Abstract
The HIV pandemic has disproportionately impacted sub-Saharan Africa and Southern Africa in particular. The concurrent presence of overlapping epidemic drivers likely underpins how and why the HIV epidemic is so explosive in this region, with implications for understanding approaches to reduce transmission. In this review, we discuss the relative contribution and interaction between epidemic drivers in the Southern African context, including factors both distally and proximally associated with the likelihood and degree of exposure to HIV and factors that increase the probability of transmission when exposure occurs. In particular, we focus on young women as a key population in need of HIV prevention and highlight factors that increase their risk on several levels.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
2011 National Antenatal HIV & Syphilis Prevalence Survey released - Health-e. google.co.za at http://www.google.co.za/search?client = safari&rls = 10_7_4&hl = en-ZA&source = hp&q = http%3A%2F%2Fwww.health-e.org.za%2F2012%2F12%2F11%2F2011-national-antenatal-hiv-syphilis-prevalence-survey-released%2F&gbv = 2&oq = http%3A%2F%2Fwww.health-e.org.za%2F2012%2F12%2F11%2F2011-national-antenatal-hiv-syphilis-prevalence-survey-released%2F&gs_l = heirloom-hp.3…747.747.0.1615.1.1.0.0.0.0.0.0..0.0.msedr…0…1ac.1.34.heirloom-hp..1.0.0.vQOe8rYMO8g
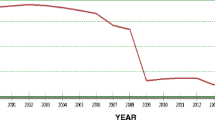
Kharsany ABM et al. Trends in HIV prevalence in pregnant women in rural South Africa. J Acquir Immune Defic Syndr. 2015;70:289–95.
Nagelkerke NJD et al. The rise and fall of HIV in high-prevalence countries: a challenge for mathematical modeling. PLoS Comput Biol. 2014;10:e1003459.
Chen L et al. Sexual risk factors for HIV infection in early and advanced HIV epidemics in sub-Saharan Africa: systematic overview of 68 epidemiological studies. PLoS One. 2007;2:e1001.
McKinnon LR et al. High HIV risk in a cohort of male sex workers from Nairobi, Kenya. Sex Transm Infect. 2014;90:237–42.
Sanders EJ, Jaffe H, Musyoki H, Muraguri N, Graham SM. Kenyan MSM: no longer a hidden population. AIDS. 2015;29 Suppl 3:S195–9.
Rispel LC, Metcalf CA, Cloete A, Reddy V, Lombard C. HIV prevalence and risk practices among men who have sex with men in two South African cities. J Acquir Immune Defic Syndr. 2011;57:69–76.
Sandfort TGM, Lane T, Dolezal C, Reddy V. Gender expression and risk of HIV infection among Black South African men who have sex with men. AIDS Behav. 2015;19:2270–9.
Dunkle KL, Jewkes RK, Murdock DW, Sikweyiya Y, Morrell R. Prevalence of consensual male-male sex and sexual violence, and associations with HIV in South Africa: a population-based cross-sectional study. PLoS Med. 2013;10:e1001472.
Karim QA et al. Stabilizing HIV prevalence masks high HIV incidence rates amongst rural and urban women in KwaZulu-Natal, South Africa. Int J Epidemiol. 2011;40:922–30.
Tanser F, Bärnighausen T, Grapsa E, Zaidi J, Newell M-L. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science. 2013;966. This important cohort analysis followed up on the HPTN052 clinical trial results suggesting that ART prevents HIV acquisition. Importantly, these effects were seen in a large population in the context of community treatment programs, suggesting real-world effectiveness of ART as a prevention strategy.
Abdool Karim Q, Sibeko S, Baxter C. Preventing HIV infection in women: a global health imperative. Clin Infect Dis. 2010;50 Suppl 3:S122–9.
Kapogiannis BG, Legins KE, Chandan U, Lee S. Evidence-based programming for adolescent HIV prevention and care: operational research to inform best practices. J Acquir Immune Defic Syndr. 2014;66 Suppl 2:S228–35.
Eaton JW et al. Health benefits, costs, and cost-effectiveness of earlier eligibility for adult antiretroviral therapy and expanded treatment coverage: a combined analysis of 12 mathematical models. Lancet Glob Health. 2014;2:e23–34.
Tanser F, de Oliveira T, Maheu-Giroux M, Bärnighausen T. Concentrated HIV subepidemics in generalized epidemic settings. Curr Opin HIV AIDS. 2014;9:115–25.
