Abstract
Purpose of Review
To evaluate the impact of the implementation of the Rome IV criteria on pediatric gastrointestinal practice.
Recent Findings
In 2016, the Rome IV criteria were published, providing an update of symptom-based criteria to diagnose children with functional gastrointestinal disorders (FGIDs).
Summary
For neonates and toddlers, Wessel’s criteria for diagnosing infant colic were abandoned, and a differentiation was made between toilet-trained and non-toilet-trained children in the diagnosis of functional constipation. For children and adolescents, two new disorders (functional nausea and functional vomiting) are described, and in the diagnosis of functional dyspepsia, pain does not have to be the chief complaint anymore. This change has made functional dyspepsia the most common functional abdominal pain disorder, exceeding the prevalence of irritable bowel syndrome (IBS). Lastly, the diagnosis of abdominal migraine was narrowed, causing an appropriate drop in its prevalence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional gastrointestinal disorders (FGIDs) are common in children of all age groups [1•, 2•]. In the absence of biomarkers or specific tests to diagnose FGIDs, their diagnosis is based on symptom-based criteria. The current criteria used to diagnose FGIDs were published in 2016 and are called the Rome IV criteria [3••, 4••]. These criteria replace the previous Rome III criteria [5, 6] and are the second revision of the pediatric FGID criteria who were first described in 1999 as the Rome II pediatric criteria [7]. The consensual definition of criteria is important in order to select homogeneous groups of patients to advance research on and treatment for patients with functional gastrointestinal complaints. The diagnostic criteria are regularly updated to account for new developments in epidemiology, pathophysiology, diagnostic testing, and treatment [8]. The current pediatric criteria divide FGIDs according to age groups (neonates and toddlers—0 to 3 years old—and children and adolescents—4 to 18 years old) (see Table 1). Within the children and adolescents’ group of diagnoses, there are three diagnostic categories based on the most bothersome symptom according to the patient’s own report (or parental report in younger children): disorders of nausea and vomiting, disorders of abdominal pain, and defecation disorders [3••, 4••].
This review provides an overview of the most relevant changes in the Rome IV criteria in each age group, the impact of these changes in the epidemiology of FGIDs, and the clinical implications for daily practice. At the end of each section, the reader will find a brief outline on considerations for future research.
Infants and Toddlers
Infant Colic
The most important modification in the diagnosis of FGIDs in neonates and toddlers concerns the diagnostic criteria for infant colic. The Rome IV pediatric committee established different diagnostic criteria for clinical and research purposes. For clinical purposes, the criteria are no longer based on Wessel et al.’s “rule of threes” (crying more than 3 h a day, for more than 3 days a week, for more than 3 weeks in a row) [9]. According to the committee, these criteria were arbitrary, culturally dependent, impractical, and did not reflect the impact of the child’s symptoms on the family [3••]. Therefore, the new clinical criteria are based on symptoms that have been shown to cause higher distress to parents. Besides this, the age of diagnosis of infant colic was extended to infants up to 5 months of age. Infant colic is characterized as recurrent and prolonged periods of crying, fussing, or irritability, without obvious cause and not resolvable or preventable by caregivers, without evidence of failure to thrive, fever, or illness in an infant under 5 months at the onset and resolution of symptoms. With these new criteria, the committee attempted to reduce family distress by providing early and timely reassurance, education, and support to the parents of infants with colic, factors that are the mainstay of management [10]. Changes in the diagnostic criteria for infant colic did not result in significant changes in epidemiology when comparing community-based studies using the Rome III and Rome IV criteria [1•]. The treatment of infant colic is currently based on expert-opinions and should, in the absence of red-flags, focus on reassuring and supporting parents [11].
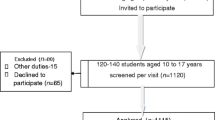
For research purposes, there are additional criteria to diagnose infant colic: the caregiver should report that the infant has cried or fussed for 3 or more hours per day during 3 or more days in 7 days in a telephone or face-to-face screening interview with a researcher or clinician. Crying or fussing should be confirmed to be 3 h or more when measured by at least one prospectively kept, 24-h behavior diary. These additional criteria will secure a specific diagnosis for research; however, they also increase the necessary effort to set up a research study. No studies have been conducted to establish if the changes of the research criteria for infant colic will influence the frequency of diagnosis.
