Abstract
Purpose of Review
Colorectal cancer (CRC) screening is recommended to reduce CRC mortality. This review outlines key factors to consider when recommending screening, including disease burden, screening benefits and harms, and remaining knowledge gaps.
Recent Findings
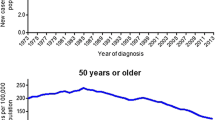
In response to increasing rates of CRC incidence among younger (age < 50 years) adults, the American Cancer Society published guidelines in May 2018 recommending average-risk CRC screening beginning at age 45 (vs. 50) years. Rates of young-onset CRC have increased in the USA since the early 1990s. However, there is very little empirical evidence of screening effectiveness in younger adults, and few studies have reported harms of routine screening in this age group. Further, we know little about the natural history of CRC in younger adults.
Summary
Uncertainty surrounding the efficacy of CRC screening in younger adults suggests the benefits may be small. Precision cancer screening—or modified screening regimens based on risk—may improve the balance of screening benefits and harms beyond conventional age-based strategies.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Winawer SJ, Miller DG, Schottenfeld D, Leidner SD, Sherlock P, Befler B, et al. Feasibility of fecal occult-blood testing for detection of colorectal neoplasia: debits and credits. Cancer. 1977;40(5 Suppl):2616–9.
National Cancer Institute. Working guidelines for early cancer detection: rationale and supporting evidence to decrease mortality. Bethesda, MD: National Cancer Institute Bethesda; 1987.
Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: a decision analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2008;149(9):659–69.
•• Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O'Connor E, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(23):2576–94. https://doi.org/10.1001/jama.2016.3332 Systematic review commissioned by the U.S. Preventive Services Task Force to update CRC screening recommendations in 2016; addresses effectiveness of screening, test performance, and adverse effects of different screening tests.
Murphy CC, Sandler RS, Sanoff HK, Yang YC, Lund JL, Baron JA. Decrease in incidence of colorectal cancer among individuals 50 years or older after recommendations for population-based screening. Clin Gastroenterol Hepatol. 2017;15(6):903–9.e6. https://doi.org/10.1016/j.cgh.2016.08.037.
Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31(1):52–61. https://doi.org/10.1016/j.amepre.2006.03.012.
Maciosek MV, Solberg LI, Coffield AB, Edwards NM, Goodman MJ. Colorectal cancer screening: health impact and cost effectiveness. Am J Prev Med. 2006;31(1):80–9. https://doi.org/10.1016/j.amepre.2006.03.009.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER 9 Regs Research Data, Nov 2017 Sub (1973–2015) <Katrina/Rita Population Adjustment> − Linked To County Attributes - Total U.S., 1969–2016 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2018, based on the November 2017 submission.
• Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, García FA, et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(23):2564–75 Summary of 2016 U.S. Preventive Services Task Force recommendation for colorectal cancer screening.
Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, et al. Colorectal cancer screening: recommendations for physicians and patients from the US Multi-Society Task Force on colorectal cancer. Am J Gastroenterol. 2017;112(7):1016–30.
Leddin D, Lieberman DA, Tse F, Barkun AN, Abou-Setta AM, Marshall JK, et al. Clinical practice guideline on screening for colorectal cancer in individuals with a family history of nonhereditary colorectal cancer or adenoma: The Canadian Association of Gastroenterology Banff Consensus. Gastroenterology. 2018;155(5):1325–47.e3. https://doi.org/10.1053/j.gastro.2018.08.017.
Provenzale D, Gupta S, Ahnen DJ, Markowitz AJ, Chung DC, Mayer RJ, et al. NCCN guidelines insights: colorectal cancer screening, version 1.2018. J Natl Compr Cancer Netw. 2018;16(8):939–49.
Gupta S, Provenzale D, Regenbogen SE, Hampel H, Slavin TP Jr, Hall MJ, et al. NCCN guidelines insights: genetic/familial high-risk assessment: colorectal, version 3.2017. J Natl Compr Cancer Netw. 2017;15(12):1465–75. https://doi.org/10.6004/jnccn.2017.0176.
Qaseem A, Denberg TD, Hopkins RH, Humphrey LL, Levine J, Sweet DE, et al. Screening for colorectal cancer: a guidance statement from the American College of Physicians. Ann Intern Med. 2012;156(5):378–86.
