Abstract
Purpose of Review
The prevalence of cancer therapy-related cardiac dysfunction (CTRCD) is increasing due to improved cancer survival. Serial monitoring of cardiac function is essential to detect CTRCD, guiding timely intervention strategies. Multigated radionuclide angiography (MUGA) has been the main screening tool using left ventricular ejection fraction (LVEF) to monitor cardiac dysfunction. However, transthoracic echocardiography (TTE) and cardiac magnetic resonance imaging (CMR) may be more suitable for serial assessment. We aimed to assess the concordance between different non-radiating imaging modalities with MUGA to determine whether they can be used interchangeably.
Recent Findings
In order to identify relevant studies, a PubMed search was performed. We included cross-sectional studies comparing MUGA LVEF to that of 2D TTE, 3D TTE, and CMR. From 470 articles, 22 were selected, comprising 1017 patients in total. Among others, this included three 3D TTE, seven 2D harmonic TTE + contrast (2DHC), and seven CMR comparisons. The correlations and Bland-Altman limits of agreement varied for CMR but were stronger for 3D TTE and 2DHC.
Summary
Our findings suggest that MUGA and CMR should not be used interchangeably whereas 3D TTE and 2DHC are appropriate alternatives following an initial MUGA scan. We propose a multimodality diagnostic imaging strategy for LVEF monitoring in patients undergoing cancer treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer treatment has become more effective over the past decades, resulting in increasing numbers of cancer survivors globally [1]. Unfortunately, cancer treatment can lead to cancer therapy-related cardiac dysfunction (CTRCD) due to its direct and indirect cardiotoxic effects, such as ischemia, hypertension, and vascular and metabolic dysregulation [2]. The resulting cardiomyocyte damage and dysfunction can in turn lead to congestive heart failure [3]. In this manner, cardiovascular complications resulting from cancer treatment contribute greatly to the global burden of cardiovascular disease and represent a leading cause of death in cancer survivors [1, 3,4,5]. While the progressive decline in cardiac function due to cancer treatment can occur up to 20 years after treatment, research has shown that it can be prevented or ameliorated through early monitoring, continued cardiac surveillance during and after treatment, and timely intervention [6].
According to the European Society of Cardiology (ESC), the optimal parameter of cardiac function assessment in the field of cardio-oncology is left ventricular ejection fraction (LVEF). The ESC defines CTRCD as a decrease in LVEF by more than 10 percentage-points below the value of 53%, which is the normal reference value of two-dimensional echocardiography (2D TTE), or below 50%, which is the lower limit of normal for multigated acquisition (MUGA) scan [7, 8]. Timely interruption of cancer treatment and/or early initiation of cardioprotective treatment is often necessary to impede further LVEF decline and optimize the possibility of LVEF recovery in asymptomatic cardiac dysfunction [3, 9]. Therefore, serial cardiac monitoring using the optimal method of imaging is crucial.
MUGA became popular in the 1970s when researchers were trying to identify patients with a decline in LVEF prior to heart failure symptoms [7]. To date, the MUGA scan is being used in clinical settings for LVEF monitoring due to its high reproducibility, low variability, and few technical limitations. Two main disadvantages are its lack in ability to evaluate structural and functional abnormalities beyond LVEF and its exposure of patients to additional ionizing radiation [7, 10]. The effect of cumulative radiation is feared, especially so for the long-term consequences it may have for young patients [4]. Consequently, implementation of an alternative imaging modality is desired.
The ESC and EACVI advise to first and foremost use echocardiography for the serial assessment of LVEF in patients at risk for CTRCD [7, 8]. Three-dimensional echocardiography (3D TTE) is preferred as its lack of reliance on geometrical assumptions and its ability to provide a scan of the entire left ventricular cavity yield highly accurate and reproducible results [11, 12]. Alternatively, cardiac magnetic resonance (CMR) imaging is considered the current gold standard for left and right ventricular volumes and their function due to its clear and reliable measurements [7, 13].
