Abstract
Purpose of the Review
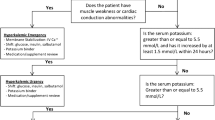
Hyperkalemia is a common electrolyte abnormality that can lead to life-threatening cardiac arrhythmia. Medical management of acute hyperkalemia revolves around three strategies—stabilizing the myocardium, intracellular shifting of serum potassium, and enhancing elimination of total body potassium via urinary or fecal excretion. In this review, we outline the current evidence behind the acute medical management of hyperkalemia.
Recent Findings
Two new oral potassium-binding agents, patiromer and sodium zirconium cyclosilicate, show promise in the management of hyperkalemia. Their role in the acute setting needs further investigation. Recent investigations also suggest that the optimal dosing of intravenous insulin may be lower than previously described.
Summary
Despite its prevalence, there is wide variability in the medical management of hyperkalemia in the acute setting. High-quality evidence demonstrating efficacy is lacking for many medications, though novel oral potassium-binding agents show promise. Overall, more research is necessary to establish optimal dosing strategies to manage hyperkalemia in the acute setting.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Mahoney BA, Smith WAD, Lo D, Tsoi K, Tonelli M, Clase C. Emergency interventions for hyperkalemia. Cochrane Database Syst Rev 2009;1–54.
Singer AJ, Thode HC, Peacock WF. A retrospective study of emergency department potassium disturbances: severity, treatment, and outcomes. Clin Exp Emerg. 2017;4(2):73–9.
Collins AJ, Pitt B, Reaven N, Funk S, McGaughey K, Wilson D, et al. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46:213–21.
Bandak G, Sang YY, Gaspirini A, Chang AR, Ballew SH, Evans M, et al. Hyperkalemia after initiating renin-angiotensin system blockade: the Stockholm creatinine measurements (SCREAM) project. J Am Heart Assoc. 2017;6:1–13.
Chang A, Sang YY, Leddy J, Yahya T, Kirchner HL, Inker LA, et al. Antihypertensive medications and the prevalence of hyperkalemia in a large health system. Hypertension. 2017;67:1181–8.
Betts KA, Woolley JM, Mu F, McDonald E, Tang W, Wu EQ. The prevalence of hyperkalemia in the United States. Curr Med Res Op. 2018;34(6):971–8.
Truhlar A, Deakin C, Soar J, Khalifa GEA, Alfonzo A, Bierenes JJLM, et al. European resuscitation council guidelines for resuscitation 2015. Resuscitation. 2015;95:148–201.
Medford-Davis L, Zubaid R. Derangements of potassium. Emerg Med Clin N Am. 2014;32:329–47.
Pfennig CL, Slovis CM. Electrolyte disorders. Rosen's emergency medicine: concepts and clinical practice: Elsevier; 2018. p. 1516–32.
Khanagavi J, Gupta T, Aronow WS, Shah T, Garg J, Ahn C, et al. Hyperkalemia among hospitalized patients and association between duration of hyperkalemia and outcomes. Arch Med Sci. 2014;10(2):251–7.
An JN, Lee JP, Jeon HJ, Kim DH, Oh YK, et al. Severe hyperkalemia requiring hospitalization: predictors of mortality. Crit Care. 2012;16(6):225.
Einhorn LM, Zhan M, Hsu VD, Walker LD, Moen MF, Seliger SL, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009;169(12):1156–62.
Goyal A, Spertus J, Gosch K, Venkitachalam L, Jones PG, et al. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012;307(2):157–64.
Merril JP, Levin HD, Somerville W, Smith S. Clinical recognition and treatment of acute potassium intoxication. Ann Intern Med. 1950;33:797–830.
Chamberlain MJ. Emergency treatment of hyperkalemia. Lancet Lond Engl. 1964;33:464–7.
Meroney W, Herndon R. The management of acute renal insufficiency. JAMA. 1954;155:877–83.
