Abstract
Purpose of Review
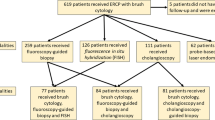
Indeterminate biliary strictures (IDBS) continue to be an area of frustration for clinicians. Standard endoscopic retrograde cholangiopancreatography (ERCP) with conventional brush cytology and/or forceps biopsy has a low sensitivity for distinguishing benign from malignant biliary strictures. A delay in diagnosis of malignancy has consequences for subsequent therapy or surgery. In this article, we review current and emerging technologies that may aid in this diagnostic dilemma.
Recent Findings
Several technologies have been utilized in IDBS to establish a diagnosis which include peroral cholangioscopy, confocal laser endomicroscopy, endoscopic ultrasound with fine needle aspiration, intraductal ultrasound, optical coherence tomography, fluorescence in situ hybridization, next generation sequencing, integrated molecular pathology, and DNA-image cytometry.
Summary
While cholangioscopy and confocal laser endomicroscopy have become standards of care in expert centers for the evaluation of patients with IDBS, there are several endoscopic and molecular modalities that may also aid in establishing a diagnosis. Further head-to-head prospective diagnostic studies as well as cost-efficacy studies are needed.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bowlus CL, Olson KA, Gershwin ME. Evaluation of indeterminate biliary strictures. Nat Rev Gastroenterol Hepatol. 2016;13:28–37.
Singh A, Gelrud A, Agarwal B. Biliary strictures: diagnostic considerations and approach. Gastroenterol Rep (Oxf). 2015;3:22–31.
Oseini AM, Chaiteerakij R, Shire AM, Ghazale A, Kaiya J, Moser CD, et al. Utility of serum immunoglobulin G4 in distinguishing immunoglobulin G4-associated cholangitis from cholangiocarcinoma. Hepatology. 2011;54:940–8.
Azeem N, Ajmera V, Hameed B, Mehta N. Hilar cholangiocarcinoma associated with immunoglobulin G4-positive plasma cells and elevated serum immunoglobulin G4 levels. Hepatol Commun. 2018;2:349–53.
•• Singhi AD, Nikiforova MN, Chennat J, Papachristou GI, Khalid A, Rabinovitz M, et al. Integrating next-generation sequencing to endoscopic retrograde cholangiopancreatography (ERCP)-obtained biliary specimens improves the detection and management of patients with malignant bile duct strictures. Gut. 2020;69:52–61 A large, prospective study demonstrating the impact of combining next generation sequencing and pathological evaluation in diagnosis of malignant bile duct strictures.
Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol. 2007;33:266–70.
Ballehaninna UK, Chamberlain RS. The clinical utility of serum CA 19-9 in the diagnosis, prognosis and management of pancreatic adenocarcinoma: an evidence based appraisal. J Gastrointest Oncol. 2012;3:105–19.
Qin XL, Wang ZR, Shi JS, Lu M, Wang L, He QR. Utility of serum CA19-9 in diagnosis of cholangiocarcinoma: in comparison with CEA. World J Gastroenterol. 2004;10:427–32.
Tabibian JH, Ali AH, Lindor KD. Primary Sclerosing cholangitis, part 1: epidemiology, etiopathogenesis, clinical features, and treatment. Gastroenterol Hepatol. 2018;14:293–304.
Chapman RW, Williamson KD. Are dominant strictures in primary sclerosing cholangitis a risk factor for cholangiocarcinoma? Curr Hepatol Rep. 2017;16:124–9.
Loftus EV, Harewood GC, Loftus CG, Tremaine WJ, Harmsen WS, Zinsmeister AR, et al. PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut. 2005;54:91–6.
Ma MX, Jayasekeran V, Chong AK. Benign biliary strictures: prevalence, impact, and management strategies. Clin Exp Gastroenterol. 2019;12:83–92.
Naseer M, Dailey FE, Al Juboori A, Samiullah S, Tahan V. Epidemiology, determinants, and management of AIDS cholangiopathy: a review. World J Gastroenterol. 2018;24:767–74.
Altman A, Zangan SM. Benign biliary strictures. Semin Intervent Radiol. 2016;33:297–306.
Romagnuolo J, Bardou M, Rahme E, Joseph L. Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Ann Intern Med. 2013;139:547–57.