Within cardio-oncological screening, multiple cardiac imaging modalities are interchangeably used due to an unexpected necessity of alternative imaging modalities (e.g., in patients where TTE becomes unsuitable for LVEF follow-up after a left-sided mastectomy). The ability of different imaging modalities to yield accurate and, most importantly, comparable results remains to be fully determined. This is relevant for improving patient care as changes in cancer treatment based on inaccurate LVEF evaluations can have severe consequences [6]. Therefore, this systematic review aims to assess the interchangeability of MUGA with other cardiac imaging modalities.
Methods
This systematic review was performed in accordance with the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [14]. A comprehensive PubMed search was performed and updated on January 17, 2022 using the search query listed in Supplemental Table 1. This list consists of synonyms for the MUGA scan, each of the reference tests and LVEF. Additionally, the following filters were applied: humans, adults (≥18 years old), and English language. The reference lists of all selected papers were hand searched and relevant studies were included.
This systematic review includes cross-sectional studies comparing LVEF measurements of the MUGA scan with at least one of the appropriate reference tests: contrast angiography, 2D TTE, 3D TTE, CMR, and thermodilution (TD). For 2D TTE, reporting of the biplane method of disks, or modified Simpson’s rule, was a requirement. Papers assessing LVEF by visual assessment only were excluded. Additionally, since harmonic 2D TTE provides images of superior quality to fundamental imaging, only harmonic 2D TTE was used for the analysis in studies reporting both harmonic and fundamental images [15]. However, if the study only researched fundamental 2D TTE, it was still included. For the final analysis, we considered the different echocardiographic techniques (fundamental, harmonic, harmonic with contrast, and 3D) as separate [16]. We excluded ionizing imaging modalities, such as computed tomography (CT) and single-positron emission computed tomography (SPECT). No distinctions were made between different MUGA techniques, such as first-pass MUGA and planar MUGA [17]. Articles were included based on their abstracts and full text availability as well as the following inclusion criteria: English language, human population, adult population (≥18 years), and a comparison between MUGA with at least one of the mentioned reference tests. Afterward, full texts of the remaining articles were read, implementing the exclusion criteria to narrow down the search to the most relevant articles. Exclusion criteria were MUGA and reference test performed more than 30 days apart, unclear or invalid correlation analysis method, and no LVEF measurement reported. The methodological quality of each article was assessed using the National Heart, Lung and Blood Institute’s Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies and all studies of poor quality were excluded [18].
The following parameters were extracted from the included studies: study design (prospective/retrospective), population size, female to male ratio, mean age, main cardiac disease, reference test(s), correlation coefficient(s), Bland-Altman 95% limits of agreement (LOAs), and the number of days between the reference test(s) and MUGA. In case multiple correlation values were reported in a single study (e.g., measurements done at different time points), this was transformed into a mean value if possible — likewise for Bland-Altman values. As a rule of thumb for Pearson correlation coefficient analysis, a value of 0.0–0.3 was considered to reflect negligible, 0.3–0.5 low, 0.5–0.7 moderate, 0.7–0.9 high, and 0.9–1.0 very high correlation. Since the definition of CTRCD indicates a change in more than 10 percentage-point change of LVEF, LOAs over 10% either way of the line were considered to represent an unsuitable imaging modality to use interchangeably with MUGA [19]. Percentages were calculated for the study population characteristics and the correlation coefficients and Bland-Altman values were plotted to compare between the various studies and modalities.
Results
Our search yielded a total of 473 articles, as illustrated in the PRISMA flow chart depicted in Figure 1 [20]. Of the 473 articles, 142 were excluded based on language, full text availability, or population age. Through title and abstract screening, 279 articles were excluded based on incomplete agreement with our predefined inclusion criteria. Of the 52 articles assessed on full text, 30 were excluded based on exclusion criteria or missing inclusion criteria. The remaining 22 articles were included in this study and data was extracted for qualitative analysis.