Gerberry DJ, Wagner BG, García-Lerma JG, Heneine W, Blower S. Using geospatial modelling to optimize the rollout of antiretroviral-based pre-exposure HIV interventions in Sub-Saharan Africa. Nat Commun. 2014;5:5454. This paper highlights a major shift in focus of strategies to fight the epidemic in light of antiretroviral-based prevention, and that is finding ways to focus on those most in need and where transmission densities are highest.
Kasedde S, Kapogiannis BG, McClure C, Luo C. Executive summary: opportunities for action and impact to address HIV and AIDS in adolescents. J Acquir Immune Defic Syndr. 2014;66 Suppl 2:S139–43.
Horton R. African AIDS beyond Mbeki: tripping into anarchy. Lancet. 2000;356:1541–2.
Tan JY, Huedo-Medina TB, Warren MR, Carey MP, Johnson BT. A meta-analysis of the efficacy of HIV/AIDS prevention interventions in Asia, 1995–2009. Soc Sci Med. 2012;75:676–87.
Chandrasekaran P et al. Evaluation design for large-scale HIV prevention programmes: the case of Avahan, the India AIDS initiative. AIDS. 2008;22 Suppl 5:S1–15.
Tladi LS. Poverty and HIV/AIDS in South Africa: an empirical contribution. SAHARA J. 2006;3:369–81.
Kalichman SC et al. Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Soc Sci Med. 2006;62:1641–9.
Fenton L. Preventing HIV/AIDS through poverty reduction: the only sustainable solution? Lancet. 2004;364:1186–7.
Weine SM, Kashuba AB. Labor migration and HIV risk: a systematic review of the literature. AIDS Behav. 2012;16:1605–21.
Shisana O, Rice K, Zungu N, Zuma K. Gender and poverty in South Africa in the era of HIV/AIDS: a quantitative study. J Womens Health (Larchmt). 2010;19:39–46.
Mishra V et al. HIV infection does not disproportionately affect the poorer in sub-Saharan Africa. AIDS. 2007;21 Suppl 7:S17–28.
Jewkes RK, Levin JB, Penn-Kekana LA. Gender inequalities, intimate partner violence and HIV preventive practices: findings of a South African cross-sectional study. Soc Sci Med. 2003;56:125–34.
Shamu S et al. Prevalence and risk factors for intimate partner violence among Grade 8 learners in urban South Africa: baseline analysis from the Skhokho Supporting Success cluster randomised controlled trial. Int Health. 2016;8:18–26.
MacPherson EE, Richards E, Namakhoma I, Theobald S. Gender equity and sexual and reproductive health in Eastern and Southern Africa: a critical overview of the literature. Glob Health Action. 2014;7:23717.
Durevall D, Lindskog A. Intimate partner violence and HIV in ten sub-Saharan African countries: what do the Demographic and Health Surveys tell us? Lancet Glob Health. 2015;3:e34–43. This study used several large national datasets to explore in more detail the associations between intimate partner violence and HIV, providing insight into scenarios where the linkage between these two factors is strongest.
Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8:141–51.
Hargreaves JR et al. Systematic review exploring time trends in the association between educational attainment and risk of HIV infection in sub-Saharan Africa. AIDS. 2008;22:403–14.
Bärnighausen T, Hosegood V, Timaeus IM, Newell M-L. The socioeconomic determinants of HIV incidence: evidence from a longitudinal, population-based study in rural South Africa. AIDS. 2007;21 Suppl 7:S29–38.
Pettifor AE et al. Keep them in school: the importance of education as a protective factor against HIV infection among young South African women. Int J Epidemiol. 2008;37:1266–73.
Stroeken K et al. HIV among out-of-school youth in Eastern and Southern Africa: a review. AIDS Care. 2012;24:186–94.
Abdool Karim Q et al. HIV incidence in young girls in KwaZulu-Natal, South Africa—public health imperative for their inclusion in HIV biomedical intervention trials. AIDS Behav. 2012;16:1870–6.
Mugo NR et al. Increased risk of HIV-1 transmission in pregnancy: a prospective study among African HIV-1-serodiscordant couples. AIDS. 2011;25:1887–95.