Rösch T, Meining A, Frühmorgen S, Zillinger C, Schusdziarra V, Hellerhoff K, et al. A prospective comparison of the diagnostic accuracy of ERCP, MRCP, CT, and EUS in biliary strictures. Gastrointest Endosc. 2002;55:870–6.
Al-Dhuhli H. Role of magnetic resonance cholangiopancreatography in the evaluation of biliary disease. Sultan Qaboos Univ Med J. 2009;9:341–52.
Zenouzi R, Welle CL, Venkatesh SK, Schramm C, Eaton JE. Magnetic resonance imaging in primary sclerosing cholangitis--current state and future directions. Semin Liver Dis. 2019;39:369–80.
Navaneethan U, Njei B, Lourdusamy V, Konjeti R, Vargo JJ, Parsi MA. Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and meta-analysis. Gastrointest Endosc. 2015;81:168–76.
• Slivka A, Gan I, Jamidar P, Costamagna G, Cesaro P, Giovannini M, et al. Validation of the diagnostic accuracy of probe-based confocal laser endomicroscopy for the characterization of indeterminate biliary strictures: results of a prospective multicenter international study. Gastrointest Endosc. 2015;81:282–90 A prospective study evaluating the diagnostic performance of confocal laser endomicroscopy in indeterminate biliary strictures and the inflammatory Paris criteria.
Parsa N, Khashab MA. The role of peroral cholangioscopy in evaluating indeterminate biliary strictures. Clin Endosc. 2019;52:556–64.
• de Oliveira PVAG, de Moura DTH, Ribeiro IB, Bazarbashi AN, Franzini TAP, dos Santos MEL, et al. Efficacy of digital single operator cholangioscopy in the visual interpretation of indeterminate biliary strictures: a systematic review and metaanalysis. Surg Endosc. 2020;34:3321–9 A meta-analysis of the use of visual interpretation during peroral cholangioscopy in the diagnosis of indeterminate biliary strictures.
Chen YK, Parsi MA, Binmoeller KF, Hawes RH, Pleskow DK, Slivka A, et al. Single-operator cholangioscopy in patients requiring evaluation of bile duct disease or therapy of biliary stones (with videos). Gastrointest Endosc. 2011;74:805–14.
• Ramchandani M, Reddy DN, Gupta R, Lakhtakia S, Tandan M, Darisetty S, et al. Role of single-operator peroral cholangioscopy in the diagnosis of indeterminate biliary lesions: a single-center, prospective study. Gastrointest Endosc. 2011;74:511–9 A prospective study demonstrating the efficacy of peroral cholangioscopy in the diagnosis of indeterminate biliary lesions.
Manta R, Frazzoni M, Conigliaro R, Maccio L, Melotti G, Dabizzi E, et al. SpyGlass® single-operator peroral cholangioscopy in the evaluation of indeterminate biliary lesions: a single-center, prospective, cohort study. Surg Endosc. 2013;27:1569–72.
Kurihara T, Yasuda I, Isayama H, Tsuyuguchi T, Yamaguchi T, Kawabe K, et al. Diagnostic and therapeutic single-operator cholangiopancreatoscopy in biliopancreatic diseases: prospective multicenter study in Japan. World J Gastroenterol. 2016;22:1891–901.
• Navaneethan U, Hasan MK, Kommaraju K, Zhu X, Hebert-Magee S, Hawes RH, et al. Digital, single-operator cholangiopancreatoscopy in the diagnosis and management of pancreatobiliary disorders: a multicenter clinical experience (with video). Gastrointest Endosc. 2016;84:649–55 A meta-analysis demonstrating the diagnostic utility of peroral cholangioscopy (SpyGlass) and targeted biopsies in the evaluation of indeterminate biliary strictures.
Ogura T, Imanishi M, Kurisu Y, Onda S, Sano T, Takagi W, et al. Prospective evaluation of digital single-operator cholangioscope for diagnostic and therapeutic procedures (with videos). Dig Endosc. 2017;29:782–9.
Shah RJ, Raijman I, Brauer B, Gumustop B, Pleskow DK. Performance of a fully disposable, digital, single-operator cholangiopancreatoscope. Endoscopy. 2017;49:651–8.
Almadi MA, Itoi T, Moon JH, Goenka MK, Seo DW, Rerknimitr R, et al. Using single-operator cholangioscopy for endoscopic evaluation of indeterminate biliary strictures: results from a large multinational registry. Endoscopy. 2020;52:574–82.
