Abstract
Purpose of Review
Managing nutrition in individuals with advanced liver disease is an integral part of their care and can significantly impact their morbidity and mortality. The aim of this review study is to focus on the etiology of malnutrition in end-stage liver disease, screening and assessment methods of these individuals, and providing evidenced-based recommendations on the proper nutritional interventions.
Recent Findings
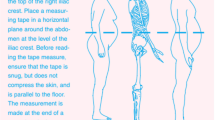
The etiology of malnutrition in advanced liver disease is multifactorial but can be described as the effects of a chronic catabolic illness accompanied by decreased food intake. In order to determine the necessary steps of intervention, adequate screening for malnutrition much first be conducted. Assessment for malnutrition should include a review of biochemical markers, a diet history, and a physical assessment including subjective global assessment, handgrip strength, anthropometric measures, and body composition testing. Interventions for these individuals range from diet education to enteral/parenteral feedings, depending on the degree of malnutrition.
Summary
All patients diagnosed with advanced liver disease should have their nutrition status promptly assessed. Once assessed, they should be educated by a registered dietitian nutritionist to help better their quality of life and to prevent any nutrition-related medical complications. As their disease progresses and their condition worsens, they should be continually evaluated for treatment plan adjustments as needed.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Italian Multicentre Cooperative Project on nutrition in liver cirrhosis. Nutritional status in cirrhosis. J Hepatol. 1994;21:317–25.
Figuerido FA, Perez De Mello R, Kondo M. Effect of liver cirrhosis on body composition: evidence of significant depletion even in mild disease. J Gastroenterl Hepatol. 2005;20:209–16.
Ma Z, Zhang Y, Huet PM, Lee SS. Differential effects of jaundice and cirrhosis on beta-adrenoceptor signaling in three rat models of cirrhotic cardiomyopathy. J Hepatol. 1999;30:485–91.
Campillo B, Richardet JP, Scherman E, et al. Evaluation of nutritional practice in hospitalized cirrhotic patients: results of a prospective study. Nutrition. 2003;19(6):515–21.
Sobhonslidsuk A, Roongpisuthipong C, Nantiruj K, Kulapongse S, Songchitsomboon S, Sumalnop K, et al. Impact of liver cirrhosis on nutritional and immunological status. J Med Assoc Thail. 2001;84:982–8.
Cheung K, Lee SS, Raman M. Prevalence and mechanisms of malnutrition in patients with advanced liver disease, and nutrition management strategies. Clin Gastroenterol Hepatol. 2012;10:117–25.
Testa R, Franceschini R, Giannini E, Cataldi A, Botta F, Fasoli A, et al. Serum leptin levels in patients with viral chronic hepatitis or liver cirrhosis. J Hepatol. 2000;33(1):33–7.
Kalaitzakis E, Simrén M, Olsson R, Henfridsson P, Hugosson I, Bengtsson M, et al. Gastrointestinal symptoms in patients with liver cirrhosis: associations with nutritional status and health-related quality of life. Scand J Gastroenterol. 2006;41:1464–72.
Tsiaousi ET, Hatzitolios AI, Trygonis SK, Savopoulos CG. Malnutrition in end stage liver disease: recommendations and nutritional support. J Gastroenterol Hepatol. 2008;23(4):527–33.
Yamanaka H, Genjida K, Yokota K, Taketani Y, Morita K, Miyamoto KI, et al. Daily pattern of energy metabolism in cirrhosis. Nutrition. 1999;15:749–54.
Changani KK, Jalan R, Cox IJ, et al. Evidence for altered hepatic gluconeogenesis in patients with cirrhosis using in vivo 31-phosphorus magnetic resonance spectroscopy. Gut. 2001;49:557–64.
Charlton MR. Protein metabolism and liver disease. Bailliere Clin Endocrinol Metab. 1996;10:617–35.
Rasmussen HH, Irtun Ø, Olesen SS, Drewes AM, Holst M. Nutrition in chronic pancreatitis. World J Gastroenterol. 2013;19(42):7267–75.
Koivisto M, Valta P, Höckerstedt K, Lindgren L. Magnesium depletion in chronic terminal liver cirrhosis. Clin Transpl. 2002;16:325–8.
• Sengupta S, Wroblewski K, Aronsohn A, et al. Screening for zinc deficiency in patients with cirrhosis: When should we start? Dig Dis Sci. 2015;60(10):3130-5. Study on zinc deficiency in cirrhotics which correlates with disease severity, infection, and worse transplant-free outcomes.
Mohammad MK, Zhou Z, Cave M, et al. Zinc and liver disease. Nutr Clin Pract. 2012;27(1):8–20.
Yoshida Y, Higashi T, Nouso K, Nakatsukasa H, Nakamura SI, Watanabe A, et al. Effects of zinc deficiency/zinc supplementation on ammonia metabolism in patients with decompensated liver cirrhosis. Acta Med Okayama. 2001;55:349–55.
