin Xue Guan Bing Za Zhi. 2005;33(9):848–52. https://doi.org/10.3760/j:issn:0253-3758.2005.09.020.
Zheng L, Sun Z, Zhang X, Xu C, Li J, Hu D, et al. Predictors of progression from prehypertension to hypertension among rural Chinese adults: Results from Liaoning Province. Eur J Cardiovasc Prev Rehabil. 2010;17(2):217–22. https://doi.org/10.1097/HJR.0b013e328334f417.
Appel LJ, Espeland MA, Easter L, Wilson AC, Folmar S, Lacy CR. Effects of reduced sodium intake on hypertension control in older individuals: Results from the Trial of Nonpharmacologic Interventions in the Elderly (TONE). Arch Intern Med. 2001;161(5):685–93. https://doi.org/10.1001/archinte.161.5.685.
Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger WH Jr, Kostis JB, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: A randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group JAMA. 1998;279(11):839–46. https://doi.org/10.1001/jama.279.11.839.
Uzu T, Nakao K, Kume S, Araki H, Isshiki K, Araki S, et al. High sodium intake is associated with masked hypertension in Japanese patients with type 2 diabetes and treated hypertension. Am J Hypertens. 2012;25(11):1170–4. https://doi.org/10.1038/ajh.2012.102.
EFSA Panel on Dietetic Products; Nutrition and Allergies, Turck D, Bresson J-L, Burlingame B, Dean T, Fairweather-Tait S, et al. Dietary reference values for potassium. EFSA J. 2016;14(10):e04592. https://doi.org/10.2903/j.efsa.2016.4592.
Filippini T, Violi F, D’Amico R, Vinceti M. The effect of potassium supplementation on blood pressure in hypertensive subjects: A systematic review and meta-analysis. Int J Cardiol. 2017;230:127–35. https://doi.org/10.1016/j.ijcard.2016.12.048.
Whelton PK. Sodium and potassium intake in US adults. Circulation. 2018;137(3):247–9. https://doi.org/10.1161/CIRCULATIONAHA.117.031371.
•• Filippini T, Naska A, Kasdagli MI, Torres D, Lopes C, Carvalho C, et al. Potassium intake and blood pressure: A dose-response meta-analysis of randomized controlled trials. J Am Heart Assoc. 2020;9(12):e015719. https://doi.org/10.1161/JAHA.119.015719. This review suggests a possible nonlinear relationship between potassium intake and both SBP and DBP and indicates that an adequate intake of 3.5 g/day of potassium is desirable to achieve a lower BP level.
Vinceti M, Filippini T, Crippa A, de Sesmaisons A, Wise LA, Orsini N. Meta-analysis of potassium Intake and the risk of stroke. J Am Heart Assoc. 2016;5(10):e004210. https://doi.org/10.1161/JAHA.116.004210.
Malavolti M, Naska A, Fairweather-Tait SJ, Malagoli C, Vescovi L, Marchesi C, et al. Sodium and potassium content of foods consumed in an Italian population and the impact of adherence to a Mediterranean diet on their Intake. Nutrients. 2021;13(8):2681. https://doi.org/10.3390/nu13082681.
Howard G, Cushman M, Moy CS, Oparil S, Muntner P, Lackland DT, et al. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA. 2018;320(13):1338–48. https://doi.org/10.1001/jama.2018.13467.
Bernabe-Ortiz A, Sal YRVG, Ponce-Lucero V, Cardenas MK, Carrillo-Larco RM, Diez-Canseco F, et al. Effect of salt substitution on community-wide blood pressure and hypertension incidence. Nat Med. 2020;26(3):374–8. https://doi.org/10.1038/s41591-020-0754-2.
Kumanyika SK, Cook NR, Cutler JA, Belden L, Brewer A, Cohen JD, et al. Sodium reduction for hypertension prevention in overweight adults: further results from the Trials of Hypertension Prevention Phase II. J Hum Hypertens. 2005;19(1):33–45. https://doi.org/10.1038/sj.jhh.1001774.
Funding
Drs. Tommaso Filippini, Marcella Malavolti, and Marco Vinceti were supported by grant ‘Dipartimenti di Eccellenza 2018 to 2022’ to the UNIMORE Department of Biomedical, Metabolic and Neural Sciences from the Italian Ministry of Education, University and Research, and Dr. Tommaso Filippini by grant ‘UNIMORE FAR IMPULSO 2020’ (no. 494/2020) from the University of Modena and Reggio Emilia. Dr. Paul K. Whelton was supported by a Centers of Research Excellence grant from the National Institute of General Medical Sciences (no. P20GM109036).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research Involving Human and Animal Participants
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Hypertension and the Kidney
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Filippini, T., Malavolti, M., Whelton, P.K. et al. Sodium Intake and Risk of Hypertension: A Systematic Review and Dose–Response Meta-analysis of Observational Cohort Studies. Curr Hypertens Rep 24, 133–144 (2022). https://doi.org/10.1007/s11906-022-01182-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-022-01182-9