Discussion Paper: Cash Transfers and HIV Prevention | UNDP. google.co.za at http://www.google.co.za/search?client = safari&rls = 10_7_4&hl = en-ZA&source = hp&q = http%3A%2F%2Fwww.undp.org%2Fcontent%2Fundp%2Fen%2Fhome%2Flibrarypage%2Fhiv-aids%2Fdiscussion-paper--cash-transfers-and-hiv-prevention%2F&gbv = 2&oq = http%3A%2F%2Fwww.undp.org%2Fcontent%2Fundp%2Fen%2Fhome%2Flibrarypage%2Fhiv-aids%2Fdiscussion-paper--cash-transfers-and-hiv-prevention%2F&gs_l = heirloom-hp.3…704.704.0.1229.1.1.0.0.0.0.0.0..0.0.msedr…0…1ac.1.34.heirloom-hp..1.0.0.pp_kSQ_vP_o
Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379:1320–9.
de Walque D et al. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open. 2012;2:e000747.
Kohler H-P, Thornton R. Conditional cash transfers and HIV/AIDS prevention: unconditionally promising? World Bank Econ Rev. 2012;26:165–90.
Fieno J, Leclerc-Madlala S. The promise and limitations of cash transfer programs for HIV prevention. Afr J AIDS Res. 2014;13:153–60.
Abdool Karim Q et al. Prevalence of HIV, HSV-2 and pregnancy among high school students in rural KwaZulu-Natal. South Africa: a bio-behavioural cross-sectional survey Sex Transm Infect. 2014;90:620–6.
Pettifor A, et al. HPTN 068: A Randomized Control Trial of a Conditional Cash Transfer to Reduce HIV Infection in Young Women in South Africa-Study Design and Baseline Results. AIDS Behav. 2016. doi:10.1007/s10461-015-1270-0
Abdool Karim Q, Leask K, Kharsany A, Humphries H, Ntombela F, Samsunder N, Baxter C, Frohlich J, van der Elst L, Abdool Karim S. Impact of conditional cash incentives on HSV-2 and HIV prevention in rural South African high school students: results of the CAPRISA 007 cluster randomized controlled trial. (TUAC0101LB). 8th IAS Conference on HIV Pathogenesis, Treatment & Prevention 19–22 July 2015, Vancouver, Canada. J Int AIDS Soc. 2015;18. References [46••] and [47••] explore the possibility of a school-based intervention to prevent HIV transmission, in particular to young women in rural South Africa, by in various ways providing an incentive-based behavioural intervention. Importantly, neither of these studies showed an HIV effect while [46••] showed an HSV2 effect. Understanding these outcomes is critical to the decision of if and how to move forward with this strategy.
Pettifor A, MacPhail C, Selin A, Gomez-Olivé X, Hughes J, Wagner R, Mabuza W, Mokoena I, Eshleman S, Piwowar-Manning E, Twine R, Julien A, Marcus C, Andrew P, Wang J, Xing Y, McKinstry L, Hamilton E, Agyei Y, Allison S, Sato P, Townley E, Tollman S, Kahn K, HPTN 068 Study Team. HPTN 068 conditional cash transfer to prevent HIV infection among young women in South Africa: results of a randomized controlled tria (TUAC0106LB). 8th IAS Conference on HIV Pathogenesis, Treatment & Prevention 19–22 July 2015, Vancouver, Canada. J Int AIDS Soc. 2015;18. References [46••] and [47••] explore the possibility of a school-based intervention to prevent HIV transmission, in particular to young women in rural South Africa, by in various ways providing an incentive-based behavioural intervention. Importantly, neither of these studies showed an HIV effect while [46••] showed an HSV2 effect. Understanding these outcomes is critical to the decision of if and how to move forward with this strategy.
Wagman JA et al. Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: analysis of an intervention in an existing cluster randomised cohort. Lancet Glob Health. 2015;3:e23–33. References [48••], [49••], and [50••] are cluster-randomized studies that all show positive outcomes for interventions to reduce violence including gender-based and intimate partner violence in the context of broader HIV prevention efforts.
Abramsky T et al. Findings from the SASA! Study: a cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Med. 2014;12:122. References [48••], [49••], and [50••] are cluster-randomized studies that all show positive outcomes for interventions to reduce violence including gender-based and intimate partner violence in the context of broader HIV prevention efforts.
Devries KM et al. The Good School Toolkit for reducing physical violence from school staff to primary school students: a cluster-randomised controlled trial in Uganda. Lancet Glob Health. 2015;3:e378–86. References [48••], [49••], and [50••] are cluster-randomized studies that all show positive outcomes for interventions to reduce violence including gender-based and intimate partner violence in the context of broader HIV prevention efforts..