• Eghtesad S, Poustchi H, Malekzadeh R. Malnutrition in liver cirrhosis: the influence of protein and sodium. Middle East J Dig Dis. 2013;5:65–75. Review paper focusing on protein-calorie malnutrition in cirrhosis and the important role of protein and sodium.
Qin H, Li H, Xing M, Wu C, Li G, Song J. Nutritional support treatment for severe chronic hepatitis and posthepatitic cirrhosis. J Huazhong Univ Sci Technolog Med Sci. 2006;26(2):217–20.
Merli M, Giusto M, Giannelli V, Lucidi C, Riggio O. Nutritional status and liver transplantation. J Clin Exp Hepatol. 2011;1:190–8.
•• Frazier TH, Wheeler BE, McClain CJ, Cave, M. Liver Disease. In: Mueller CM, ed. The A.S.P.E.N. nutrition support core curriculum, 2nd ed. Silver Spring, MD: American Society of Parenteral and Enteral Nutrition. 2012: 454-471. Consensus from the American Society of Parenteral and Enterall Nutrition on how to nutritionally manage patients with liver disease.
Ferguson M, Capra S, Bauer J, et al. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition. 1999;15:458–64.
•• Plauth M, Cabre E, Riggio O, et al. ESPEN guidelines on enteral nutrition: liver disease. Eur Soc Clin Nutr Metab. 2006;25:285–94. Guidelines from European Society for Parenteral and Enteral Nutrition, specifically for assessing the nutritional status of those with liver disease.
•• Hasse J, Strong S, Gorman MA, Liepa G. Subjective global assessment: alternative nutrition-assessment technique for liver-transplant candidates. Nutrition. 1993;9:339–43. Registered dietitian-led study that focused on the subjective global assessment, the gold standard for nutritional assessment among liver disease patients. Raters agreed on nutrition status 80% of the time.
Makhija S, Baker J. The subjective global assessment: a review of its use in clinical practice. Nutr Clin Pract. 2008;23(4):405–9.
Baker JP, Detsky AS, Wasson DE, et al. Nutritional assessment: a comparison of clinical judgment and objective measurements. N Engl J Med. 1982;306:969–72.
Alvares-da-Silva NR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21:113–7.
Figueiredo FA, Perez RM, Freitas MM, Kondo M. Comparison of three methods of nutritional assessment in liver cirrhosis: subjective global assessment, traditional nutritional parameters, and body composition analysis. J Gastroenterol. 2006;41:476–82.
Massy-Westropp NMM, Gill TK, Taylor AW, Bohannon RW, Hill CW. Handgrip strength: age and gender stratified normative data in a population-based study. BMC Research Notes. 2011;4:127.
Klinijian AM, Foster KJ, Kammerling RM, Cooper A, Karran SJ. Relation of anthropometric and dynamometric variables to serious postoperative complications. Br Med J. 1980;281:899.
• Chanpiwat K, Bunchorntavakul C. Nutritional assessment in patients with cirrhosis: comparison between different methods. Thai J Gastroenterol. 2014;15(2):90–8. Study comparing different methods of assessing nutritional status of patients with cirrhosis; Mid-arm-muscle circumference found to be superior to subjective global assessment, handgrip strength, and bioelectrical impedance analysis.
Guglielmi FW, Contento F, Laddaga L, Panella C, Francavilla A. Bioelectric impedance analysis: experience with male patients with cirrhosis. Hepatology. 1991;13:892–5.
Panella C, Guglielmi FW, Mastronuzzi T, Francavilla A. Whole-body and segmental bioelectrical parameters in chronic liver disease: effect of gender and disease stages. Hepatology. 1995;21:352–8.
• Romeiro FG, Augusti L. Nutritional assessment in cirrhotic patients with hepatic encephalopathy. World J Hepatol. 2015;7:2940–54. Review article focusing on how hepatic encephalopathy and severely impact nutritional status. Includes informative review on how to use CT scan in assessing lean mass depletion.
• DiMartini A, Cruz RJ, Dew MA, Myaskovsky L, Goodpaster B, Fox K, et al. Muscle mass predicts outcomes following liver transplantation. Liver Transpl. 2013;19:1172–80. Study using CT scan data of 338 liver transplant candidates that found the majority (68%) were cachectic.
Chutaputti A. Advances in liver disease: alcoholic hepatitis, noncirrhotic portal fibrosis and complications of cirrhosis. J Gastroenterol Hepatol. 2002;17:456–46.
Cordoba J, Lopez-Hellin J, Planas M, et al. Normal protein diet for episodic hepatic encephalopathy: results of a randomized study. J Hepatol. 2004;41:38–43.
