Abstract
Purpose of the Work
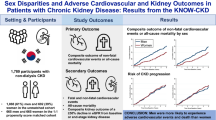
Although sex-specific differences in heart failure (HF) or kidney disease (KD) have been analyzed separately, the predominant cardiorenal phenotype by sex has not been described. This study aims to explore the sex-related differences in cardiorenal syndrome (CRS) in a contemporary cohort of outpatients with HF.
Findings
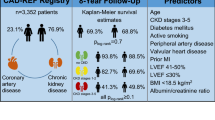
An analysis of the Cardiorenal Spanish registry (CARDIOREN) was performed. CARDIOREN Registry is a prospective multicenter observational registry including 1107 chronic ambulatory HF patients (37% females) from 13 Spanish HF clinics. Estimated Glomerular Filtration Rate (eGFR) < 60 ml/min/1.73 m2 was present in 59.1% of the overall HF population, being this prevalence higher in the female population (63.2% vs. 56.6%, p = 0.032, median age: 81 years old, IQR:74–86). Among those with kidney dysfunction, women displayed higher odds of showing HF with preserved ejection fraction (HFpEF) (odds ratio [OR] = 4.07; confidence interval [CI] 95%: 2.65–6.25, p < 0.001), prior valvular heart disease (OR = 1.76; CI 95%:1.13–2.75, p = 0.014), anemia (OR: 2.02; CI 95%:1.30–3.14, p = 0.002), more advanced kidney disease (OR for CKD stage 3: 1.81; CI 95%:1.04–3.13, p = 0.034; OR for CKD stage 4: 2.49, CI 95%:1.31–4.70, p = 0.004) and clinical features of congestion (OR:1.51; CI 95%: 1.02–2.25, p = 0.039). On the contrary, males with cardiorenal disease showed higher odds of presenting HF with reduced ejection fraction (HFrEF) (OR:3.13; CI 95%: 1.90–5.16, p < 0.005), ischemic cardiomyopathy (OR:2.17; CI 95%: 1.31–3.61, p = 0.003), hypertension (OR = 2.11; CI 95%:1.18–3.78, p = 0.009), atrial fibrillation (OR:1.71; CI 95%: 1.06–2.75, p = 0.025), and hyperkalemia (OR:2.43, CI 95%: 1.31–4.50, p = 0.005).
Summary
In this contemporary registry of chronic ambulatory HF patients, we observed sex-related differences in patients with combined heart and kidney disease. The emerging cardiorenal phenotype characterized by advanced CKD, congestion, and HFpEF was predominantly observed in women, whereas HFrEF, ischemic etiology, hypertension, hyperkalemia, and atrial fibrillation were more frequently observed in men.



Similar content being viewed by others
Data Availability
The raw data supporting the conclusion of this article will be made available by the authors, under request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Ventura-Clapier R, Dworatzek E, Seeland U, Kararigas G, Arnal JF, Brunelleschi S, et al. Sex in basic research: concepts in the cardiovascular field. Cardiovasc Res [Internet]. 2017 [cited 2022 Nov 28];113(7):711–24. Available from: https://pubmed.ncbi.nlm.nih.gov/28472454/.
Carrero JJ, Hecking M, Chesnaye NC, Jager KJ. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol [Internet]. 2018 [cited 2022 Dec 4];14(3):151–64. Available from: https://pubmed.ncbi.nlm.nih.gov/29355169/.
Merrill M, Sweitzer NK, Lindenfeld JA, Kao DP. Sex Differences in Outcomes and Responses to Spironolactone in Heart Failure With Preserved Ejection Fraction: A Secondary Analysis of TOPCAT Trial. JACC Heart Fail [Internet]. 2019 [cited 2022 Dec 4];7(3):228–38. Available from: https://pubmed.ncbi.nlm.nih.gov/30819379/.
Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol [Internet]. 2008 [cited 2022 Dec 4];52(19):1527–39. Available from: https://pubmed.ncbi.nlm.nih.gov/19007588/.
Tedeschi A, Agostoni P, Pezzuto B, Corra’ U, Scrutinio D, la Gioia R, et al. Role of comorbidities in heart failure prognosis Part 2: Chronic kidney disease, elevated serum uric acid. Eur J Prev Cardiol [Internet]. 2020 [cited 2022 Dec 4];27(2_suppl):35–45. Available from: https://pubmed.ncbi.nlm.nih.gov/33238740/.
Núñez J, Miñana G, Santas E, Bertomeu-González V. Cardiorenal Syndrome in Acute Heart Failure: Revisiting Paradigms. Rev Esp Cardiol (Engl Ed) [Internet]. 2015 [cited 2022 Dec 4];68(5):426–35. Available from: https://pubmed.ncbi.nlm.nih.gov/25758162/.
di Lullo L, Bellasi A, Barbera V, Russo D, Russo L, di Iorio B, et al. Pathophysiology of the cardio-renal syndromes types 1–5: An uptodate. Indian Heart J [Internet]. 2017 [cited 2022 Dec 4];69(2):255–65. Available from: https://pubmed.ncbi.nlm.nih.gov/28460776/.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med [Internet]. 2013 [cited 2022 Dec 4];158(11):825–30. Available from: https://pubmed.ncbi.nlm.nih.gov/23732715/.