Green EP, Blattman C, Jamison J, Annan J. Women’s entrepreneurship and intimate partner violence: a cluster randomized trial of microenterprise assistance and partner participation in post-conflict Uganda (SSM-D-14-01580R1). Soc Sci Med. 2015;133:177–88.
Kajula L et al. Vijana Vijiweni II: a cluster-randomized trial to evaluate the efficacy of a microfinance and peer health leadership intervention for HIV and intimate partner violence prevention among social networks of young men in Dar es Salaam. BMC Public Health. 2016;16:113.
Mathews C et al. Reaching the hard to reach: longitudinal investigation of adolescents’ attendance at an after-school sexual and reproductive health programme in Western Cape, South Africa. BMC Public Health. 2015;15:608.
Quinn TC et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N Engl J Med. 2000;342:921–9.
Baeten JM et al. Genital HIV-1 RNA predicts risk of heterosexual HIV-1 transmission. Sci Transl Med. 2011;3:77ra29.
Hughes JP et al. Determinants of per-coital-act HIV-1 infectivity among African HIV-1-serodiscordant couples. J Infect Dis. 2012;205:358–65.
Cohen MS et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Donnell D et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–8.
Stöckl H, Kalra N, Jacobi J, Watts C. Is early sexual debut a risk factor for HIV infection among women in sub-Saharan Africa? A systematic review. Am J Reprod Immunol. 2013;69 Suppl 1:27–40.
Pilgrim NA et al. Family structure effects on early sexual debut among adolescent girls in Rakai, Uganda. Vulnerable Child Youth Stud. 2014;9:193–205.
Seth P, DiClemente RJ, Lovvorn AE. State of the evidence: intimate partner violence and HIV/STI risk among adolescents. Curr HIV Res. 2013;11:528–35.
Maughan-Brown B, Kenyon C, Lurie MN. Partner age differences and concurrency in South Africa: implications for HIV-infection risk among young women. AIDS Behav. 2014;18:2469–76.
Harling G et al. Do age-disparate relationships drive HIV incidence in young women? Evidence from a population cohort in rural KwaZulu-Natal, South Africa. J Acquir Immune Defic Syndr. 2014;66:443–51.
Pettifor A et al. Preventing HIV among young people: research priorities for the future. J Acquir Immune Defic Syndr. 2013;63 Suppl 2:S155–60.
Helleringer S, Kohler H-P. Sexual network structure and the spread of HIV in Africa: evidence from Likoma Island, Malawi. AIDS. 2007;21:2323–32.
Morris M, Kretzschmar M. Concurrent partnerships and the spread of HIV. AIDS. 1997;11:641–8.
Tanser F et al. Effect of concurrent sexual partnerships on rate of new HIV infections in a high-prevalence, rural South African population: a cohort study. Lancet. 2011;378:247–55.
Wawer MJ et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis. 2005;191:1403–9.
Brenner B, Wainberg MA, Roger M. Phylogenetic inferences on HIV-1 transmission: implications for the design of prevention and treatment interventions. AIDS. 2013;27:1045–57.
Eaton JW, Hallett TB. Why the proportion of transmission during early-stage HIV infection does not predict the long-term impact of treatment on HIV incidence. Proc Natl Acad Sci U S A. 2014;111:16202–7. This paper deals with an important issue that has caused substantial controversy; HIV transmission during acute infection. Using mathematical models the authors argue that there are several reasons to think this may not be a significant barrier to slowing the epidemic by treatment.
Cohen MS, Pilcher CD. Amplified HIV transmission and new approaches to HIV prevention. J Infect Dis. 2005;191:1391–3.
Lewis F, Hughes GJ, Rambaut A, Pozniak A, Leigh Brown AJ. Episodic sexual transmission of HIV revealed by molecular phylodynamics. PLoS Med. 2008;5:e50.
Brenner BG, Wainberg MA. Future of phylogeny in HIV prevention. J Acquir Immune Defic Syndr. 2013;63 Suppl 2:S248–54.
Wertheim JO et al. The global transmission network of HIV-1. J Infect Dis. 2014;209:304–13.
Lai A et al. HIV-1 A1 subtype epidemic in Italy originated from Africa and Eastern Europe and shows a high frequency of transmission chains involving intravenous drug users. PLoS One. 2016;11:e0146097.
Ratmann O et al. Sources of HIV infection among men having sex with men and implications for prevention. Sci Transl Med. 2016;8:320ra2.