•• Gerges C, Beyna T, Tang RSY, Bahin F, Lau JYW, van Geenen E, et al. Digital single-operator peroral cholangioscopy-guided biopsy sampling versus ERCP-guided brushing for indeterminate biliary strictures: a prospective, randomized, multicenter trial (with video). Gastrointest Endosc. 2020;91:1105–13 A multicenter, prospective, randomized study comparing the efficacy of biliary sampling during cholangioscopy to ERCP-brushings.
• Prat F, Leblanc S, Foissac F, Ponchon T, Laugier R, Bichard P, et al. Impact of peroral cholangioscopy on the management of indeterminate biliary conditions: A multicentre prospective trial. Frontline Gastroenterol. 2019;10:236–43 A multicenter, prospective study highlighting the impact of cholangioscopy on the management of indeterminate biliary strictures and primary sclerosing cholangitis.
Korc P, Sherman S. ERCP tissue sampling. Gastrointest Endosc. 2016;84:557–71.
Barakat MT, Angelotti TP, Banerjee S. Use of an ultra-slim gastroscope to accomplish endoscopist-facilitated rescue intubation during ERCP: a novel approach to enhance patient and staff safety. Dig Dis Sci. 2020:1–6.
Di Mitri R, Mocciaro F. Single-operator holmium laser lithotripsy under direct peroral cholangioscopy using an ultra-slim upper endoscope in a patient with a large stone in the common bile duct. Turk J Gastroenterol. 2017;28:505–9.
Weigt J, Kandulski A, Malfertheiner P. Technical improvement using ultra-slim gastroscopes for direct peroral cholangioscopy: analysis of the initial learning phase. J Hepatobiliary Pancreat Sci. 2015;22:74–8.
Pohl J, Meves VC, Mayer G, Behrens A, Frimberger E, Ell C. Prospective randomized comparison of short-access mother-baby cholangioscopy versus direct cholangioscopy with ultraslim gastroscopes. Gastrointest Endosc. 2013;78:609–16.
Lee YN, Moon JH, Lee TH, Choi HJ, Itoi T, Beyna T, et al. Prospective randomized trial of a new multibending versus conventional ultra-slim endoscope for peroral cholangioscopy without device or endoscope assistance (with video). Gastrointest Endosc. 2020;91:92–101.
Mounzer R, Austin GL, Wani S, Brauer BC, Fukami N, Shah RJ. Per-oral video cholangiopancreatoscopy with narrow-band imaging for the evaluation of indeterminate pancreaticobiliary disease. Gastrointest Endosc. 2017;85:509–17.
Itoi T, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Ishii K, et al. Peroral cholangioscopic diagnosis of biliary-tract diseases by using narrow-band imaging (with videos). Gastrointest Endosc. 2007;66:730–6.
Osanai M, Itoi T, Igarashi Y, Tanaka K, Kida M, Maguchi H, et al. Peroral video cholangioscopy to evaluate indeterminate bile duct lesions and preoperative mucosal cancerous extension: a prospective multicenter study. Endoscopy. 2013;45:635–42.
Sethi A, Doukides T, Sejpal DV, Pleskow DK, Slivka A, Adler DG, et al. Interobserver agreement for single operator choledochoscopy imaging: can we do better? Diagn Ther Endosc. 2014;2014:1–4.
Sethi A, Widmer J, Shah NL, Pleskow DK, Edmundowicz SA, Sejpal DV, et al. Interobserver agreement for evaluation of imaging with single operator choledochoscopy: what are we looking at? Dig Liver Dis. 2014;46:518–22.
Ayoub F, Yang D, Draganov PV. Cholangioscopy in the digital era. Transl Gastroenterol Hepatol. 2018;3:1–10.
Kim HJ, Kim MH, Lee SK, Yoo KS, Seo DW, Min Y. Tumor vessel: A valuable cholangioscopic clue of malignant biliary stricture. Gastrointest Endosc. 2000;2:635–8.
Robles-Medranda C, Valero M, Soria-Alcivar M, Puga-Tejada M, Oleas R, Ospina-Arboleda J, et al. Reliability and accuracy of a novel classification system using peroral cholangioscopy for the diagnosis of bile duct lesions. Endoscopy. 2018;50:1059–70.