Future research in infant colic should focus on investigating the role of the microbiome in the pathophysiology and possible treatment of infant colic, on developing an objective method to measure the severity of infant colic for research purposes, and on establishing evidence-based management strategies for treating infant colic.
Functional constipation
can be diagnosed in both age groups. There are different definitions for functional constipation in neonates and toddlers versus children and adolescents. The committee harmonized the duration criterion in both age groups to 1 month and made additional adjustments to the criteria for the younger children. After reviewing the Rome III diagnostic criteria, the members of the committee thought that some aspects of the criteria were not pertinent to children in diapers. The Rome IV now differentiates between children with and without toilet training. Non-toilet-trained children may be diagnosed with functional constipation if they show at least two of the following criteria: two or fewer defecations per week, a history of excessive stool retention, a history of painful or hard bowel movements, a history of large-diameter stools, and/or the presence of a large fecal mass in the rectum. For toilet-trained children, two additional criteria may be used: at least one episode of incontinence per week and/or a history of large-diameter stools that may obstruct the toilet. Since the new criteria, one study found a rise in prevalence of functional constipation in infants and toddlers from 4.7 to 12.1% [1]. Unpublished data by some of the authors of this manuscript did not confirm this rise; however, they did find a significant higher prevalence in toilet-trained young children compared with non-toilet-trained young children.
Future research should focus on assessing the impact of the changes made in the Rome IV criteria compared with previous versions in terms of prevalence of constipation and treatment. Next to this, randomized controlled trials should be set up to evaluate the influence of foods and laxatives in this age group.
Children and Adolescents
There have been multiple modifications in the diagnostic criteria in this age group. Specific changes were also made to each category of FGIDs. In the past, there was a common criterion to all FGIDs: a requirement for “absence of inflammatory, anatomic, metabolic, or neoplastic process that explains the subject’s symptoms.” This criterion has been substituted by “after appropriate medical evaluation, the symptoms cannot be attributed to another medical condition.” The reasoning behind this change was the common perception among the members of the committee that the previous statement could be misconstrued as a mandate to conduct exhaustive testing prior to establishing diagnosis. However, in the absence of biomarkers, testing is not always necessary. The rephrasing of the criterion leaves the decision of determining what type of testing (if any) is to be conducted with the physician. Although the result of this change has not yet been evaluated, it was hoped that this would reduce the amount of unnecessary testing in subjects with FGIDs [12].
The Rome IV criteria underscored the importance of recognizing the presence of overlapping comorbidities. Children with FGIDs frequently meet criteria for two FGIDs simultaneously or in succession. The committee also encourages clinicians to consider the possibility of an overlap between FGIDs and organic diseases. For example, it is known that a large proportion of children (up to 25% in some studies) diagnosed with inflammatory bowel disease have symptoms of functional origin that are not explained by the underlying inflammatory process [13]. The recognition of the overlap of functional symptoms in organic diseases moves away from the reductionistic assumption that all symptoms reported by patients with organic diseases should have an organic origin. The understanding that alterations of brain-gut axis can explain the symptoms in children with functional or organic diseases has important treatment implications. It justifies the use of mind-body treatments such as cognitive behavioral therapy, guided imagery, or hypnotherapy to alleviate symptoms [14] in children with both functional and/or organic diagnoses.
Functional Disorders of Nausea and Vomiting
The criteria for the diagnosis of cyclic vomiting syndrome have been modified and are now in line with the NASPGHAN guidelines for diagnoses and treatment [15]. Cyclic vomiting syndrome, abdominal migraine, and migraine headaches are considered part of the same family of disorders and, as such, frequently manifest in the same patient. In order to clarify the diagnosis in patients with overlapping symptoms (e.g., children with cyclic vomiting syndrome and abdominal migraine can have both abdominal pain and vomiting), the Rome IV criteria stress that the primary diagnosis should be based on the most bothersome symptom. This consideration has diagnostic and therapeutic implications in clinical practice, as children with abdominal migraine are not always referred to a pediatric gastroenterologist and are instead seen by neurologists, who use different diagnostic criteria (ICHD) and frequently recommend different treatments [16, 17].