Canaditaion Task Force on Preventive Health. Recommendations on screening for colorectal cancer in primary care. CMAJ. 2016;188(5):340–8.
•• Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte SJ, et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin 2018;68(4):250–81. Summary of new guidelines by the American Cancer Society recommending average risk colorectal cancer screening begin at age 45 years.
Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348(9040):1472–7. https://doi.org/10.1016/s0140-6736(96)03386-7.
Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348(9040):1467–71. https://doi.org/10.1016/s0140-6736(96)03430-7.
Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375(9726):1624–33. https://doi.org/10.1016/s0140-6736(10)60551-x.
Segnan N, Armaroli P, Bonelli L, Risio M, Sciallero S, Zappa M, et al. Once-only sigmoidoscopy in colorectal cancer screening: follow-up findings of the Italian randomized controlled trial--SCORE. J Natl Cancer Inst. 2011;103(17):1310–22. https://doi.org/10.1093/jnci/djr284.
Elmunzer BJ, Hayward RA, Schoenfeld PS, Saini SD, Deshpande A, Waljee AK. Effect of flexible sigmoidoscopy-based screening on incidence and mortality of colorectal cancer: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2012;9(12):e1001352. https://doi.org/10.1371/journal.pmed.1001352.
Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L. Association of colonoscopy and death from colorectal cancer. Ann Intern Med. 2009;150(1):1–8.
Nishihara R, Wu K, Lochhead P, Morikawa T, Liao X, Qian ZR, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369(12):1095–105. https://doi.org/10.1056/NEJMoa1301969.
Young GP, Symonds EL, Allison JE, Cole SR, Fraser CG, Halloran SP, et al. Advances in fecal occult blood tests: the FIT revolution. Dig Dis Sci. 2015;60(3):609–22. https://doi.org/10.1007/s10620-014-3445-3.
Ransohoff DF, Sox HC. Clinical practice guidelines for colorectal cancer screening: new recommendations and new challenges. JAMA. 2016;315(23):2529–31. https://doi.org/10.1001/jama.2016.7990.
Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, et al. Effectiveness of interventions to increase screening for breast, cervical, and colorectal cancers: nine updated systematic reviews for the guide to community preventive services. Am J Prev Med. 2012;43(1):97–118.
•• Siegel RL, Fedewa SA, Anderson WF, Miller KD, Ma J, Rosenberg PS, et al. Colorectal cancer incidence patterns in the United States, 1974-2013. J Natl Cancer Inst. 2017;109(8). https://doi.org/10.1093/jnci/djw322 Landmark publication describing increasing rates of colorectal cancer incidence among younger adults.
Meester RG, Peterse EF, Knudsen AB, de Weerdt AC, Chen JC, Lietz AP, et al. Optimizing colorectal cancer screening by race and sex: microsimulation analysis II to inform the American Cancer Society colorectal cancer screening guideline. Cancer. 2018;124:2974–85.
•• Peterse EFP, Meester RGS, Siegel RL, Chen JC, Dwyer A, Ahnen DJ, et al. The impact of rising colorectal cancer incidence in young adults on the optimal age to start screening: microsimulation analysis I to inform the American Cancer Society colorectal cancer screening guideline. Cancer 2018;124(14):2964–73. Results of microsimulation modeling studies used to inform 2018 American Cancer Society recommendations for colorectal cancer screening in average-risk adults.
• Corley DA, Peek RM. When should guidelines change? a clarion call for evidence regarding the benefits and risks of screening for colorectal cancer at earlier ages. Gastroenterology. 2018;155(4):947–9 Editorial calling for more evidence on the benefits and harms of colorectal cancer screening for 45–49 year olds.
• Liang PS, Allison J, Ladabaum U, Martinez ME, Murphy CC, Schoen RE, et al. Potential intended and unintended consequences of recommending initiation of colorectal cancer screening at age 45 years. Gastroenterology. 2018;155(4):950–4. https://doi.org/10.1053/j.gastro.2018.08.019 Commentary summarizing the pros and cons of lowering the colorectal cancer screening age to 45 years.
• Anderson JC, Samadder JN. To screen or not to screen adults 45–49 years of age: that is the question. Am J Gastroenterol 2018;113(12):1750–3. Summary of two opposing view points in support of or oppostion to American Cancer Society guidelines for colorectal cancer screening.