Sethi A, Tyberg A, Slivka A, Adler DG, Desai AP, Sejpal DV, et al. Digital single-operator cholangioscopy (DSOC) improves interobserver agreement (IOA) and accuracy for evaluation of indeterminate biliary strictures. J Clin Gastroenterol. 2020;0:1–4.
Pavey DA, Gress FG. The role of EUS-guided FNA for the evaluation of biliary strictures. Gastrointest Endosc. 2006;64:334–7.
Fritscher-Ravens A, Broering DC, Knoefel WT, Rogiers X, Swain P, Thonke F, et al. EUS-guided fine-needle aspiration of suspected hilar cholangiocarcinoma in potentially operable patients with negative brush cytology. Am J Gastroenterol. 2004;99:45–51.
Mohamadnejad M, Dewitt JM, Sherman S, Leblanc JK, Pitt HA, House MG, et al. Role of EUS for preoperative evaluation of cholangiocarcinoma: a large single-center experience. Gastrointest Endosc. 2011;73:71–8.
Topazian M. Endoscopic ultrasonography in the evaluation of indeterminate biliary strictures. Clin Endosc. 2012;45:328–30.
• Chiang A, Theriault M, Salim M, James PD. The incremental benefit of EUS for the identification of malignancy in indeterminate extrahepatic biliary strictures: a systematic review and meta-analysis. Endosc Ultrasound. 2019;8:310–7 A meta-analysis demonstrating the diagnostic utility of endoscopic ultrasound in indeterminate biliary strictures.
Sadeghi A, Mohamadnejad M, Islami F, Keshtkar A, Biglari M, Malekzadeh R, et al. Diagnostic yield of EUS-guided FNA for malignant biliary stricture: a systematic review and meta-analysis. Gastrointest Endosc. 2016;83:290–8.
Farrell RJ, Agarwal B, Brandwein SL, Underhill J, Chuttani R, Pleskow DK. Intraductal US is a useful adjunct to ERCP for distinguishing malignant from benign biliary strictures. Gastrointest Endosc. 2002;56:681–7.
Sun B, Hu B. The role of intraductal ultrasonography in pancreatobiliary diseases. Endosc Ultrasound. 2016;5:291–9.
Krishna NB, Saripalli S, Safdar R, Agarwal B. Intraductal US in evaluation of biliary strictures without a mass lesion on CT scan or magnetic resonance imaging: significance of focal wall thickening and extrinsic compression at the stricture site. Gastrointest Endosc. 2007;66:90–6.
Meister T, Heinzow HS, Woestmeyer C, Lenz P, Menzel J, Kucharzik T, et al. Intraductal ultrasound substantiates diagnostics of bile duct strictures of uncertain etiology. World J Gastroenterol. 2013;19:874–81.
• Menzel J, Poremba C, Dietl KH, Domschke W. Preoperative diagnosis of bile duct strictures - comparison of intraductal ultrasonography with conventional endosonography. Scand J Gastroenterol. 2000;35:77–82 One of the few studies to prospectively compare the use of intraductal ultrasound to endoscopic ultrasound in the evaluation of bile duct strictures.
Heinzow HS, Kammerer S, Rammes C, Wessling J, Domagk D, Meister T. Comparative analysis of ERCP, IDUS, EUS and CT in predicting malignant bile duct strictures. World J Gastroenterol. 2014;20:10495–503.
Tamada K, Ueno N, Tomiyama T, Oohashi A, Wada S, Nishizono T, et al. Characterization of biliary strictures using intraductal ultrasonography: comparison with percutaneous cholangioscopic biopsy. Gastrointest Endosc. 1998;47:341–9.
Khandwalla HE, Graham DY, Kramer JR, Ramsey DJ, Duong N, Green LK, et al. Barrett’s esophagus suspected at endoscopy but no specialized intestinal metaplasia on biopsy, what’s next? Am J Gastroenterol. 2014;109:178–82.
Li CQ, Zuo XL, Guo J, Zhang JY, Liu JW, Li YQ. Comparison between two types of confocal laser endomicroscopy in gastrointestinal tract. J Dig Dis. 2015;16:279–85.
Xiong YQ, Ma SJ, Zhou JH, Zhong XS, Chen Q. A meta-analysis of confocal laser endomicroscopy for the detection of neoplasia in patients with Barrett’s esophagus. J Gastroenterol Hepatol. 2016;31:1102–10.