The Rome III criteria made no reference to children with isolated nausea or to the overlap of nausea with non-cyclical disorders. In the previous version of the criteria, nausea was only mentioned in the setting of cyclic vomiting syndrome or abdominal migraine. Studies have shown that nausea is a common symptom in children with functional abdominal pain disorders [18] and that some children have nausea or vomiting that presents in a non-stereotypical and cyclical fashion [19]. Moreover, studies have shown that nausea is a highly invalidating symptom and that children with severe and prolonged nausea have a poor quality of life [20]. As a result, the Rome IV criteria established two new diagnoses: functional nausea and functional vomiting. Functional nausea is applied to the group of children that report bothersome nausea as the predominant symptom, occurring at least twice per week, for at least 2 months, and generally not related to meals, nor consistently associated with vomiting. To diagnose a patient with functional vomiting, the child must have at least one episode of vomiting per week. The vomiting should not be related to an eating disorder, to rumination, or be self-induced. The current evidence suggests that functional nausea and vomiting can be diagnosed in children. Epidemiological studies conducted in the USA and Latin-America have shown that these disorders are uncommon. The prevalence of functional nausea is approximately 0.1–0.5%, and the prevalence of functional vomiting is approximately 0.6–1.4% [1•, 2•].
The newly defined diagnoses allow labeling a subset of patients seen in clinic. Providing a patient with a diagnosis helps reassure the families and children while at the same time may avoid unnecessary testing in search of an elusive disease. Education of families on the diagnosis can provide a sense of relief that can positively influence the prognosis [21]. Due to the recent inclusion of the diagnoses of functional and nausea and vomiting in children, there is still lack of evidence for specific pharmacological and non-pharmacological treatments [22]. In the absence of evidence-based recommendations for their treatment, management principles are extrapolated from clinical trials aimed at treating other diseases/disorders with common symptoms. Pharmacological treatments, as well as complementary treatments such as some herbal therapies, cognitive behavioral therapy, and hypnotherapy, which have been shown to be effective in children with severe nausea due to chemotherapy or post-surgery [23], can be indicated in children with these diagnoses. Similar to the treatment of most FGIDs, an interdisciplinary approach addressing psychosocial burden is sought [19].
Future research on functional nausea and vomiting should focus on establishing the natural history of these disorders, understanding the risk and protective factors for their development, and designing clinical trials to obtain evidence-based data for their treatment. However, due to the low prevalence of these disorders, clinical trials will likely need to be multicenter.
Functional Abdominal Pain Disorders
The group of disorders characterized by the predominance of abdominal pain has been renamed as functional abdominal pain disorders. It was thought that the Rome III criteria term of “abdominal pain predominant functional gastrointestinal disorders” was cumbersome and that new and more intuitive terminology was needed. This group of disorders includes functional abdominal pain-not otherwise specified (FAP-NOS), which replaces the Rome III diagnoses of functional abdominal pain and functional abdominal pain syndrome, two diagnosis that were thought to be a spectrum of severity within the same disorder. Three other diagnoses are included in this category: functional dyspepsia, irritable bowel syndrome (IBS), and abdominal migraine. Each of these diagnoses underwent changes.