Vanden Hoek TL, Morrison LJ, Shuster M, Donnino M, Sinz E, Lavonas EJ, et al. 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, part 12. Cardiac arrest in special situations. Circulation. 2010;122:829–61.
Rossignol P, Legrand M, Kosiborod M, Hollenberg SM, Peacock WF, Emmett M, et al. Emergency management of severe hyperkalemia: guideline for best practice and opportunities for the future. Pharmacol Res. 2016;113:585–91.
Alfonso AVM, Isles C, Geddes C, Deighan C. Potassium disorders - clinical spectrum and emergency management. Resuscitation. 2006;70:10–25.
Moss J, Syrengelas A, Antaya R, Lazova R. Calcinosis cutis: a complication of intravenous administration of calcium gluconate. J Cutan Pathol. 2006;33:60–2.
Erickson CP, Olson KR. Case files of the medical toxicology fellowship of California poison control system - San Francisco: calcium plus digoxin - more taboo than toxic? J Med Toxicol. 2008;4(1):33–9.
Manini AF, Nelson LS, Hoffman RS. Prognostic utility of serum potassium in chronic digoxin toxicity. Am J Cardiovasc Drugs. 2016;11(3):173–8.
Nola GT, Pope S, Harrison DC. Assessment of the synergistic relationship between serum calcium and digitalis. Am Heart J. 1970;79:499–507.
Fenton F, Smally AJ, Laut J. Hyperkalemia and digoxin toxicity in a patient with kidney failure. Ann Emerg Med. 1996;28:440–1.
Levine M, Nikkanen H, Pallin D. The effects of intravenous calcium in patients with digoxin toxicity. J Emerg Med. 2011;40(1):21–46.
Ho K. A critically swift response: insulin-stimulated potassium and glucose transport in skeletal muscle. Clin J Am Soc Nephrol. 2011;6:1513–6.
Allon M, Copkney C. Albuterol and insulin for treatment of hyperkalemia in hemodialysis patients. Kidney Int. 1990;38:869–72.
Harel Z, Kamel K. Optimial dose and method of administration of intravenous insulin in the management of emergency hyperkalemia: a systematic review. PLoS One. 2016:1–12;11(5):e0154963.
Brown K, Setji TL, Hale SL, Cooper A, Hong B, Herbst R, et al. Assessing the impact of an order panel utilizing weight-based insulin and standardized monitoring of blood glucose for patients with hyperkalemia. Am J Med Qual. 2018;33(6):598–603.
Wheeler DT, Scafers SJ, Horwedel TA, Deal EN, Tobin GS. Weight-based insulin dosing for acute hyperkalemia results in less hypoglycemia: hyperkalemia treatment and hypoglycemia. J Hosp Med. 2016;11:355–7.
McNicholas BA, Pham MH, Carli K, Chen CH, Colobong-Smith N, Anderson AE, et al. Treatment of hyperkalemia with a low-dose insulin protocol is effective and results in reduced hypoglycemia. Int Soc Nephrol. 2018;3(2):328–36.
Garcia J, Pintens M, Morris A, Takamoto P, Baumgartner L, Tasaka CL. Reduced versus conventional dose insulin for hyperkalemia treatment. J Pharm Pract. 2018;6:089719001879922.
LaRue HA, Peksa GD, Shah SC. A comparison of insulin doses for the treatment of hyperkalemia in patients with renal insufficiency. Pharmcotherapy. 2017;37:1516–22.
Putcha N, Allon M. Management of hyperkalemia in dialysis patients. Semin Dial. 2007;20:431–9.
Ngugi NN, McLigeyo SO, Kayima JK. Treatment of hyperkalemia by altering the transcellular gradient in patients with renal failure: effect of vrious therapeutic approaches. East Afr Med J. 1997;74:503–9.
Montoliu J, Lens S, Revert L. Potassium-lowering effect of albuterol for hyperkalemia in renal failure. Arch Intern Med. 1987;147:713–7.