Table 1 provides an overview of the characteristics of the included publications. In total, the studies comprised 1017 patients with a mean age of 56 years, and the male sex was predominant. A prospective study design was used in 18 out of 22 studies. Of the included studies, 41% was conducted between 1984 and 2000, 41% between 2000 and 2010, and 18% between 2010 and 2020. In total, 32 comparisons were made, with 2DHC and CMR being the most common reference tests (22% both). However, when pooling all different 2D TTE methods, this made up 53% of the comparisons. Furthermore, three comparisons were made with 3D TTE, four with contrast angiography, and one with TD.
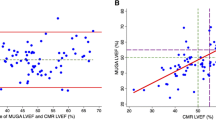
An overview of the correlation coefficients for all comparisons is shown in Figure 2. 2DH shows high correlation overall, with a slight decrease in the latest two studies. 2DHC particularly provides high correlation with MUGA scan throughout the course of time, with five very high and two high correlations. All 3D TTEs showed high correlation values as well. Figure 2 also illustrates varying correlations between MUGA and CMR from 2010 onward. TD was compared once, using cardiac output instead of LVEF, and was reported to correlate very strongly with MUGA results.
Bubble chart depicting correlations between MUGA and other imaging modalities. Most represent the Pearson correlation coefficient, while some studies reported Lin’s concordance (asterisk) or a correlation coefficient from linear regression analysis (dagger). The bubbles represent the correlation between the mentioned tests and MUGA over time, while factoring in the number of participants included (bubble size). 2DF two-dimensional fundamental echocardiography (red), 2DH two-dimensional harmonic echocardiography (orange), 2DHC two-dimensional harmonic echocardiography with contrast (brown), 3D three-dimensional echocardiography (blue), A angiography (yellow), CMR cardiac magnetic resonance imaging (green), and TD thermodilution (purple)
Unfortunately, not all publications reported Bland-Altman LOAs. Of 22 included publications, 16 reported 23 comparisons using Bland-Altman. Figure 3 illustrates that only eight publications had LOAs within the predefined ±10% range; this was predominantly seen for 2DHC (three out of four) and for 3D TTE (two out of three). Almost all 2DF (four out of five) and all the 2DH and angiography comparisons had weak agreements. Interestingly, CMR showed poor agreement with MUGA, with broad LOAs that exceeded the ±10% range in four out of six studies. In particular, the three most recent studies showed weak agreement, with LOAs of −19.4 to 16.5% for Huang et al., −12.1 to 11.4% for Kotha et al., and −15.4 to 9.5% for Dhir et al. [21, 22, 24]. Two older studies by Walker et al. and Gaudio et al. indicated appropriate LOAs of −4.8 to 3.8% and −4 to 7.5%, respectively [25, 26]. However, their cumulative number of subjects (n = 82) accounted for only 23% of the total.
Overview of Bland-Altman 95% limits of agreement. Mean bias is depicted as a black horizontal stripe, the 95% LOA by the colored bars, and the predefined clinical acceptable limit of 10% left ventricular ejection fraction (LVEF) differences by the horizontal lines at ±10% LVEF. 2DF two-dimensional fundamental echocardiography (red), 2DH two-dimensional harmonic echocardiography (orange), 2DHC two-dimensional harmonic echocardiography with contrast (brown), 3D three-dimensional echocardiography (blue), A angiography (yellow), and CMR cardiac magnetic resonance imaging (green)
Discussion
Standardized diagnostic protocols for serial monitoring of LVEF are of crucial importance in cardio-oncological care [2, 7, 9]. As many different non-invasive cardiac diagnostic modalities have evolved, determining their interchangeability is essential. MUGA provides limited cardiac information and contributes to cumulative radiation exposure. Therefore, it has become clear that MUGA should be replaced as the primary method of LVEF monitoring, despite its excellent reproducibility. Therefore, we set out to compare the concordance of LVEF measurements between MUGA and other diagnostic tests to determine which imaging modality should be chosen when local institution guidelines are to be changed from MUGA to an alternative. Additionally, the findings of our systematic analysis will aid in determining the position of MUGA in an imaging strategy when suitable alternatives must be available for echocardiography (e.g., due to poor image quality) and CMR (e.g., due to claustrophobia). Our first main finding was that only 3D TTE and 2DHC correlate well with MUGA and show variability within our pre-defined LOA range of ±10% LVEF units. To our surprise, our second finding revealed that CMR and MUGA do not appear to be interchangeable since most studies (four out of six) reported LOAs exceeding ±10%. Thus, this variability could potentially result in an incorrect diagnosis of CTRCD when these two techniques are used within a single patient.