Patel P et al. Estimating per-act HIV transmission risk: a systematic review. AIDS. 2014;28:1509–19.
Dennis AM et al. Phylogenetic studies of transmission dynamics in generalized HIV epidemics: an essential tool where the burden is greatest? J Acquir Immune Defic Syndr. 2014;67:181–95.
Kharsany ABM et al. HIV infection in high school students in rural South Africa: role of transmissions among students. AIDS Res Hum Retroviruses. 2014;30:956–65. References [80••] and [81••] are some of the first to study heterosexual HIV transmission networks in Africa using phylogenetics, which has substantial potential to be expanded and gain insight into how to target interventions to where they can have the most impact.
Grabowski MK et al. The role of viral introductions in sustaining community-based HIV epidemics in rural Uganda: evidence from spatial clustering, phylogenetics, and egocentric transmission models. PLoS Med. 2014;11:e1001610. References [80••] and [81••] are some of the first to study heterosexual HIV transmission networks in Africa using phylogenetics, which has substantial potential to be expanded and gain insight into how to target interventions to where they can have the most impact.
Scott-Sheldon LAJ, Walstrom P, Harrison A, Kalichman SC, Carey MP. Sexual risk reduction interventions for HIV prevention among South African youth: a meta-analytic review. Curr HIV Res. 2013;11:549–58.
Protogerou C, Johnson BT. Factors underlying the success of behavioral HIV-prevention interventions for adolescents: a meta-review. AIDS Behav. 2014;18:1847–63.
Jewkes R et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. BMJ. 2008;337:a506.
Kaul R, et al. Inflammation and HIV Transmission in Sub-Saharan Africa. Curr HIV/AIDS Rep. 2015. doi:10.1007/s11904-015-0269-5
Boily M-C et al. Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies. Lancet Infect Dis. 2009;9:118–29.
Powers KA, Poole C, Pettifor AE, Cohen MS. Rethinking the heterosexual infectivity of HIV-1: a systematic review and meta-analysis. Lancet Infect Dis. 2008;8:553–63.
Abu-Raddad LJ et al. Have the explosive HIV epidemics in sub-Saharan Africa been driven by higher community viral load? AIDS. 2013;27:981–9. This reference along with reference [93] suggest that clade C infections do not have higher viral loads nor are they more transmissible than other clades. These are both important issues that have been proposed to fuel the more substantial epidemics in Southern Africa, and these two large, well-designed analyses fail to find evidence to support this idea.
Van Harmelen JH et al. A predominantly HIV type 1 subtype C-restricted epidemic in South African urban populations. AIDS Res Hum Retroviruses. 1999;15:395–8.
McKinnon LR et al. HIV-1 clade D is associated with increased rates of CD4 decline in a Kenyan cohort. PLoS One. 2012;7:e49797.
Kiwanuka N et al. Effect of human immunodeficiency virus Type 1 (HIV-1) subtype on disease progression in persons from Rakai, Uganda, with incident HIV-1 infection. J Infect Dis. 2008;197:707–13.
Baeten JM et al. HIV-1 subtype D infection is associated with faster disease progression than subtype A in spite of similar plasma HIV-1 loads. J Infect Dis. 2007;195:1177–80.
Kahle E et al. HIV-1 subtype C is not associated with higher risk of heterosexual HIV-1 transmission: a multinational study among HIV-1 serodiscordant couples. AIDS. 2014;28:235–43.
McKinnon LR, Kaul R. Quality and quantity: mucosal CD4+ T cells and HIV susceptibility. Curr Opin HIV AIDS. 2012;7:195–202.
Montague C et al. Implementation of adolescent-friendly voluntary medical male circumcision using a school based recruitment program in rural KwaZulu-Natal, South Africa. PLoS One. 2014;9:e96468.
Moses S et al. Geographical patterns of male circumcision practices in Africa: association with HIV seroprevalence. Int J Epidemiol. 1990;19:693–7.
Bailey RC et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–56.
Gray RH et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–66.
Auvert B et al. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:e298.
Hayes R, Watson-Jones D, Celum C, van de Wijgert J, Wasserheit J. Treatment of sexually transmitted infections for HIV prevention: end of the road or new beginning? AIDS. 2010;24 Suppl 4:S15–26.
Freeman EE et al. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS. 2006;20:73–83.