Meining A, Shah RJ, Slivka A, Pleskow D, Chuttani R, Stevens PD, et al. Classification of probe-based confocal laser endomicroscopy findings in pancreaticobiliary strictures. Endoscopy. 2012;44:251–7.
Caillol F, Bories E, Autret A, Poizat F, Pesenti C, Ewald J, et al. Evaluation of pCLE in the bile duct: final results of EMID study: pCLE: impact in the management of bile duct strictures. Surg Endosc. 2015;29:2661–8.
• Meining A, Chen YK, Pleskow D, Stevens P, Shah RJ, Chuttani R, et al. Direct visualization of indeterminate pancreaticobiliary strictures with probe-based confocal laser endomicroscopy: a multicenter experience. Gastroint Endosc. 2011;74:961–8 A prospective, multicenter study demonstrating the diagnostic accuracy of confocal laser endomicroscopy in the diagnosis of indeterminate pancreaticobiliary strictures using the Miami classification.
Taunk P, Singh S, Lichtenstein D, Joshi V, Gold J, Sharma A. Improved classification of indeterminate biliary strictures by probe-based confocal laser endomicroscopy using the Paris Criteria following biliary stenting. J Gastroenterol Hepatol. 2017;32:1778–83.
Dubow M, Tatman PD, Shah RJ. Individual probe based confocal laser endomicroscopy criteria in the analysis of indeterminate biliary strictures. Scand J Gastroenterol. 2018;53:1358–63.
Fugazza A, Gaiani F, Carra MC, Brunetti F, Lévy M, Sobhani I, et al. Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary diseases: a systematic review and meta-analysis. Biomed Res Int. 2016;2016:1–31.
Smith MS, Cash B, Konda V, Trindade AJ, Gordon S, DeMeester S, et al. Volumetric laser endomicroscopy and its application to Barrett’s esophagus: results from a 1,000 patient registry. Dis Esophagus. 2019;32:1–8.
Trindade AJ, McKinley MJ, Fan C, Leggett CL, Kahn A, Pleskow DK. Endoscopic surveillance of Barrett’s esophagus using volumetric laser endomicroscopy with artificial intelligence image enhancement. Gastroenterology. 2019;157:303–5.
Poneros JM, Tearney GJ, Shiskov M, Kelsey PB, Lauwers GY, Nishioka NS, et al. Optical coherence tomography of the biliary tree during ERCP. Gastrointest Endosc. 2002;55:84–8.
Arvanitakis M, Hookey L, Tessier G, Demetter P, Nagy N, Stellke A, et al. Intraductal optical coherence tomography during endoscopic retrograde cholangiopancreatography for investigation of biliary strictures. Endoscopy. 2009;41:696–701.
Tyberg A, Xu MM, Gaidhane M, Kahaleh M. Second generation optical coherence tomography: preliminary experience in pancreatic and biliary strictures. Dig Liver Dis. 2018;50:1214–7.
Nanda A, Brown JM, Berger SH, Lewis MM, Barr Fritcher EG, Gores GJ, et al. Triple modality testing by endoscopic retrograde cholangiopancreatography for the diagnosis of cholangiocarcinoma. Ther Adv Gastroenterol. 2015;8:56–65.
Liew ZH, Loh TJ, Lim TKH, Lim TH, Khor CJL, Mesenas SJ, et al. Role of fluorescence in situ hybridization in diagnosing cholangiocarcinoma in indeterminate biliary strictures. J Gastroenterol Hepatol. 2018;33:315–9.
Gonda TA, Glick MP, Sethi A, Poneros JM, Palmas W, Iqbal S, et al. Polysomy and p16 deletion by fluorescence in situ hybridization in the diagnosis of indeterminate biliary strictures. Gastrointest Endosc. 2012;75:74–9.
Singhi AD, Slivka A. Evaluation of indeterminate biliary strictures: is it time to FISH or cut bait? Gastrointest Endosc. 2016;83:1236–8.
Brooks C, Gausman V, Kokoy-Mondragon C, Munot K, Amin SP, Desai A, et al. Role of fluorescent in situ hybridization, cholangioscopic biopsies, and EUS-FNA in the evaluation of biliary strictures. Dig Dis Sci. 2018;63:636–44.
de Vries AB, van der Heide F, ter Steege RWF, Koornstra JJ, Buddingh KT, Gouw ASH, et al. Limited diagnostic accuracy and clinical impact of single-operator peroral cholangioscopy for indeterminate biliary strictures. Endoscopy. 2020;52:107–14.