3D TTE was unfortunately not compared with MUGA as frequently as 2DHC and CMR. Even though no definitive conclusions can be drawn from only three articles (n = 134), the strong correlations and narrow LOAs reported by Walker et al. and Nosir et al. demonstrate that 3D TTE LVEF measurements are highly comparable to MUGA [25, 27]. Both publications had two independent interpreters that blindly evaluated LVEF at separate occasions to minimize observer bias. The third 3D TTE study by Takuma et al. had a weak agreement (despite a correlation of 0.87) that may be explained by their use of an outdated post processing technique [28]. These findings are in line with the recommendation of the EACVI to use 3D TTE as the primary method for serial LVEF monitoring [7, 25, 29].
CMR had correlation coefficients ranging from low to very high and variable LOAs as seen in Figures 2 and 3. In contrast to our expectations, our findings reveal a generally poor agreement between MUGA and CMR. Namely, out of six comparisons with correlation coefficients and Bland-Altman LOAs, four (72% of patients) show poor concordance between MUGA and CMR, strongly suggesting the two are not to be used interchangeably. Interestingly, when comparing CMR and 3D TTE, Walker et al. observed a strong correlation (0.93) and appropriate LOAs of −6.5 to 3% [30]. This may implicate that the recommendation to use CMR as a complementary method only holds true when the primary evaluation was performed with 3D TTE and not MUGA [7, 10]. We lack a good explanation why, in this study, CMR and 3D TTE have an excellent agreement, while a discrepancy exists between the good agreement of MUGA and 3D TTE and the poor agreement between MUGA and CMR.
Figures 2 and 3 illustrate comparable 2DF and 2DH results whereas the superiority of 2DHC is obvious. Our data show that, with seven studies showing very high correlation and three out of four studies with appropriate agreement with MUGA results, 2DHC is the most feasible MUGA replacement when 3D TTE is unavailable [8, 12, 31, 32]. While the two most recent correlation coefficients suggest a slight decline in correlation, the population size of these studies is quite small (33% of patients) which might have affected the results. Normally, contrast administration is advised when images are not sufficiently clear, as it enhances the LV borders. The accuracy and strong correlation with MUGA support this recommendation and should thus be considered in selected cases [10, 33, 34].
Notably, some of the included studies investigated LVEF measurements across different imaging modalities in patients with (possible) cardiotoxicity. As serial monitoring is essential to detect early cardiac dysfunction, these studies compared methods with MUGA over several time points. For example, Walker et al. conducted a long-term research with serial assessments on patients receiving anthracyclines or trastuzumab for breast cancer [25]. They performed real-time 3D TTE, CMR, and MUGA tests at baseline, 6, and 12 months after initiation of trastuzumab and found that 3D TTE was a feasible, accurate, and reproducible alternative for serial monitoring of LVEF. Dhir et al. as well came to the resolution that CMR and MUGA were not interchangeable and serial monitoring should be done with one of the two methods exclusively [24].
Only a limited number of articles were available comparing methods performed on patients undergoing cancer treatment. Instead, most of the publications involved patients with other existing or suspected cardiac problems. Furthermore, technological improvements during the studied period do not allow for any definite conclusions based on the older comparative studies. For example, no study compared 3D TTE with MUGA after 2010, while many technological improvements have occurred that could presumably significantly improve the compatibility between the two methods. Finally, it should be taken into consideration that only two studies included over 100 patients and 46% of the studies had less than 40 patients.