•• European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010; 397-417. doi:10.1016/j.jhep.2010.05.004. Recommendation for sodium intake between 1840-2760mg slightly higher than typical recommendation of 1500-2000mg/day.
Gauthier A, Levy VG, Quinton A, Michel H, Rueff B, Descos L, et al. Salt or no salt in the treatment of cirrhotic ascites: a randomised study. Gut. 1986;27:705–9.
Swart GR, Zillikens MC, van Vuure JK, van den Berg JW. Effect of a late evening meal on nitrogen balance in patients with cirrhosis of the liver. BMJ. 1989;299:1202–3.
Hidaka H, Nakazawa T, Kutsukake S, Yamazaki Y, Aoki I, Nakano S, et al. The efficacy of nocturnal administration of branched-chain amino acid granules to improve quality of life in patients with cirrhosis. J Gastroenterol. 2013;48:269–76.
Verboeket-van de Venne WP, Westerterp KR, van Hoek B, Swart GR. Energy expenditure and substrate metabolism in patients with cirrhosis of the liver: effects of the pattern of food intake. Gut. 1995;36:110–6.
Arteh J, Narra S, Nair S. Prevalence of vitamin D deficiency in chronic liver disease. Dig Dis Sci. 2010;55(9):2624–8.
• Finkelmeier F, Kronenberger B, Zeuzem S, et al. Low 25-hydroxyvitamin D levels are associated with infections and mortality in patients with cirrhosis. PLoS One. 2015;10(6):e0132119. doi:10.1371/journal.pone.0132119. Patients with decompensated cirrhosis and infectious complications had significantly lower vitamin D levels compared to subjects without complications.
• Vidot H, Potter A, Cheng R, Allman-Farinelli M, Shackel N. Serum 25-hydroxyvitamin D deficiency and hepatic encephalopathy in chronic liver disease. World J Hepatol. 2017;9(10):510–8. doi:10.4254/wjh.v9.i10.510. A restrospecitve analysis that found a significant correlation between vitamin D deficiency and severity of liver disease and the presence of hepatic encephalopathy.
Abbott-Johnson W, Kerlin P, Clague A, et al. Relationships between blood levels of fat soluble vitamins and disease etiology and severity in adults awaiting liver transplantation. J Gastroenterol Hepatol. 2011;26:1402–10.
Rabbani P, Prasad AS. Plasma ammonia and liver ornithine transcarbamoylase activity in zinc-deficient rats. Am J Phys. 1978;235:E203–6.
Takuma Y, Nouso K, Makino Y, Hayashi M, Takahashi H. Clinical trial: oral zinc in hepatic encephalopathy. Aliment Pharmacol Ther. 2010;32:1080–90.
Marchesini G, Bianchi G, Merli M, Amodio P, Panella C, Loguercio C, et al. Nutritional supplementation with branched-chain amino acids in advanced cirrhosis: a double-blind, randomized trial. Gastroenterology. 2003;124:1792–801.
Iwasa J, Shimizu M, Shiraki M, et al. Dietary supplementation with branched-chain amino acids suppresses diethylnitrosamine-induced liver tumorigenesis in obese and diabetic C57BL/KsJ-db/db mice. Cancer Sci. 2010;101:460–7.
Kawaguchi T, Izumi N, Charlton MR, Sata M. Branched-chain amino acids as pharmacological nutrients in chronic liver disease. Hepatology. 2011;54:1063–70.
Muto Y, Sato S, Watanabe A, Moriwaki H, Suzuki K, Kato A, et al. Overweight and obesity increase the risk for liver cancer in patients with liver cirrhosis and long-term oral supplementation with branched-chain amino acid granules inhibits liver carcinogenesis in heavier patients with liver cirrhosis. Hepatol Res. 2006;35:204–14.
Lunia MK, Sharma BC, Sharma P, Sachdeva S, Srivastava S. Probiotics prevent hepatic encephalopathy in patients with cirrhosis: a randomized controlled trial. Clin Gastroenterol Hepatol. 2014;12:1003–8.
Kwarta E, Nagle S, Welstead L. Update on malnutrition in liver cirrhosis: assessment and treatment. Curr Hepatol Rep. 2014;13:24–34.
Swart DR, Van DBJ, Wattimena JL, et al. Elevated protein requirements in cirrhosis of the liver investigated by whole body protein turnover. Clin Sci. 1988;75:101–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Annie Grochocinski, Alissa Dandalides, and Lauren Remley declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
This article is part of the Topical Collection on Management of the Cirrhotic Patient
Rights and permissions
About this article
Cite this article
Grochocinski, A., Dandalides, A. & Remley, L. Nutrition for the Patient with Advanced Liver Disease. Curr Hepatology Rep 16, 205–211 (2017). https://doi.org/10.1007/s11901-017-0354-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11901-017-0354-x