Trikudanathan G, Navaneethan U, Njei B, Vargo JJ, Parsi MA. Diagnostic yield of bile duct brushings for cholangiocarcinoma in primary sclerosing cholangitis: a systematic review and meta-analysis. Gastrointest Endosc. 2014;79:783–9.
Arnelo U, von Seth E, Bergquist A. Prospective evaluation of the clinical utility of single-operator peroral cholangioscopy in patients with primary sclerosing cholangitis. Endoscopy. 2015;47:696–702.
Eaton JE, Barr Fritcher EG, Gores GJ, Atkinson EJ, Tabibian JH, Topazian MD, et al. Biliary multifocal chromosomal polysomy and cholangiocarcinoma in primary sclerosing cholangitis. Am J Gastroenterol. 2015;110:299–309.
Quinn KP, Tabibian JH, Lindor KD. Clinical implications of serial versus isolated biliary fluorescence in situ hybridization (FISH) polysomy in primary sclerosing cholangitis. Scand J Gastroenterol. 2017;52:377–81.
Bangarulingam SY, Bjornsson E, Enders F, Barr Fritcher EG, Gores G, Halling KC, et al. Long-term outcomes of positive fluorescence in situ hybridization tests in primary sclerosing cholangitis. Hepatology. 2010;51:174–80.
• Moreno Luna LE, Kipp B, Halling KC, Sebo TJ, Kremers WK, Roberts LR, et al. Advanced cytologic techniques for the detection of malignant pancreatobiliary strictures. Gastroenterology. 2016;131:1064–72 A prospective study comparing the diagnostic utility of cytology, Fluorescence in situ Hybridization and digital image analysis.
Alekseyev YO, Fazeli R, Yang S, Basran R, Maher T, Miller NS, et al. A next-generation sequencing primer—how does it work and what can it do? Acad Pathol. 2018;5:1–11.
• Bankov K, Döring C, Schneider M, Hartmann S, Winkelmann R, Albert JG, et al. Sequencing of intraductal biopsies is feasible and potentially impacts clinical management of patients with indeterminate biliary stricture and cholangiocarcinoma. Clin Transl Gastroenterol. 2018;9:1–10 A study demonstrating the feasibility and potential diagnostic and therapeutic improvements with next generation sequencing in biliary dysplasia and neoplasia.
Malhotra N, Jackson SA, Freed LL, Styn MA, Sidawy MK, Haddad NG, et al. The added value of using mutational profiling in addition to cytology in diagnosing aggressive pancreaticobiliary disease: review of clinical cases at a single center. BMC Gastroenterol. 2014;14:1–7.
Yang X, Sun L, Guo J, Gao L, Qin C, Jin Z. The value of DNA image cytometry combined with brush routine cytology in diagnosing indeterminate biliary strictures: a large sample size retrospective study. J Gastroenterol Hepatol. 2019;34:2036–42.
Agarwal N, Biancardi AM, Patten FW, Reeves AP, Seibel EJ. Three-dimensional DNA image cytometry by optical projection tomographic microscopy for early cancer diagnosis. J Med Imaging. 2014;1:1–10.
Gonzalo-Marin J, Vila JJ, Perez-Miranda M. Role of endoscopic ultrasound in the diagnosis of pancreatic cancer. World J Gastrointest Oncol. 2014;6:360–8.
Heimbach JK, Sanchez W, Rosen CB, Gores GJ. Trans-peritoneal fine needle aspiration biopsy of hilar cholangiocarcinoma is associated with disease dissemination. HPB. 2011;13:356–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Divyesh Sejpal reports grants and personal fees from Boston Scientific, personal fees from Olympus, outside the submitted work.
Arvind Trindade reports personal fees from Olympus America, personal fees from Pentax Medical, personal fees from Ninepoint Medical, outside the submitted work.
Nichol Martinez declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Endoscopy and Surgery
Rights and permissions
About this article
Cite this article
Martinez, N.S., Trindade, A.J. & Sejpal, D.V. Determining the Indeterminate Biliary Stricture: Cholangioscopy and Beyond. Curr Gastroenterol Rep 22, 58 (2020). https://doi.org/10.1007/s11894-020-00797-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s11894-020-00797-9