Abstract
Purpose of Review
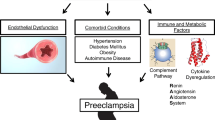
We focus on the current understanding of preeclampsia (PE) in order to examine how it mediates glomerular injury and affects the course of glomerulonephritis (GNs). In addition, this review discusses the role of GNs on the development of PE.
Recent Findings
In PE, the dysfunctional utero-placental perfusion causes the release into the mother’s circulation of anti-angiogenic substances, leading to systemic endotheliosis. In preeclamptic patients, the imbalance between pro- and anti-angiogenic factors is responsible for the kidney injury, and PE may reveal a silent pre-existent GN or may induce the development of the disease. Moreover, in women with chronic kidney disease (CKD), it could accelerate the disease progression. In any case, GNs compromise renal function, making the kidney less responsive to physiological changes that occur during pregnancy and, at the same time, cause maternal vascular inflammation, representing a risk factor for PE development.
Summary
Although a bidirectional correlation between GNs and PE has been demonstrated, the data are limited, and further large studies are warranted. Close collaboration between a multidisciplinary team of obstetricians and nephrologists is essential to establish the correct diagnosis and safely manage these vulnerable women and their fetuses.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Say L, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33.
Kongwattanakul K, et al. Incidence, characteristics, maternal complications, and perinatal outcomes associated with preeclampsia with severe features and HELLP syndrome. Int J Womens Health. 2018;10:371–7.
Phipps E, et al. Preeclampsia: updates in pathogenesis, definitions, and guidelines. Clin J Am Soc Nephrol. 2016;11(6):1102–13.
Staff AC. The two-stage placental model of preeclampsia: an update. J Reprod Immunol. 2019;134–135:1–10.
Xiong X, et al. Impact of preeclampsia and gestational hypertension on birth weight by gestational age. Am J Epidemiol. 2002;155(3):203–9.
Ness RB, Roberts JM. Heterogeneous causes constituting the single syndrome of preeclampsia: a hypothesis and its implications. Am J Obstet Gynecol. 1996;175(5):1365–70.
Redman CW. Current topic: pre-eclampsia and the placenta. Placenta. 1991;12(4):301–8.
Armaly Z, et al. Preeclampsia: novel mechanisms and potential therapeutic approaches. Front Physiol. 2018;9:973.
Burton GJ, et al. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta. 2009;30(6):473–82.
Redman CW, Sargent IL, Staff AC. IFPA Senior Award Lecture: making sense of pre-eclampsia - two placental causes of preeclampsia? Placenta. 2014;35(Suppl):S20–5.
Sircar M, Thadhani R, Karumanchi SA. Pathogenesis of preeclampsia. Curr Opin Nephrol Hypertens. 2015;24(2):131–8.
Staff AC, et al. Preeclampsia and uteroplacental acute atherosis: immune and inflammatory factors. J Reprod Immunol. 2014;101–102:120–6.
Moghaddas Sani H, Vahed SZ, Ardalan M. Preeclampsia: a close look at renal dysfunction. Biomed Pharmacother. 2019;109:408–16.
Spargo BH, et al. The renal lesion in preeclampsia. Perspect Nephrol Hypertens. 1976;5:129–37.
Stillman IE, Karumanchi SA. The glomerular injury of preeclampsia. J Am Soc Nephrol. 2007;18(8):2281–4.
Hussein W, Lafayette RA. Renal function in normal and disordered pregnancy. Curr Opin Nephrol Hypertens. 2014;23(1):46–53.
Johnson, RJ. Comprehensive clinical nephrology 6th Edition. Elsevier. 2019. SECTION VIII Pregnancy and Renal Disease, Chapter 42 - 43, p. 502–522.
Eremina V, et al. Glomerular-specific alterations of VEGF-A expression lead to distinct congenital and acquired renal diseases. J Clin Invest. 2003;111(5):707–16.
Eremina V, et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med. 2008;358(11):1129–36.
Galvis-Ramirez MF, Quintana-Castillo JC, Bueno-Sanchez JC. Novel insights into the role of glycans in the pathophysiology of glomerular endotheliosis in preeclampsia. Front Physiol. 2018;9:1470.
Collino F, et al. Preeclamptic sera induce nephrin shedding from podocytes through endothelin-1 release by endothelial glomerular cells. Am J Physiol Renal Physiol. 2008;294(5):F1185–94.
Craici IM, et al. Advances in the pathophysiology of pre-eclampsia and related podocyte injury. Kidney Int. 2014;86(2):275–85.
•• Wang Y, et al. Loss of slit protein nephrin is associated with reduced antioxidant superoxide dismutase expression in podocytes shed from women with preeclampsia. Physiol Rep. 2018;6(13):e13785 This paper shows that reduced nephrin and podoplanin expression is associated with increased oxidative stress, that plays a significant role in inducing podocyte protein shedding in PE.