Clinical perspectives
Our findings should be interpreted as clinical recommendations regarding imaging modalities which can be used interchangeably with MUGA to ensure adequate identification of cardiotoxic severity and minimize interpatient variability. Our proposed diagnostic imaging strategy for serial LVEF monitoring in cancer patients at risk for CTRCD, with respect to MUGA, is illustrated in Figure 4. At baseline, 3D TTE should be used as the initial method of LVEF evaluation as it was found to be the most reproducible echocardiographic technique for LVEF measurement over a 1-year follow-up in patients undergoing chemotherapy [11]. Furthermore, it has lower costs and is more widely available than CMR. If unavailable or images of better quality are needed, 2DHC should be performed. In case of unsuitable LVEF calculation by 2DHC, CMR has the preference due to its high correlation with 3D TTE and lack of radiation that MUGA bears [30]. However, MUGA can be used if CMR is unavailable [25]. For patients who have been initially assessed with MUGA, a switch to 3D TTE is advised to avoid cumulative radiation exposure. Alternatively, 2DHC can be used. If the images are unclear, it is more sensible to revert to MUGA, as opposed to CMR, as that would concur most with the initial images taken and thus represent a more accurate monitoring of ejection fraction within a single patient. In patients with unexplained cardiac dysfunction, in those with possible concomitant ischemia, or in those where advanced assessment of tissue characteristics is warranted (e.g., suspicion of myocarditis), the role of CMR is unquestioned and should be considered with a very low threshold to complement the findings of ultrasound in order to better understand the underlying cardiac mechanism in the cancer patient guiding therapeutic decision making [45].
Central illustration: flow diagram of proposed imaging strategy for patients at risk for cancer therapy-related cardiac dysfunction. Preferred modality ranges from top to bottom, from most to least preferred. 2D two-dimensional, 3D three-dimensional, and MUGA multigated acquisition scan. *LVEF obtained by MUGA after CMR monitoring should be interpreted cautiously, since these modalities show poor agreement with one another
Conclusion
In conclusion, when substituting LVEF assessing imaging modalities for MUGA, the findings of this systematic review support the use of echocardiography (3D in particular), while CMR should be used cautiously due to its large variability with MUGA. For serial monitoring of LVEF in patients with (possible) CTRCD, 3D TTE, or alternatively 2DHC, may be the best initial cardiac imaging method.
Data Availability
The data that support the findings of this systematic review are available through the original manuscripts to which we refer. No new data were generated in support of this research.
References
Han X, Zhou Y, Liu W. Precision cardio-oncology: understanding the cardiotoxicity of cancer therapy. npj Precis. Oncol. 2017;1:1–11.
Teske AJ, Linschoten M, Kamphuis JAM, et al. Cardio-oncology: an overview on outpatient management and future developments. Neth Hear J. 2018;26:512–32.
Cardinale D, Colombo A, Bacchiani G, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131:1981–8.
Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355:1572–82.
Naaktgeboren WR, Linschoten M, de Graeff A, et al. Long-term cardiovascular health in adult cancer survivors. Maturitas. 2017;105:37–45.
Clark RA, Marin TS, McCarthy AL, et al. Cardiotoxicity after cancer treatment: a process map of the patient treatment journey. Cardio-Oncology. 2019;5:14.
Plana JC, Galderisi M, Barac A, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2014;27:911–39.
Zamorano JL, Lancellotti P, Rodriguez Munoz D, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines. Eur Heart J. 2016;37:2768–801.
Thakur A, Witteles RM. Cancer therapy-induced left ventricular dysfunction: interventions and prognosis. J Card Fail. 2014;20:155–8.
Makavos G, Ikonomidis I, Palios J, et al. Cardiac imaging in cardiotoxicity: a focus on clinical practice. Heart Fail Rev. 2020;26:1175–87.
Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popović ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol. 2013;61:77–84.
Hare JL, Jenkins C, Nakatani S, Ogawa A, Yu CM, Marwick TH. Feasibility and clinical decision-making with 3D echocardiography in routine practice. Heart. 2008;94:440–5.
Neilan TG, Coelho-Filho OR, Pena-Herrera D, et al. Left ventricular mass in patients with a cardiomyopathy after treatment with anthracyclines. Am J Cardiol. 2012;110:1679–86.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Kosaraju A, Goyal A, Grigorova Y, Makaryus AN. Left ventricular ejection fraction. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459131/. Accessed June 20th, 2020.