Functional Dyspepsia
In contrast to the Rome III criteria, the Rome IV definition of functional dyspepsia does not require patients to describe pain as the predominant symptom. Patients may present with at least one of the following symptoms: postprandial fullness, early satiation, epigastric pain, or burning. With this new definition came two subtypes: epigastric pain syndrome and postprandial distress syndrome. Epigastric pain syndrome is characterized by epigastric pain that is not modified with bowel movements, as would be the case in IBS. Postprandial distress syndrome includes children who have early satiety or discomfort that may not allow them to finish their meal and occasionally even leads to weight loss. While the latter is associated with meals, it is not always the case with epigastric pain syndrome. Based on the new definitions of subtypes, children diagnosed with functional dyspepsia in Rome III would now mostly fulfill the criteria for epigastric pain syndrome in Rome IV. Studies comparing the prevalence of functional abdominal pain disorders between the Rome III criteria and the Rome IV criteria found that with the new definition, functional dyspepsia is now the most common disorder in this group (3.0–7.6%), with postprandial distress syndrome being the most common subtype (2.7–7.2%) [1•, 2•]. Interestingly, in these studies, the prevalence of functional dyspepsia exceeds the prevalence of IBS, which was previously found to be the most prevalent functional abdominal pain disorder in the regions of the conducted studies and in a worldwide meta-analysis [24]. A recent study studying the prevalence of functional dyspepsia in adults in the USA, Canada, and the UK also found functional dyspepsia to be more common than IBS [25]. Because of the previous predominance in prevalence of IBS, most published research was focused on this diagnosis, and little attention was being paid to functional dyspepsia, which was thought to be uncommon. Thus, currently, there are neither guidelines for the treatment of children with functional dyspepsia nor prospective randomized studies to provide recommendations. A recent systematic review found that there is no available evidence to support the use of any pharmacological drugs to treat children with functional dyspepsia [22]. However, the committee made recommendations for the treatment of each subtype based on expert opinion and adult based data. For the epigastric pain syndrome subtype, the committee recommended the use of proton pump inhibitors as first line treatment. Tricyclic antidepressants are recommended for the most severe or recalcitrant cases. For the postprandial distress syndrome subtype, the committee recommends the use of fundal relaxant medications (i.e., cyproheptadine) and prokinetics, such as erythromycin. Retrospective studies have shown that cyproheptadine may be beneficial and safe for children with symptoms of dyspepsia [26]. Although approximately one third of children will report side effects, those are usually minor and limited to somnolence, increased appetite, and weight gain [27]. Other medications with 5HT-1 agonist effect, such as buspirone, have been used with some success in small trials in adults [28]. There are few prokinetics with pediatric evidence available in the USA. The Food and Drug Adminsitration (FDA) has issued a black box warning to the use of metoclopramide due to the risk of tardive dyskinesia associated with prolonged use [29]. Domperidone is not available in the USA, but can be more easily obtained in many other countries. Risk of QT prolongation should be considered with its use [30] as well as with antibiotics that have a motilin agonist effect, such as erythromycin and azithromycin, which are sometimes used as prokinetics. Newly FDA approved prokinetics for the use in adult patients include tegaserod and prucalopride. Pediatric studies have also shown that gastro-electrical stimulation may be useful in children with functional dyspepsia [31, 32].
Prospective, preferably multicenter, studies should be designed to assess the pathophysiology of each subtype of functional dyspepsia in children, to establish the risk factors for their development and prognosis, and to assess the efficacy of the various treatment options.
Abdominal Migraine
With the change of diagnostic criteria from the Rome II to Rome III edition, the prevalence of this diagnosis greatly increased to what was thought to be an unusual high prevalence [33]. The committee considered that such a high prevalence did not reflect clinical practice. Studies have shown that the Rome III abdominal migraine diagnosis was easily misclassified and regularly overlapped with the diagnosis of IBS [33,34,35,36]. The committee made changes in the abdominal migraine diagnosis to solve this problem. The new diagnosis of abdominal migraine is more stringent and better defines the period between symptomatic attacks. The Rome IV criteria include paroxysmal and stereotypical episodes of intense, acute periumbilical, midline or diffuse abdominal incapacitating pain as the predominant symptom, lasting at least 1 h and interfering with daily activities. The pain should be associated with at least 2 of the following: anorexia, nausea, vomiting, headache, photophobia, or pallor, and the episodes should occur at least twice within 6 months [4••]. As a result of these changes in diagnostic criteria, the prevalence of abdominal migraines decreased from 23 to 0.5–1.1% [1•, 2•]. This prevalence most likely better reflects the “real” prevalence of this disorder. This more specific diagnosis of patients with abdominal migraine has important implications for treatment, as management strategies between abdominal migraine and IBS differ. Primary interventions for abdominal migraine include preventive measures such as avoidance of triggers, behavior therapy, and dietary modifications [37]. Pharmacological treatment should be considered if symptoms are refractory to these interventions [37]. Up until now, only one small (n = 16) double blind placebo controlled study has evaluated the effect of pizotifen (not available in the USA) as a prophylactic treatment, which showed a positive effect [38]. Amitriptyline can be used in the prevention of abdominal migraine and cyclic vomiting. The recommended doses for abdominal migraine range 0.2–0.4 mg/kg [39], while for cyclic vomiting syndrome, the guideline recommends slowly increasing the dose up to 1.0–1.5 mg/kg [15].