Wang Y, et al. Increased urinary levels of podocyte glycoproteins, matrix metallopeptidases, inflammatory cytokines, and kidney injury biomarkers in women with preeclampsia. Am J Physiol Renal Physiol. 2015;309(12):F1009–17.
Zhao S, et al. Altered nephrin and podoplanin distribution is associated with disturbed polarity protein PARD-3 and PARD-6 expressions in podocytes from preeclampsia. Reprod Sci. 2011;18(8):772–80.
Ponticelli C, Moroni G. Is preeclampsia a risk for end-stage renal disease? Kidney Int. 2019;96(3):547–9.
•• Covella B, et al. A systematic review and meta-analysis indicates long-term risk of chronic and end-stage kidney disease after preeclampsia. Kidney Int. 2019;96(3):711–27 This is a very useful systematic review and a meta-analysis. The authors report that the relative risk of ESRD was significantly greater (6.35) in 110,803 women who had PE in comparison with 2,680,929 control subjects without PE.
Di Marco GS, et al. The soluble VEGF receptor sFlt1 contributes to endothelial dysfunction in CKD. J Am Soc Nephrol. 2009;20(10):2235–45.
Foster RR. The importance of cellular VEGF bioactivity in the development of glomerular disease. Nephron Exp Nephrol. 2009;113(1):e8–e15.
Zhang JJ, et al. A systematic review and meta-analysis of outcomes of pregnancy in CKD and CKD outcomes in pregnancy. Clin J Am Soc Nephrol. 2015;10(11):1964–78.
Floege J, Amann K. Primary glomerulonephritides. Lancet. 2016;387(10032):2036–48.
•• Wang F, et al. Renal outcomes of pregnant patients with immunoglobulin A nephropathy: a systematic review and meta-analysis. Am J Nephrol. 2019;49(3):214–24 This is a large recent meta-analysis including 145 renal events in 1198 participants, in which the authors concluded that pregnancy did not accelerate kidney disease deterioration in women with IgAN in stages of chronic kidney disease 1–3.
Piccoli GB, et al. A systematic review on materno-foetal outcomes in pregnant women with IgA nephropathy: a case of "late-maternal" preeclampsia? J Clin Med. 2018;7(8).
Piccoli GB, et al. Maternal-foetal outcomes in pregnant women with glomerulonephritides. Are all glomerulonephritides alike in pregnancy? J Autoimmun. 2017;79:91–8.
• Zhai YL, et al. Elevated soluble VEGF receptor sFlt-1 correlates with endothelial injury in IgA nephropathy. PLoS One. 2014;9(7):e101779 This is a very interesting study, in which the authors show that VEGF/sFlt-1 levels are significantly lower in IgAN patients than healthy volunteers. The plasma sFlt-1 levels are significantly elevated and correlated with proteinuria, hypertension, and vWF levels.
Gaber LW, Spargo BH. Pregnancy-induced nephropathy: the significance of focal segmental glomerulosclerosis. Am J Kidney Dis. 1987;9(4):317–23.
Suzuki H, Inoue T. Renal diseases associated with pre-eclampsia in postmenopausal women. J Clin Nephrol Res. 2014;1(2):1011.
Orozco Guillen OA, et al. Collapsing lesions and focal segmental glomerulosclerosis in pregnancy: a report of 3 cases. Am J Kidney Dis. 2019;74(6):837–43.
Garovic VD. The role of the podocyte in preeclampsia. Clin J Am Soc Nephrol. 2014;9(8):1337–40.
Penning ME, et al. Association of preeclampsia with podocyte turnover. Clin J Am Soc Nephrol. 2014;9(8):1377–85.
Oliverio AL, et al. Renal complications in pregnancy preceding glomerulonephropathy diagnosis. Kidney Int Rep. 2019;4(1):159–62.
Jara LJ, et al. Risk factors of systemic lupus erythematosus flares during pregnancy. Immunol Res. 2014;60(2–3):184–92.
•• Andreoli L, et al. EULAR recommendations for women's health and the management of family planning, assisted reproduction, pregnancy and menopause in patients with systemic lupus erythematosus and/or antiphospholipid syndrome. Ann Rheum Dis. 2017;76(3):476–85 This systematic review of evidence provides recommendations for women's health issues in SLE and was developed using an evidence-based approach followed by expert consensus.
Yang H, et al. Pregnancy-related systemic lupus erythematosus: clinical features, outcome and risk factors of disease flares--a case control study. PLoS One. 2014;9(8):e104375.
Marder W, et al. Placental histology and neutrophil extracellular traps in lupus and pre-eclampsia pregnancies. Lupus Sci Med. 2016;3(1):e000134.