Blumberg A, Wiedman P, Shaw S, Gnadinger M. Effect of various therapeutic approaches on plasma potassium and major regulating factors in terminal renal failure. Am J Med. 1988;85:507–12.
Liou HH, Chiang SS, Wu SC, Huang TP, Campese VM, Smorgorzewski M, et al. Hypokalemic effects of intravenous infusion or nebulization of salbutamol in patients with chronic renal failure: comparative study. Am J Kidney Dis. 1994;23(2):266–71.
Lens XM, Montoliu J, Cases A, Campistol JM, Revert L. Treatment of hyperkalemia in renal failure: salbutamol v. insulin. Nephrol Dial Transplant. 1989;4:228–32.
Mandelberg A, Krupnik Z, Houri S, Smetana S, Gilad E, Matas Z, et al. Salbutamol mtered-dose inhaler with spacer for hyperkalaemia. How fast? How safe? Chest. 1999;115:617–22.
Pancu D, LaFlamme M, Evans E, Reed J. Levalbuterol is as effective as racemic albuterol in lowering serum potassium. J Emerg Med. 2003;25:13–6.
Schwarz KC, Cohen BD, Lubash GD, Rubin AL. Severe acidosis and hyperpotassemia treated with sodium bicarbonate infusion. Circulation. 1959;19:215–20.
Gutierrez R, Schlessinger F, Oster JR, Rietberg B, Perez GO. Effect of hypertonic versus isotonic sodium bicarbonate on plasma potassium concentration in patients with end-stage renal disease. Miner Electrolyte Metab. 1991;17:297–302.
Allon M, Shanklin N. Effect of bicarbonate administration on plasma potassium in dialysis patients: interactions with insulin and albuterol. Am J Kidney Dis. 1996;28:508–13.
Alfonzo A, Soar J, MacTier R, Fox J, Shillday I, et al. Treatment of acute hyperkalaemia in adults. 2014.
Wang CH, Huang CH, Chang WT, Tsai MS, Yu PH, Wu YW, et al. The effects of calcium and sodium bicarbonate on severe hyperkalemia during cardiopulmonary resuscitation: a retrospective cohort study of adult in-hospital cardiac arrest. Resuscitation. 2016;98:105–11.
Jaber S, Paugam C, Futier E, Lefrant JY, Sigismond L, et al. Sodium bicarbonate therapy for patients with severe metabolic acodisis in the intensive care unit (BICAR-ICU): a multicentre, open-label, randomised controlled, phase 3 trial. Lancet. 2018;392:31–40.
Reyes A. Effects of diuretics on renal excretory function. Eur Heart J. 1992;13:15–21.
Reyes A. Renal excretory profiles of loop diuretics: consequences for therapeutic application. J Cardiovasc Pharmacol. 1993;22:S11–23.
Channer KS, McLean KA, Lawson-Matthew P, Richardson M. Combination diuretic treatment in severe heart failure: a randomised controlled trial. Br Heart J. 1994;71:146–50.
Chawla LS, Davison DL, Brasha-Mitchell E, Koyner JL, Arthur JM, Shaw AD, et al. Development and standardization of a furosemide stress test to predict the severity of acute kidney injury. Crit Care. 2013;17(5):R207.
Carlisle EJ, Donnelly SM, Ethier JH, et al. Modulation of the secretion of potassium accompanying anions in humans. Kidney Int. 1991;39:1206–12.
Kamel KS, Ethier JH, Quaggin S, Levin A, Albert S, Carlisle EJ, et al. Studies to determine the basis for hyperkalemia in recipients of a renal transplant who are treated with cyclosporine. J Am Soc Nephrol. 1992;2:1279–84.
Weisberg L. Management of severe hyperkalemia. Crit Care Med. 2008;36:3246–51.