Dewan P, Rørth R, Jhund PS, Shen L, Raparelli V, Petrie MC, et al. Differential Impact of Heart Failure With Reduced Ejection Fraction on Men and Women. J Am Coll Cardiol [Internet]. 2019 [cited 2022 Dec 4];73(1):29–40. Available from: https://pubmed.ncbi.nlm.nih.gov/30621948/.
Omote K, Verbrugge FH, Borlaug BA. Heart Failure with Preserved Ejection Fraction: Mechanisms and Treatment Strategies. Annu Rev Med [Internet]. 2022 [cited 2022 Dec 4];73:321–37. Available from: https://pubmed.ncbi.nlm.nih.gov/34379445/.
Salamanca-Bautista P, Álvarez-García J, Aramburu-Bodas Ó, Ferrero-Gregori A, Arias-Jiménez JL, Delgado JF, et al. Modes of death in heart failure according to age, sex and left ventricular ejection fraction. Intern Emerg Med [Internet]. 2021 [cited 2022 Dec 4];16(3):643–52. Available from: https://pubmed.ncbi.nlm.nih.gov/32813117/.
de Bellis A, de Angelis G, Fabris E, Cannatà A, Merlo M, Sinagra G. Gender-related differences in heart failure: beyond the “one-size-fits-all” paradigm. Heart Fail Rev [Internet]. 2020 [cited 2022 Dec 9];25(2):245–55. Available from: https://pubmed.ncbi.nlm.nih.gov/31267323/.
• Lam CSP, Arnott C, Beale AL, Chandramouli C, Hilfiker-Kleiner D, Kaye DM, et al. Sex differences in heart failure. Eur Heart J. 2019;40(47):3859–68. Review that outlines the key sex differences with respect to clinical characteristics, pathophysiology, and therapeutic responses to HF treatment.
Wetzels JFM, Willems HL, Heijer M den. Age- and gender-specific reference values of estimated glomerular filtration rate in a Caucasian population: Results of the Nijmegen Biomedical Study. Kidney Int [Internet]. 2008 [cited 2022 Dec 4];73(5):657–8. Available from: https://pubmed.ncbi.nlm.nih.gov/18274547/.
Inker LA, Levey AS, Tighiouart H, Shafi T, Eckfeldt JH, Johnson C, et al. Performance of glomerular filtration rate estimating equations in a community-based sample of Blacks and Whites: the multiethnic study of atherosclerosis. Nephrol Dial Transplant [Internet]. 2018 [cited 2022 Dec 4];33(3):417–25. Available from: https://pubmed.ncbi.nlm.nih.gov/28505377/.
de la Espriella R, Navarro J, Mollar A, D’Marco L, Palau P, Miñana G, et al. Long-Term Prognostic Impact of Estimated Glomerular Filtration Rate on Admission in Patients Hospitalized for Acute Heart Failure. Cardiorenal Med [Internet]. 2022 [cited 2022 Dec 4];12(4):179–88. Available from: https://pubmed.ncbi.nlm.nih.gov/36282062/.
Mascarenhas J, Laszczynska O, Severo M, Friões F, Alvelos M, Bettencourt P, et al. Prognostic Effect of Renal Function in Ambulatory Patients With Heart Failure and Reduced Ejection Fraction: The Kidney Is a Marker of Cardiac Function. Can J Cardiol [Internet]. 2018 [cited 2022 Dec 4];34(10):1325–32. Available from: https://pubmed.ncbi.nlm.nih.gov/30201253/.
Smith DH, Thorp ML, Gurwitz JH, McManus DD, Goldberg RJ, Allen LA, et al. Chronic kidney disease and outcomes in heart failure with preserved versus reduced ejection fraction: the Cardiovascular Research Network PRESERVE Study. Circ Cardiovasc Qual Outcomes [Internet]. 2013 [cited 2022 Dec 4];6(3):333–42. Available from: https://pubmed.ncbi.nlm.nih.gov/23685625/.
Gevaert AB, Kataria R, Zannad F, Sauer AJ, Damman K, Sharma K, et al. Heart failure with preserved ejection fraction: recent concepts in diagnosis, mechanisms and management. Heart [Internet]. 2022 [cited 2022 Dec 4];108(17):1342–50. Available from: https://pubmed.ncbi.nlm.nih.gov/35022210/.
• ter Maaten JM, Damman K, Verhaar MC, Paulus WJ, Duncker DJ, Cheng C, et al. Connecting heart failure with preserved ejection fraction and renal dysfunction: the role of endothelial dysfunction and inflammation. Eur J Heart Fail [Internet]. 2016 [cited 2022 Dec 4];18(6):588–98. Available from: https://pubmed.ncbi.nlm.nih.gov/26861140/. Review the role of endothelial dysfunction and inflammation to explain the link between renal dysfunction and HFpEF.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol [Internet]. 2016 [cited 2022 Dec 4];16(10):626–38. Available from: https://pubmed.ncbi.nlm.nih.gov/27546235/.