The committee believes that abdominal migraine, cyclic vomiting, and migraine headache share the same pathophysiology, but none of the current hypotheses have been definitely confirmed [37]. There is a need for studies to better characterize this family of disorders, the common triggers, natural history, and treatment options.
Irritable Bowel Syndrome
In line with adult diagnostic criteria, four subtypes of IBS have been defined [40]. The new classification allows differentiation of treatments for patients with different subtypes of IBS. The subtypes are based on the predominant stooling pattern according to the Bristol Stool Scale and are defined as IBS with constipation (IBS-C), diarrhea (IBS-D), mixed bowel habits (IBS-M), and an unclassified group for those who do not fit in these subtypes. IBS-C seems to be the most common subtype in children and adolescents in most studies; however, it is not uncommon for patients to change subtype over time [41, 42]. An important consideration made by the committee was to set criteria to differentiate IBS-C from functional constipation. The committee recommends that patients with abdominal pain and constipation should first be treated for constipation. When symptoms of abdominal pain persist despite adequate treatment of constipation, the patient is to be diagnosed with IBS-C and treated according to evidence-based guidelines [21].
For the treatment of IBS, education, establishing a therapeutic alliance and providing reassurance, may be sufficient. In other cases, additional therapeutic strategies can be applied. There is increasing evidence for a non-pharmacological treatment approach, including biopsychosocial modifying therapies and dietary interventions [21, 43]. In patients who prefer a pharmacological approach, the Rome IV Interactive Clinical Decision Toolkit recommends antispasmodics as first line and the use of tricyclic antidepressants in recalcitrant cases [44]. The treatment of the patient’s stool problems may require additional medications. Laxatives can be used in cases of constipation and medications that decrease motility and secretions can be used in cases of diarrhea. Common medications used in IBS-D are loperamide and cholestyramine. Studies in adults have shown significant benefit from the use of lubiprostone, prucalopride, and linaclotide over placebo in IBS-C [45]. For adults with IBS-D, the use of bile acid sequestrants may be beneficial, as up to 50% of adults with functional diarrhea and IBS-D have bile acid malabsorption [46]. Rifaximin, eluxadoline, and alosetron have been shown to be beneficial in the treatment of IBS-D in adults but no trials have been conducted in children [47].
There is a paucity of validation of the Bristol Scale and little evidence to support treatments for the various IBS subtypes in children. Large clinical trials should be conducted in this regard and to better characterize the IBS diagnosis and its subtypes and to test the Rome IV proposed differences between IBS-C and functional constipation.
Functional Defecation Disorders
In the category of functional defecation disorders, only minor adjustments were made to the children and adolescent group. The necessary duration for diagnosis of functional constipation was shortened from 2 to 1 month to emphasize the importance of early treatment that was shown to improve the prognosis. Studies comparing the Rome III and Rome IV criteria have shown that the reduction in the time criterion did not modify the prevalence of functional constipation in children and adolescents [1•, 2•, 48].
Conclusion
The Rome IV criteria have changed the framework in which physicians examine, diagnose, and treat children. With the introduction of functional nausea and functional vomiting as defined disorders and the significant changes in diagnostic criteria for infant colic, abdominal migraine, and functional dyspepsia, prevalence and patient characteristics have changed, warranting new studies involving the different patient populations. Additionally, and in view of the differences in results between clinical trials conducted in children and adults, pediatric trials should be designed to establish evidence-based beneficial treatment strategies specifically for children.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Robin SG, Keller C, Zwiener R, Hyman PE, Nurko S, Saps M, et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV criteria. J Pediatr. 2018;195:134–9 Study on the prevalence of functional gastrointestinal disorders in infants and toddlers, and children and adolescents.
• Saps M, Velasco-Benitez CA, Langshaw AH, Ramírez-Hernández CR. Prevalence of functional gastrointestinal disorders in children and adolescents: comparison between Rome III and Rome IV criteria. J Pediatr. 2018;199:212–6 Study on the prevalence of functional gastrointestinal disorders in children and adolescents.