Houlihan CF et al. Human papillomavirus infection and increased risk of HIV acquisition. A systematic review and meta-analysis. AIDS. 2012;26:2211–22.
Atashili J, Poole C, Ndumbe PM, Adimora AA, Smith JS. Bacterial vaginosis and HIV acquisition: a meta-analysis of published studies. AIDS. 2008;22:1493–501.
Ralph LJ, McCoy SI, Shiu K, Padian NS. Hormonal contraceptive use and women’s risk of HIV acquisition: a meta-analysis of observational studies. Lancet Infect Dis. 2015. doi:10.1016/S1473-3099(14)71052-7. See also: Hormonal Contraception and the Risk of HIV Acquisition: An Individual Participant Data Meta-analysis. Charles S. Morrison1*, Pai-Lien Chen2, Cynthia Kwok2, Jared M. Baeten3, Joelle Brown4, Angela M. Crook5, Lut Van Damme6, Sinead Delany-Moretlwe7, Suzanna C. Francis8, Barbara A. Friedland9, Richard J. Hayes8, Renee Heffron3, Saidi Kapiga8, Quarraisha Abdool Karim10, Stephanie Karpoff11, Rupert Kaul12, R. Scott McClelland3, Sheena McCormack4, Nuala McGrath13, Landon Myer14, Helen Rees7, Ariane van der Straten15, Deborah Watson-Jones16, Janneke H. H. M. van de Wijgert17, Randy Stalter1, Nicola Low18. These 2 references represent the more recent meta-analyses that have tried to answer the controversial question of whether DMPA use increases HIV risk. Both papers found an approximate 50% increase in risk, which is having major policy considerations on a global level on how to balance the risk of HIV with that of unwanted pregnancy in much of the African region.
Murphy K, Irvin SC, Herold BC. Research gaps in defining the biological link between HIV risk and hormonal contraception. Am J Reprod Immunol. 2014;72:228–35.
Low N et al. Intravaginal practices, bacterial vaginosis, and HIV infection in women: individual participant data meta-analysis. PLoS Med. 2011;8:e1000416.
Hilber AM, Chersich MF, van de Wijgert JHHM, Rees H, Temmerman M. Vaginal practices, microbicides and HIV: what do we need to know? Sex Transm Infect. 2007;83:505–8.
Yi TJ, Shannon B, Prodger J, McKinnon L, Kaul R. Genital immunology and HIV susceptibility in young women. Am J Reprod Immunol. 2013;69 Suppl 1:74–9.
Mlisana K et al. Symptomatic vaginal discharge is a poor predictor of sexually transmitted infections and genital tract inflammation in high-risk women in South Africa. J Infect Dis. 2012;206:6–14.
Levinson P et al. Levels of innate immune factors in genital fluids: association of alpha defensins and LL-37 with genital infections and increased HIV acquisition. AIDS. 2009;23:309–17.
Morrison C et al. Cervical inflammation and immunity associated with hormonal contraception, pregnancy, and HIV-1 seroconversion. J Acquir Immune Defic Syndr. 2014;66:109–17.
Hwang LY, Scott ME, Ma Y, Moscicki A-B. Higher levels of cervicovaginal inflammatory and regulatory cytokines and chemokines in healthy young women with immature cervical epithelium. J Reprod Immunol. 2011;88:66–71.
Masson L, et al. Genital inflammation and the risk of HIV acquisition in women. Clin. Infect. Dis. 2015. doi:10.1093/cid/civ298. This represents the definitive paper on inflammation and HIV, showing that increased levels of pro-inflammatory cytokines in the female reproductive tract increased the risk of HIV acquisition. Importantly, many of these cytokines are found at higher levels in young women. This paper has had a broad influence on the field and has led to many follow-up efforts to better understand these data
Venkatesh KK, Cu-Uvin S. Assessing the relationship between cervical ectopy and HIV susceptibility: implications for HIV prevention in women. Am J Reprod Immunol. 2013;69 Suppl 1:68–73.
McLaren PJ et al. Association study of common genetic variants and HIV-1 acquisition in 6,300 infected cases and 7,200 controls. PLoS Pathog. 2013;9:e1003515.
Masson L, et al. Defining genital tract cytokine signatures of sexually transmitted infections and bacterial vaginosis in women at high risk of HIV infection: a cross-sectional study. Sex Transm Infect. 2014. doi:10.1136/sextrans-2014-051601. References [116•], [117•], and [118•] address the issue of altered microflora as a source of inflammation, finding similar signatures of bacterial-immune associations. While the causes of mucosal inflammation remain poorly defined, the common condition of abnormal flora appears a major contributor that is in need of better interventions.