Moroni G, et al. Maternal outcome in pregnant women with lupus nephritis. a prospective multicenter study. J Autoimmun. 2016;74:194–200.
Moroni G, et al. Fetal outcome and recommendations of pregnancies in lupus nephritis in the 21st century. a prospective multicenter study. J Autoimmun. 2016;74:6–12.
Carmona F, et al. Class III-IV proliferative lupus nephritis and pregnancy: a study of 42 cases. Am J Reprod Immunol. 2005;53(4):182–8.
Rodrigues BC, et al. The impact of different classes of lupus nephritis on maternal and fetal outcomes: a cohort study of 147 pregnancies. Lupus. 2019;28(4):492–500.
Lightstone L, Hladunewich MA. Lupus nephritis and pregnancy: concerns and management. Semin Nephrol. 2017;37(4):347–53.
Smyth A, et al. A systematic review and meta-analysis of pregnancy outcomes in patients with systemic lupus erythematosus and lupus nephritis. Clin J Am Soc Nephrol. 2010;5(11):2060–8.
•• Gianfreda D, et al. Does pregnancy have any impact on long term damage accrual and on the outcome of lupus nephritis? J Autoimmun. 2017;84:46–54 This retrospective cohort study aims at establishing the long-term impact of pregnancy on renal and extra renal SLE activity, on the development of CKD, and on the increase of damage in LN patients.
Mecacci F, et al. Preeclampsia in pregnancies complicated by systemic lupus erythematosus (SLE) nephritis: prophylactic treatment with multidisciplinary approach are important keys to prevent adverse obstetric outcomes. J Matern Fetal Neonatal Med. 2019;32(8):1292–8.
Berger H, Gagnon R, Sermer M. Guideline No. 393-diabetes in pregnancy. J Obstet Gynaecol Can. 2019;41(12):1814–25 e1.
Bramham K. Diabetic nephropathy and pregnancy. Semin Nephrol. 2017;37(4):362–9.
Klemetti MM, et al. Obstetric and perinatal outcome in type 1 diabetes patients with diabetic nephropathy during 1988–2011. Diabetologia. 2015;58(4):678–86.
Bell R, et al. Trends in prevalence and outcomes of pregnancy in women with pre-existing type I and type II diabetes. BJOG. 2008;115(4):445–52.
Damm JA, et al. Diabetic nephropathy and microalbuminuria in pregnant women with type 1 and type 2 diabetes: prevalence, antihypertensive strategy, and pregnancy outcome. Diabetes Care. 2013;36(11):3489–94.
Jensen DM, et al. Microalbuminuria, preeclampsia, and preterm delivery in pregnant women with type 1 diabetes: results from a nationwide Danish study. Diabetes Care. 2010;33(1):90–4.
Gordin D, et al. Pre-eclampsia but not pregnancy-induced hypertension is a risk factor for diabetic nephropathy in type 1 diabetic women. Diabetologia. 2007;50(3):516–22.
Imbasciati E, et al. Pregnancy in CKD stages 3 to 5: fetal and maternal outcomes. Am J Kidney Dis. 2007;49(6):753–62.
Uchino E, et al. Membranous nephropathy associated with pregnancy: an anti-phospholipase A2 receptor antibody-positive case report. CEN Case Rep. 2018;7(1):101–6.
Ope-Adenuga S, Moretti M, Lakhi N. Management of membranous glomerulonephritis in pregnancy: A multidisciplinary challenge. Case Rep Obstet Gynecol. 2015;2015:839376.
De Castro I, et al. Nephrotic syndrome in pregnancy poses risks with both maternal and fetal complications. Kidney Int. 2017;91(6):1464–72.
Blom K, et al. Pregnancy and glomerular disease: a systematic review of the literature with management guidelines. Clin J Am Soc Nephrol. 2017;12(11):1862–72.
Day C, et al. The role of renal biopsy in women with kidney disease identified in pregnancy. Nephrol Dial Transplant. 2008;23(1):201–6.
•• Webster P, et al. A multicenter cohort study of histologic findings and long-term outcomes of kidney disease in women who have been pregnant. Clin J Am Soc Nephrol. 2017;12(3):408–16 This study compares causes and long-term renal outcomes of biopsy-proven renal disease identified during pregnancy or within 1 year postpartum, with non those in pregnant women.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Preeclampsia
Rights and permissions
About this article
Cite this article
Di Leo, V., Capaccio, F. & Gesualdo, L. Preeclampsia and Glomerulonephritis: A Bidirectional Association. Curr Hypertens Rep 22, 36 (2020). https://doi.org/10.1007/s11906-020-1033-9
Published:
DOI: https://doi.org/10.1007/s11906-020-1033-9