Kornbluth M, Liang DH, Brown P, Gessford E, Schnittger I. Contrast echocardiography is superior to tissue harmonics for assessment of left ventricular function in mechanically ventilated patients. Am Heart J. 2000;140:291–6.
Chin BB, Bloomgarden DC, Xia W, et al. Right and left ventricular volume and ejection fraction by tomographic gated blood-pool scintigraphy. J Nucl Med. 1997;28:942–8.
Study Quality Assessment Tools | National Heart, Lung, and Blood Institute (NHLBI) [Internet]. Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed June 15th, 2020.
Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24:68–71.
Moher D, Liberati A, Tetzlaff J AD. PRISMA 2009 flow diagram. The PRISMA statement [Internet]. 2009.
Huang H, Nijjar PS, Misialek JR, et al. Accuracy of left ventricular ejection fraction by contemporary multiple gated acquisition scanning in patients with cancer: comparison with cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2017;19:34.
Kotha VK, Deva DP, Connelly KA, et al. Cardiac MRI and radionuclide ventriculography for measurement of left ventricular ejection fraction in ICD candidates. Magn Reson Imaging. 2018;52:69–74.
Bellenger NG, Marcus NJ, Rajappan K, Yacoub M, Banner NR, Pennell DJ. Comparison of techniques for the measurement of left ventricular function following cardiac transplantation. J Cardiovasc Magn Reson. 2002;4:255–63.
Dhir V, Yan AT, Nisenbaum R, et al. Assessment of left ventricular function by CMR versus MUGA scans in breast cancer patients receiving trastuzumab: a prospective observational study. Int J Card Imaging. 2019;35:2085–93.
Walker J, Bhullar N, Fallah-Rad N, et al. Role of three-dimensional echocardiography in breast cancer: comparison with two-dimensional echocardiography, multiple-gated acquisition scans, and cardiac magnetic resonance imaging. J Clin Oncol. 2010;28:3429–36.
Gaudio C, Tanzilli G, Mazzarotto P, et al. Comparison of left ventricular ejection fraction by magnetic resonance imaging and radionuclide ventriculography in idiopathic dilated cardiomyopathy. Am J Cardiol. 1991;67:411–5.
Nosir YFM, Salustri A, Kasprzak JD, Breburda CS, Ten Cate FJ, Roelandt JRTC. Left ventricular ejection fraction in patients with normal and distorted left ventricular shape by three-dimensional echocardiographic methods: a comparison with radionuclide angiography. J Am Soc Echocardiogr. 1998;11:620–30.
Takuma S, Ota T, Muro T, et al. Assessment of left ventricular function by real-time 3-dimensional echocardiography compared with conventional noninvasive methods. J Am Soc Echocardiogr. 2001;14:275–84.
Driessen MMP, Kort E, Cramer MJM, et al. Assessment of LV ejection fraction using real-time 3D echocardiography in daily practice: direct comparison of the volumetric and speckle tracking methodologies to CMR. Neth Hear J. 2014;22:383–90.
Pickett CA, Cheezum MK, Kassop D, Villines TC, Hulten EA. Accuracy of cardiac CT, radionucleotide and invasive ventriculography, two- and three-dimensional echocardiography, and SPECT for left and right ventricular ejection fraction compared with cardiac MRI: a meta-analysis. Eur Heart J Cardiovasc Imaging. 2015;16:848–52.
Nahar T, Croft L, Shapiro R, et al. Comparison of four echocardiographic techniques for measuring left ventricular ejection fraction. Am J Cardiol. 2000;86:1358–62.
Yu E, Skyba D, Sloggett C, et al. Determination of left ventricular ejection fraction using intravenous contrast and a semiautomated border detection algorithm. J Am Soc Echocardiogr. 2003;16:22–8.
Yu E, Sloggett C, Iwanochko R, Rakowski H, Siu S. Feasibility and accuracy of left ventricular volumes and ejection fraction determination by fundamental, tissue harmonic, and intravenous contrast imaging in difficult-to-image patients. J Am Soc Echocardiogr. 2000;13:216–24.