Inanloorahatloo K, Liang G, Vo D, Ebert A, Nguyen I, Nguyen PK. Sex-based differences in myocardial gene expression in recently deceased organ donors with no prior cardiovascular disease. PLoS One [Internet]. 2017 [cited 2022 Dec 4];12(8). Available from: https://pubmed.ncbi.nlm.nih.gov/28850583/.
Patel RB, Fonarow GC, Greene SJ, Zhang S, Alhanti B, DeVore AD, et al. Kidney Function and Outcomes in Patients Hospitalized With Heart Failure. J Am Coll Cardiol [Internet]. 2021 [cited 2022 Dec 8];78(4):330–43. Available from: https://pubmed.ncbi.nlm.nih.gov/33989713/.
Janse RJ, Fu EL, Dahlström U, Benson L, Lindholm B, van Diepen M, et al. Use of guideline-recommended medical therapy in patients with heart failure and chronic kidney disease: from physician’s prescriptions to patient’s dispensations, medication adherence and persistence. Eur J Heart Fail [Internet]. 2022 [cited 2022 Dec 8]; Available from: https://pubmed.ncbi.nlm.nih.gov/35851740/.
• de la Espriella R, Marcos MC, Ronco C, Banerjee D, González M, Górriz JL, et al. Practical approaches to building up a cardiorenal clinic. Clin Kidney J [Internet]. 2022 [cited 2022 Dec 8]; Available from: https://doi.org/10.1093/ckj/sfac258/6881385.Document that defines the organizational aspects and the key elements for setting up a multidisciplinary cardiorenal clinical program.
Acknowledgements
The editors would like to thank Dr. Eduardo Zatarain for taking the time to handle the review of this manuscript.
Funding
Supported by AstraZeneca Farmacéutica Spain, S.A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All the authors report grants from Astra Zeneca during the conduct of the study. Dr. Cobo Marcos reports personal fees from ASTRA ZENECA, VIFOR PHARMA, NOVARTIS, ROVI, BOEHRINGHER INGELHEIM, NOVONORDISK, ESTEVE and BAYER; Dr Pomares reports personal fees from PFIZER, and support for attending meetings from NOVARTIS AND BAYER, Dr Méndez reports personal fees from ASTRA ZENECA, support for attending meetings from NOVARTIS, and participation on a Data Safety Monitoring Board or Advisory Board from BAYER; Dr Rubio reports personal fees from ASTRA ZENECA, NOVARTIS, BOEHRINGHER INGELHEIM, ESTEVE, and BAYER; Dr Recio reports personal fees from ASTRA ZENECA, NOVARTIS, BOEHRINGHER INGELHEIM, JANSSEN, BAYER, MSD and support for attending meetings from BAYER, MSD and NOVARTIS;. Dr Garía Pinilla reports personal fees from ASTRA ZENECA, VIFOR PHARMA, NOVARTIS, BOEHRINGHER INGELHEIM, PFIZER and BAYER, Dr Soler Romeo reports personal fees from NovoNordisk, Jansen, Boehringer, Mundipharma, Esteve, Fresenius, Ingelheim Lilly, Vifor, ICU Medical, Travere Therapeutics, GE Healthcare, grants and personal fees from AstraZeneca, Editor in Chief of CKJ; In addition, Dr. Soler Romeo has a patent 202131356 issued; Dr Núñez reports, grants from VIFOR PHARMA, personal fees from NOVARTIS, ROVI, BOEHRINGHER INGELHEIM, NOVONORDISK and BAYER. All other authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11897_2023_598_MOESM1_ESM.docx
Supplementary file 1 Sex stratified basal characteristics across kidney disease categories. eGFR: estimated glomerular filtration rate; COPD, chronic obstructive pulmonary disease; HF: heart failure; BMI: body mass index; NYHA, New York Heart Association; SBP: systolic blood pressure; DBP: diastolic blood pressure; LVEF: left ventricular ejection fraction; LVH: left ventricular hypertrophy; TAPSE: tricuspid annular plane systolic excursion; sPAP: systolic pulmonary artery pressure; NTproBNP: N-terminal pro-brain natriuretic peptide; CA125: cancer antigen 125; ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor blockers; MRA: mineralocorticoids receptor antagonists; SLGT2i: Sodium-glucose cotransporter inhibitors; IV: intravenous; ESA: erythropoiesis-stimulating agent; VKa: Vitamin K antagonists; DOACs: Direct oral anticoagulants. * Values expressed as median (interquartile range). Ç Defined as serum ferritin <100 ng/mL or, serum ferritin 100-299 ng/mL + transferrin saturation <20%. Data available in 1020 patients. † Last 3 months (DOCX 41 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cobo Marcos, M., de la Espriella, R., Gayán Ordás, J. et al. Sex differences in Cardiorenal Syndrome: Insights from CARDIOREN Registry. Curr Heart Fail Rep 20, 157–167 (2023). https://doi.org/10.1007/s11897-023-00598-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-023-00598-x