•• Benninga MA, Nurko S, Faure C, Hyman PE, Roberts ISJ, Schechter NL. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. 2016;150(6):1443–55. e2 The Rome IV criteria for neonates/toddlers.
•• Hyams JS, Di Lorenzo C, Saps M, Shulman RJ, Staiano A, van Tilburg M. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2016;150(6):1456–68. e2 The Rome IV criteria for children/adolescents.
Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E, Hyams JS, Staiano A, et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2006;130(5):1527–37.
Hyman PE, Milla PJ, Benninga MA, Davidson GP, Fleisher DF, Taminiau J. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology. 2006;130(5):1519–26.
Rasquin-Weber A, Hyman PE, Cucchiara S, Fleisher DR, Hyams JS, Milla PJ, et al. Childhood functional gastrointestinal disorders. Gut. 1999;45 Suppl 2:Ii60–8. https://doi.org/10.1136/gut.45.2008.ii60.
Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130(5):1377–90.
Wessel MA, Cobb JC, Jackson EB, Harris GS, Detwiler AC. Paroxysmal fussing in infancy, sometimes called “colic”. Pediatrics. 1954;14(5):421–35.
Vandenplas Y, Benninga M, Broekaert I, Falconer J, Gottrand F, Guarino A, et al. Functional gastro-intestinal disorder algorithms focus on early recognition, parental reassurance and nutritional strategies. Acta Paediatr. 2016;105(3):244–52. https://doi.org/10.1111/apa.13270.
Zeevenhooven J, Browne PD, L’Hoir MP, de Weerth C, Benninga MA. Infant colic: mechanisms and management. Nat Rev Gastroenterol Hepatol. 2018;15(8):479–96. https://doi.org/10.1038/s41575-018-0008-7.
Choung RS, Rubio-Tapia A, Lahr BD, Kyle RA, Camilleri MJ, Locke GR, et al. Evidence against routine testing of patients with functional gastrointestinal disorders for celiac disease: a population-based study. Clin Gastroenterol Hepatol. 2015;13(11):1937–43. https://doi.org/10.1016/j.cgh.2015.05.014.
Watson KL Jr, Kim SC, Boyle BM, Saps M. Prevalence and impact of functional abdominal pain disorders in children with inflammatory bowel diseases (IBD-FAPD). J Pediatr Gastroenterol Nutr. 2017;65(2):212–7. https://doi.org/10.1097/mpg.0000000000001479.
Rutten JM, Reitsma JB, Vlieger AM, Benninga MA. Gut-directed hypnotherapy for functional abdominal pain or irritable bowel syndrome in children: a systematic review. Arch Dis Child. 2013;98(4):252–7. https://doi.org/10.1136/archdischild-2012-302906.
Li BU, Lefevre F, Chelimsky GG, Boles RG, Nelson SP, Lewis DW, et al. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition consensus statement on the diagnosis and management of cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr. 2008;47(3):379–93. https://doi.org/10.1097/MPG.0b013e318173ed39.
The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. doi:https://doi.org/10.1177/0333102413485658.
Spiri D, Rinaldi VE, Titomanlio L. Pediatric migraine and episodic syndromes that may be associated with migraine. Ital J Pediatr. 2014;40:92. https://doi.org/10.1186/s13052-014-0092-4.
Kovacic K, Williams S, Li BUK, Chelimsky G, Miranda A. High prevalence of nausea in children with pain-associated functional gastrointestinal disorders: are Rome criteria applicable? J Pediatr Gastroenterol Nutr. 2013;57(3):311–5. https://doi.org/10.1097/MPG.0b013e3182964203.
Kovacic K, Di Lorenzo C. Functional nausea in children. J Pediatr Gastroenterol Nutr. 2016;62(3):365–71. https://doi.org/10.1097/mpg.0000000000001076.
Russell AC, Stone AL, Walker LS. Nausea in children with functional abdominal pain predicts poor health outcomes in young adulthood. Clin Gastroenterol Hepatol. 2017;15(5):706–11. https://doi.org/10.1016/j.cgh.2016.07.006.