Malm S, Frigstad S, Sagberg E, Larsson H, Skjaerpe T. Accurate and reproducible measurement of left ventricular volume and ejection fraction by contrast echocardiography: a comparison with magnetic resonance imaging. J Am Coll Cardiol. 2004;44:1030–5.
Vandenbossche JL, Kramer BL, Massie BM, Lynn Morris D, Karliner JS. Two-dimensional echocardiographic evaluation of the size, function and shape of the left ventricle in chronic aortic regurgitation: comparison with radionuclide angiography. J Am Coll Cardiol. 1984;4:1195–206.
Høilund-Carlsen PF, Marving J, Rasmussen S, Haunsø S, Pedersen JF. Accuracy of absolute left ventricular volumes and cardiac output determined by radionuclide cardiography. Int J Cardiol. 1984;6:505–21.
Verani MS, Gaeta J, LeBlanc AD, et al. Validation of left ventricular volume measurements by radionuclide angiography. J Nucl Med. 1985;26:1394–401.
Corbett JR, Jansen DE, Lewis SE, et al. Tomographic gated blood pool radionuclide ventriculography: analysis of wall motion and left ventricular volumes in patients with coronary artery disease. J Am Coll Cardiol. 1985;6:349–58.
Naik MM, Diamond GA, Pai T, Soffer A, Siegel RJ. Correspondence of left ventricular ejection fraction determinations from two-dimensional echocardiography, radionuclide angiography and contrast cineangiography. J Am Coll Cardiol. 1995;25(4):937–42.
Jensen-Urstad K, Bouvier F, Hojer J, et al. Comparison of different echocardiographic methods with radionuclide imaging for measuring left ventricular ejection fraction during acute myocardial infarction treated by thrombolytic therapy. Am J Cardiol. 1998;81:538–44.
Dias BF, Yu EH, Sloggett CE, Iwanochko RM, Rakowski H, Siu SC. Contrast-enhanced quantitation of left ventricular ejection fraction: what is the best method? J Am Soc Echocardiogr. 2001;14:1183–90.
Mohan HK, Livieratos L, Gallagher S, Bailey DL, Chambers J, Fogelman I. Comparison of myocardial gated single photon emission computerised tomography, planar radionuclide ventriculography and echocardiography in evaluating left ventricular ejection fraction, wall thickening and wall motion. Int J Clin Pract. 2004;58:1120–6.
Galasko GIW, Basu S, Lahiri A, Senior R. Is echocardiography a valid tool to screen for left ventricular systolic dysfunction in chronic survivors of acute myocardial infarction? A comparison with radionuclide ventriculography. Heart. 2004;90:1422–6.
Bezante GP, Rosa GM, Bruni R, et al. Improved assessment of left ventricular volumes and ejection fraction by contrast enhanced harmonic color Doppler echocardiography. Int J Card Imaging. 2005;21:609–16.
Plana JC, Thavendiranathan P, Bucciarelli-Ducci C, et al. Multi-modality imaging in the assessment of cardiovascular toxicity in the cancer patient. JACC Cardiovasc Imaging. 2018;11:1173–86.
Funding
L. W. L. is supported by the Netherlands Heart Foundation, Dekker Senior Clinical Scientist 2019, grant agreement no. 2019T056. F. W. A. is supported by UCL Hospitals NIHR Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
M. I. P., L. I. E. Y., M. J. C., J. A. M. K., M. G. G. H., F. W. A., and A. J. T. declare that they have no competing interests.
L. W. L.: outside the current work: consultancy fees from Abbott, Medtronic, Vifor, and Novartis. Investigator-initiated study in collaboration with Roche and Sopachem.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardio-Oncology
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Printezi, M.I., Yousif, L.I.E., Kamphuis, J.A.M. et al. LVEF by Multigated Acquisition Scan Compared to Other Imaging Modalities in Cardio-Oncology: a Systematic Review. Curr Heart Fail Rep 19, 136–145 (2022). https://doi.org/10.1007/s11897-022-00544-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-022-00544-3