Anahtar MN et al. Cervicovaginal bacteria are a major modulator of host inflammatory responses in the female genital tract. Immunity. 2015;42:965–76. References [116•], [117•], and [118•] address the issue of altered microflora as a source of inflammation, finding similar signatures of bacterial-immune associations. While the causes of mucosal inflammation remain poorly defined, the common condition of abnormal flora appears a major contributor that is in need of better interventions.
Kyongo JK et al. Cross-sectional analysis of selected genital tract immunological markers and molecular vaginal microbiota in sub-Saharan African women, with relevance to HIV risk and prevention. Clin Vaccine Immunol. 2015;22:526–38. References [116•], [117•], and [118•] address the issue of altered microflora as a source of inflammation, finding similar signatures of bacterial-immune associations. While the causes of mucosal inflammation remain poorly defined, the common condition of abnormal flora appears a major contributor that is in need of better interventions..
Rebbapragada A et al. Negative mucosal synergy between Herpes simplex type 2 and HIV in the female genital tract. AIDS. 2007;21:589–98.
Zhu J et al. Persistence of HIV-1 receptor-positive cells after HSV-2 reactivation is a potential mechanism for increased HIV-1 acquisition. Nat Med. 2009;15:886–92.
Marsden V et al. Herpes simplex virus type 2-infected dendritic cells produce TNF-α, which enhances CCR5 expression and stimulates HIV production from adjacent infected cells. J Immunol. 2015;194:4438–45.
Goode D et al. HSV-2-driven increase in the expression of α4β7 correlates with increased susceptibility to vaginal SHIV(SF162P3) infection. PLoS Pathog. 2014;10:e1004567.
Shannon B et al. Impact of asymptomatic herpes simplex virus type 2 infection on mucosal homing and immune cell subsets in the blood and female genital tract. J Immunol. 2014;192:5074–82.
Rollenhagen C, Lathrop MJ, Macura SL, Doncel GF, Asin SN. Herpes simplex virus type-2 stimulates HIV-1 replication in cervical tissues: implications for HIV-1 transmission and efficacy of anti-HIV-1 microbicides. Mucosal Immunol. 2014;7:1165–74.
Antonovics J et al. Biology and evolution of sexual transmission. Ann N Y Acad Sci. 2011;1230:12–24.
Phipps W et al. Persistent genital herpes simplex virus-2 shedding years following the first clinical episode. J Infect Dis. 2011;203:180–7.
Veldhuijzen NJ, Snijders PJ, Reiss P, Meijer CJ, van de Wijgert JH. Factors affecting transmission of mucosal human papillomavirus. Lancet Infect Dis. 2010;10:862–74.
Morrison CS et al. Hormonal contraception and HIV acquisition: reanalysis using marginal structural modeling. AIDS. 2010;24:1778–81.
Wira CR, Rodriguez-Garcia M, Patel MV. The role of sex hormones in immune protection of the female reproductive tract. Nat Rev Immunol. 2015;15:217–30.
McKinnon LR, et al. Risk Factors for HIV Acquisition in a Prospective Nairobi-Based Female Sex Worker Cohort. AIDS Behav. 2015. doi:10.1007/s10461-015-1118-7
Morris MR et al. Relationship of menstrual cycle and vaginal infection in female rhesus macaques challenged with repeated, low doses of SIVmac251. J Med Primatol. 2015;44:301–5.
Cortez V, Odem-Davis K, Lehman DA, Mabuka J, Overbaugh J. Quotidian changes of genital tract cytokines in human immunodeficiency virus-1-infected women during the menstrual cycle. Open Forum Infect Dis. 2014;1:ofu002.
Birse K et al. Molecular signatures of immune activation and epithelial barrier remodeling are enhanced during the luteal phase of the menstrual cycle: implications for HIV susceptibility. J Virol. 2015;89:8793–805.
Byrne EH, et al. Association between injectable progestin-only contraceptives and HIV acquisition and HIV target cell frequency in the female genital tract in South African women: a prospective cohort study. Lancet Infect Dis. 2015. doi:10.1016/S1473-3099(15)00429-6
Mitchell CM et al. Long-term effect of depot medroxyprogesterone acetate on vaginal microbiota, epithelial thickness and HIV target cells. J Infect Dis. 2014;210:651–5.