Kessler C, Ng J, Valdez K, Xie H, Geiger B. The use of sodium polystyrene sulfonate in the inpatient management of hyperkalemia. J Hosp Med. 2011;6:136–40.
McGowan CE, Saha S, Chu G, Resnick MB, Moss SF. Intestinal necrosis due to sodium polystyrene sulfonate (Kayexalate) in sorbitol. South Med J. 2009;102(5):493–7.
Flinn RB, Merrill JP, Welzant WR. Treatment of the oliguric patient with a new sodium-exchange resin and sorbitol. N Engl J Med. 1961;264:111–5.
Scherr L, Ogden DA, Mead AW, Spritz N, Rubin AL. Management of hyperkalemia with a cation-exchange resin. N Engl J Med. 1961;264:115–9.
• Lepage L, Dufour AA, Doiron J, Handfield K, Desforges K, Bell R, et al. Randomized clinical trial of sodium polystyrene sulfonate for the treatment of mild hyperkalemia in CKD. Clin J Am Soc Nephrol. 2015;10:2136–42 One of two randomized control trials demonstrating the efficacy of sodium polystyrene sulfonate in the management of hyperkalemia with a significant reduction in serum potassium by seven days.
• Nasir K, Ahmad A. Treatment of hyperkalemia in patients with chronic kidney disease: a comparison of calcium polystyrene sulphonate and sodium polystyrene sulphonate. J Ayub Med Coll Abbottabad. 2014;26(4):455–8 One of two randomized control trials demonstrating the efficacy of sodium polystyrene sulfonate in the management of hyperkalemia with a significant reduction in serum potassium by three days.
Hunt TV DeMott JM, Ackerbauer KA, Whittier WL, Peksa GD. Single-dose sodium polystyrene sulfonate for hyperkalemia in chronic kidney disease or end-stage renal disease. Clin Kidney J 2018;1–6.
Mistry M, Shea A, Giguere P, Nguyen ML. Evaluation of sodium polystyrene sulfonate dosing strategies in the inpatient management of hyperkalemia. Ann Pharmacother. 2016;50(6):455–62.
Hagan AE, Farrington CA, Wall GC, Belz MM. Sodium polystyrene sulfonate for the treatment of acute hyperkalemia: a retrospective study. Clin Nephrol. 2016;85(1):38–43.
Yu MY, Yeo J, Park JS, Lee CH, Kim GH. Long-term efficacy of oral calcium polystyrene sulfonate for hyperkalemia in CKD patients. PLoS One. 2017;12(3):e0173542.
Nakamura T, Fujisaki T, Miyazono M, Yoshihara M, Jinnouchi H, Fukunari K, et al. Risks and benefits of sodium polystyrene sulfonate for hyperkalemia in patients on maintenance hemodialysis. Drugs RD. 2018;18:231–5.
Gerstman BB, Kirkman R, Platt R. Intestinal necrosis associated with post-operative orally administered sodium polystyrene sulfonate in sorbitol. Am J Kidney Dis. 1992;20(2):159–61.
United States Food and Drug Administration. Kayexalate (sodium polystyrene sulfonate) powder label - FDA. 2010.
Harel Z, Harel S, Shah PS, Wald R, Perl J, Bell CM. Gastrointestinal adverse events with sodium polystyrene sulfonate (Kayexalate) use: a systematic review. Am J Med. 2013;126:264.e9–24.
Li L, Harrison SD, Cope MJ, Park C, Lee L, Salaymeh F, et al. Mechanism of action and pharmacology of patiromer, a nonabsorbed cross-linked polymer that lowers serum potassium concentration in patients with hyperkalemia. J Cardiovasc Pharmacol Ther. 2016;21(5):456–65.
Patiromer. Package insert. Redwood City, CA, USA: Relypsa, LLC; 2015.