Sandhu BK, Paul SP. Irritable bowel syndrome in children: pathogenesis, diagnosis and evidence-based treatment. World J Gastroenterol. 2014;20(20):6013–23. https://doi.org/10.3748/wjg.v20.i20.6013.
Browne PD, Nagelkerke SCJ, van Etten-Jamaludin FS, Benninga MA, Tabbers MM. Pharmacological treatments for functional nausea and functional dyspepsia in children: a systematic review. Expert Rev Clin Pharmacol. 2018;11(12):1195–208. https://doi.org/10.1080/17512433.2018.1540298.
RICHARDSON J, SMITH JE, MCCALL G, RICHARDSON A, PILKINGTON K, KIRSCH I. Hypnosis for nausea and vomiting in cancer chemotherapy: a systematic review of the research evidence. Eur J Cancer Care. 2007;16(5):402–12. https://doi.org/10.1111/j.1365-2354.2006.00736.x.
Korterink JJ, Diederen K, Benninga MA, Tabbers MM. Epidemiology of pediatric functional abdominal pain disorders: a meta-analysis. PLoS One. 2015;10(5):e0126982–e. https://doi.org/10.1371/journal.pone.0126982.
Aziz I, Palsson OS, Törnblom H, Sperber AD, Whitehead WE, Simrén M. Epidemiology, clinical characteristics, and associations for symptom-based Rome IV functional dyspepsia in adults in the USA, Canada, and the UK: a cross-sectional population-based study. Lancet Gastroenterol Hepatol. 2018;3(4):252–62. https://doi.org/10.1016/S2468-1253(18)30003-7.
Rodriguez L, Diaz J, Nurko S. Safety and efficacy of cyproheptadine for treating dyspeptic symptoms in children. J Pediatr. 2013;163(1):261–7. https://doi.org/10.1016/j.jpeds.2012.12.096.
Madani S, Cortes O, Thomas R. Cyproheptadine use in children with functional gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2016;62(3):409–13. https://doi.org/10.1097/mpg.0000000000000964.
Tack J, Janssen P, Masaoka T, Farré R, Van Oudenhove L. Efficacy of buspirone, a fundus-relaxing drug, in patients with functional dyspepsia. Clin Gastroenterol Hepatol. 2012;10(11):1239–45. https://doi.org/10.1016/j.cgh.2012.06.036.
US Food and Drug Administration. FDA requires boxed warning and risk mitigation strategy for metoclopramide-containing drugs: agency warns against chronic use of these products to treat gastrointestinal disorders. Silver Spring, MD: FDA. 2009. https://wayback.archive-it.org/7993/20170112033201/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2009/ucm149533.htm.
Morris AD, Chen J, Lau E, Poh J. Domperidone-associated QT interval prolongation in non-oncologic pediatric patients: a review of the literature. Canadian J Hosp Pharm. 2016;69(3):224–30. https://doi.org/10.4212/cjhp.v69i3.1560.
Lu PL, Teich S, Lorenzo CD, Skaggs B, Alhajj M, Mousa HM. Improvement of quality of life and symptoms after gastric electrical stimulation in children with functional dyspepsia. Neurogastroenterol Motil. 2013;25(7):567–e456. https://doi.org/10.1111/nmo.12104.
Teich S, Mousa HM, Punati J, Di Lorenzo C. Efficacy of permanent gastric electrical stimulation for the treatment of gastroparesis and functional dyspepsia in children and adolescents. J Pediatr Surg. 2013;48(1):178–83. https://doi.org/10.1016/j.jpedsurg.2012.10.038.
Baber KF, Anderson J, Puzanovova M, Walker LS. Rome II versus Rome III classification of functional gastrointestinal disorders in pediatric chronic abdominal pain. J Pediatr Gastroenterol Nutr. 2008;47(3):299–302.
van Tilburg MAL, Squires M, Blois-Martin N, Leiby A, Langseder A. Test of the child/adolescent Rome III criteria: agreement with physician diagnosis and daily symptoms. Neurogastroenterol Motil. 2013;25(4):302–e246. https://doi.org/10.1111/nmo.12056.
Helgeland H, Flagstad G, Grøtta J, Vandvik PO, Kristensen H, Markestad T. Diagnosing pediatric functional abdominal pain in children (4–15 years old) according to the Rome III criteria: results from a Norwegian prospective study. J Pediatr Gastroenterol Nutr. 2009;49(3):309–15.