Francis SC et al. Immune activation in the female genital tract: expression profiles of soluble proteins in women at high risk for HIV infection. PLoS One. 2016;11:e0143109.
Deese J, et al. Injectable Progestin-Only Contraception is Associated With Increased Levels of Pro-Inflammatory Cytokines in the Female Genital Tract. Am J Reprod Immunol. 2015. doi:10.1111/aji.12415
Ngcapu S et al. Lower concentrations of chemotactic cytokines and soluble innate factors in the lower female genital tract associated with the use of injectable hormonal contraceptive. J Reprod Immunol. 2015;110:14–21.
Carias AM et al. Defining the interaction of HIV-1 with the mucosal barriers of the female reproductive tract. J Virol. 2013;87:11388–400.
Arnold KB, et al. Increased levels of inflammatory cytokines in the female reproductive tract are associated with altered expression of proteases, mucosal barrier proteins, and an influx of HIV-susceptible target cells. Mucosal Immunol. 2015. doi:10.1038/mi.2015.51. This paper used proteomic techniques to describe linkages between the mucosal barrier, HIV target cells, and inflammatory cytokines in the female reproductive tract. These data raise many hypotheses regarding mechanisms of how these processes might be linked to increase the odds of HIV transmission during exposure.
Noguchi LM et al. Risk of HIV-1 acquisition among women who use diff erent types of injectable progestin contraception in South Africa: a prospective cohort study. Lancet HIV. 2015;2:e279–87. This is the first large study able to address the differences in HIV risk posed by DMPA and NET-EN, a similar but distinct form of contraception. Interestingly, HSV2 serostatus had a big impact on the difference between these two forms of contraception, suggesting that this virus might play some role in exacerbating DMPA’s mucosal impact.
Grabowski MK et al. Use of injectable hormonal contraception and women’s risk of herpes simplex virus type 2 acquisition: a prospective study of couples in Rakai, Uganda. Lancet Glob Health. 2015;3:e478–86.
Kaul R et al. Prevalent herpes simplex virus type 2 infection is associated with altered vaginal flora and an increased susceptibility to multiple sexually transmitted infections. J Infect Dis. 2007;196:1692–7.
Roxby AC et al. Changes in vaginal microbiota and immune mediators in HIV-1-seronegative Kenyan Women initiating depot medroxyprogesterone acetate. J Acquir Immune Defic Syndr. 2016;71:359–66.
Fichorova RN et al. The Contribution of Cervicovaginal Infections to the Immunomodulatory Effects of Hormonal Contraception. MBio. 2015;6:e00221–15. This very large cohort analysis demonstrates how mucosal associations can be dependent on other co-factors present in the same women. Importantly the sample size provided power to investigate these in greater detail than was previously available.
Eaton JW et al. Recent HIV prevalence trends among pregnant women and all women in sub-Saharan Africa: implications for HIV estimates. AIDS. 2014;28 Suppl 4:S507–14.
Santelli JS et al. Trends in HIV acquisition, risk factors and prevention policies among youth in Uganda, 1999–2011. AIDS. 2015;29:211–9.
Katz IT, Bassett IV, Wright AA. PEPFAR in transition—implications for HIV care in South Africa. N Engl J Med. 2013;369:1385–7.
Stover J et al. How can we get close to zero? The potential contribution of biomedical prevention and the investment framework towards an effective response to HIV. PLoS One. 2014;9:e111956.
Karim SSA, Karim QA. Antiretroviral prophylaxis: a defining moment in HIV control. Lancet. 2011;378:e23–5.
Baeten JM, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med 2016. doi:10.1056/NEJMoa1506110. While this very recent paper provides more good news for the HIV prevention field, it is once again worrying that adherence may be an important barrier, especially for young women, in order for interventions such as dapivurine ring to realize their full potential.
Kapogiannis BG, Handelsman E, Ruiz MS, Lee S. Introduction: paving the way for biomedical HIV prevention interventions in youth. J Acquir Immune Defic Syndr. 2010;54 Suppl 1:S1–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Lyle R. McKinnon and Quarraisha Abdool Karim declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on The Global Epidemic
Rights and permissions
About this article
Cite this article
McKinnon, L.R., Karim, Q.A. Factors Driving the HIV Epidemic in Southern Africa. Curr HIV/AIDS Rep 13, 158–169 (2016). https://doi.org/10.1007/s11904-016-0314-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-016-0314-z