• Pitt B, Anker SD, Bushinsky DA, Kitzman DW, Zannad F, Huang IZ. Evaluation of the efficacy and safety of RLY5016, a polymeric potassium binder, in a double-blind, placebo-controlled study in patiehts with chronic heart failure (the PEARL-HF) trial. Eur Heart J. 2011;32:820–8 First randomized control trial demonstrating efficacy and safety of patiromer in the management of chronic hyperkalemia. Demonstrated that 15g oral patiromer twice daily significantly lower mean serum potassium by day 3.
• Bakris GL, Pitt B, Weir MR, Freeman MW, Mayo MR, Garza D, et al. Effect of Patiromer on serum potassium level in patients with hyperkalemia and diabetic kidney disease: the AMETHYST-DN randomized clinical trial. JAMA. 2015;314(2):151–61 Phase II trial demonstrating efficacy and safety of patiromer in the management of chronic hyperkalemia. A major contribution of this study is that AMETHYST-DN was a dose ranging study that established efficacy of multiple doses ranging from 4.2g to 16.8g oral patiromer twice daily led to a dose dependent response in the reduction of serum potassium.
• Weir MR, Bakris GL, Bushinsky DA, Mayo MR, Garza D, Stasiv Y, et al. Patriomer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. NEJM. 2015;372(3):211–21 Phase III trial demonstrating efficacy and safety of patiromer in the management of chronic hyperkalemia. It also demonstrated that cessation of patiromer would to larger increases in serum potassium and higher rates of recurrent hyperkalemia when compared with placebo.
Weir MR, Bushinsky DA, Benton WW, Woods SD, Mayo MR, Arthur SP, et al. Effect of patiromer on hyperkalemia recurrence in older chronic kidney disease patients taking RAAS inhibitors. Am J Med. 2018;131:555–64.
Bushinsky DA, Williams GH, Pitt B, Weir MR, Freeman MW, Garza D, et al. Patiromer induces rapid and sustained potassium lowering in patients with chronic kidney disease and hyperkalemia. Kidney Int. 2015;88:1427–33.
Novel Drug Approvals for 2018. 2018.
Stavros F, Yang A, Leon A, Nuttal M, Rasmussen HS. Characterization of structure and function of ZS-9, a K+ selective ion trap. PLoS One. 2014;9(12):e114686.
• Ash SR, Singh B, Lavin PT, Stavros F, Rasmussen HS. A phase 2 study on the treatment of hyperkalemia in patients with chronic kidney disease suggests that the selective potassium trap, ZS-9, is safe and efficient. Kidney Int. 2015;88:404–11 Phase II trial demonstrating the efficacy and safety of ZS-9 in the management of chronic hyperkalemia in a dose dependent manner. Significant reduction were also seen within one hour, suggesting a role for ZS-9 in the acute management of hyperkalemia.
• Kosiborod M, Rasmussen HS, Lavin P, Qunibi WY, Spinowitz B, Packham D, et al. Effect of sodium zirconium cyclosilicate on potassium lowering for 38 days among outpatients with hyperkalemia. JAMA. 2015;312(21):2223–33 Phase III trial demonstrating the efficacy and safety of ZS-9 in the management of chronic hyperkalemia in a dose dependent manner. This trial also suggests a role for ZS-9 in the acute management of hyperkalemia with a median time of 2.2 hours for the normalization of serum potassium.
Packham DK, Rasmussen HS, Lavin PT, El-Shahawy MA, Roger SD, Block G, et al. Sodium zirconium cyclosilicate in hyperkalemia. NEJM. 2015;372(3):222–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mengyang Liu declares no potential conflicts of interest.
Zubaid Rafique is a principal investigator and consultant for AstraZeneca and Vifor Pharma.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Emergency Medicine
Rights and permissions
About this article
Cite this article
Liu, M., Rafique, Z. Acute Management of Hyperkalemia. Curr Heart Fail Rep 16, 67–74 (2019). https://doi.org/10.1007/s11897-019-00425-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-019-00425-2