Saps M, Sztainberg M, Pusatcioglu C, Chogle A. Tu2007 Accuracy of diagnosis for abdominal migraine in children. Gastroenterology. 2014;146(5):S–897.
Mani J, Madani S. Pediatric abdominal migraine: current perspectives on a lesser known entity. Pediatric Health Med Ther. 2018;9:47–58. https://doi.org/10.2147/PHMT.S127210.
Symon DN, Russell G. Double blind placebo controlled trial of pizotifen syrup in the treatment of abdominal migraine. Arch Dis Child. 1995;72(1):48–50. https://doi.org/10.1136/adc.72.1.48.
Bahar RJ, Collins BS, Steinmetz B, Ament ME. Double-blind placebo-controlled trial of amitriptyline for the treatment of irritable bowel syndrome in adolescents. J Pediatr. 2008;152(5):685–9. https://doi.org/10.1016/j.jpeds.2007.10.012.
Drossman DA, Hasler WL. Rome IV—functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257–61.
Giannetti E, de’Angelis G, Turco R, Campanozzi A, Pensabene L, Salvatore S, et al. Subtypes of irritable bowel syndrome in children: prevalence at diagnosis and at follow-up. J Pediatr. 2014;164(5):1099–103.e1. https://doi.org/10.1016/j.jpeds.2013.12.043.
Self MM, Czyzewski DI, Chumpitazi BP, Weidler EM, Shulman RJ. Subtypes of irritable bowel syndrome in children and adolescents. Clin Gastroenterol Hepatol. 2014;12(9):1468–73. https://doi.org/10.1016/j.cgh.2014.01.031.
Newlove-Delgado TV, Martin AE, Abbott RA, Bethel A, Thompson-Coon J, Whear R, et al. Dietary interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev. 2017;3(3):CD010972-CD. https://doi.org/10.1002/14651858.CD010972.pub2.
IV R. Interactive Clinical Decision Toolkit. 2016 http://theromefoundation.org/rome-iv-interactive-clinical-decision-toolkit/. Accessed 12/5/2019.
Chey WD, Lembo AJ, Lavins BJ, Shiff SJ, Kurtz CB, Currie MG, et al. Linaclotide for irritable bowel syndrome with constipation: a 26-week, randomized, double-blind, placebo-controlled trial to evaluate efficacy and safety. Am J Gastroenterol. 2012;107(11):1702–12. https://doi.org/10.1038/ajg.2012.254.
Wedlake L, A’Hern R, Russell D, Thomas K, Walters JR, Andreyev HJ. Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2009;30(7):707–17. https://doi.org/10.1111/j.1365-2036.2009.04081.x.
Brenner DM, Sayuk GS. Current US Food and Drug Administration-approved pharmacologic therapies for the treatment of irritable bowel syndrome with diarrhea. Adv Ther. 2019;37:83–96. https://doi.org/10.1007/s12325-019-01116-z.
Jativa-Marino E, Rivera-Valenzuela MG, Velasco-Benitez CA, Saps M. The prevalence of functional constipation in children was unchanged after the Rome IV criteria halved the diagnosis period in Rome III. Acta Paediatr. 2019. https://doi.org/10.1111/apa.14880.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Miguel Saps has served as a Scientific Consultant for Allergan, Ironwood, and Forest. Marc A. Benninga has served as a Scientific Consultant for Allergan, Norgine, Coloplast, Danone, FrieslandCampina, Sensus, and Takeda. These companies have had no input or involvement in any aspect of this study. The other authors have no conflicts of interest to disclose.
Human and Animal Rights
All reported studies/experiments with human or animal subjects performed by the authors have been previously published, unless stated otherwise, and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Pediatric Gastroenterology
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Baaleman, D.F., Di Lorenzo, C., Benninga, M.A. et al. The Effects of the Rome IV Criteria on Pediatric Gastrointestinal Practice. Curr Gastroenterol Rep 22, 21 (2020). https://doi.org/10.1007/s11894-020-00760-8
Published:
DOI: https://doi.org/10.1007/s11894-020-00760-8