• Bretthauer M, Kalager M, Weinberg DS. From colorectal cancer screening guidelines to headlines: beware! Ann Intern Med. 2018;169:405–6 Commentary cautioning against adopting new guidelines to lower the screening age to 45 years.
• Imperiale TF, Kahi CJ, Rex DK. Lowering the starting age for colorectal cancer screening to 45 years: who will come...and should they? Clin Gastroenterol Hepatol. 2018;16(10):1541–4. https://doi.org/10.1016/j.cgh.2018.08.023 Commentary addressing key questions to consider when making recommendations for average-risk screening.
Neugut AI, Jacobson JS, Rella VA. Prevalence and incidence of colorectal adenomas and cancer in asymptomatic persons. Gastrointest Endosc Clin N Am. 1997;7(3):387–99.
Imperiale TF, Abhyankar PR, Stump TE, Emmett TW. Prevalence of advanced, precancerous colorectal neoplasms in black and white populations: a systematic review and meta-analysis. Gastroenterology. 2018;155(6):1776–86.e1. https://doi.org/10.1053/j.gastro.2018.08.020.
Levin TR, Corley DA, Jensen CD, Schottinger JE, Quinn VP, Zauber AG, et al. Effects of organized colorectal cancer screening on cancer incidence and mortality in a large community-based population. Gastroenterology. 2018;155(5):1383–91.e5. https://doi.org/10.1053/j.gastro.2018.07.017.
Scholefield JH, Moss SM, Mangham CM, Whynes DK, Hardcastle JD. Nottingham trial of faecal occult blood testing for colorectal cancer: a 20-year follow-up. Gut. 2012;61(7):1036–40. https://doi.org/10.1136/gutjnl-2011-300774.
Arora G, Mannalithara A, Singh G, Gerson LB, Triadafilopoulos G. Risk of perforation from a colonoscopy in adults: a large population-based study. Gastrointest Endosc. 2009;69(3):654–64.
Rabeneck L, Paszat LF, Hilsden RJ, Saskin R, Leddin D, Grunfeld E, et al. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology. 2008;135(6):1899–906, 906.e1. https://doi.org/10.1053/j.gastro.2008.08.058.
Brenner H, Altenhofen L, Stock C, Hoffmeister M. Prevention, early detection, and overdiagnosis of colorectal cancer within 10 years of screening colonoscopy in Germany. Clin Gastroenterol Hepatol. 2015;13(4):717–23.
Rutter CM, Johnson E, Miglioretti DL, Mandelson MT, Inadomi J, Buist DS. Adverse events after screening and follow-up colonoscopy. Cancer Causes Control. 2012;23(2):289–96. https://doi.org/10.1007/s10552-011-9878-5.
Murphy CC, Lund JL, Sandler RS. Young-onset colorectal cancer: earlier diagnoses or increasing disease burden? Gastroenterology. 2017;152(8):1809–12.e3. https://doi.org/10.1053/j.gastro.2017.04.030.
Kaminski MF, Bretthauer M, Zauber AG, Kuipers EJ, Adami H-O, van Ballegooijen M, et al. The NordICC Study: rationale and design of a randomized trial on colonoscopy screening for colorectal cancer. Endoscopy. 2012;44(7):695.
Castells A, Quintero E. Programmatic screening for colorectal cancer: the COLONPREV study. Dig Dis Sci. 2015;60(3):672–80.
Dominitz JA, Robertson DJ, Ahnen DJ, Allison JE, Antonelli M, Boardman KD, et al. Colonoscopy vs. fecal immunochemical test in reducing mortality from colorectal cancer (CONFIRM): rationale for study design. Am J Gastroenterol. 2017;112(11):1736.
Rex DK, Khan AM, Shah P, Newton J, Cummings OW. Screening colonoscopy in asymptomatic average-risk African Americans. Gastrointest Endosc. 2000;51(5):524–7.
Chauvenet M, Cottet V, Lepage C, Jooste V, Faivre J, Bouvier AM. Trends in colorectal cancer incidence: a period and birth-cohort analysis in a well-defined French population. BMC Cancer. 2011;11:282. https://doi.org/10.1186/1471-2407-11-282.
Patel P, De P. Trends in colorectal cancer incidence and related lifestyle risk factors in 15-49-year-olds in Canada, 1969-2010. Cancer Epidemiol. 2016;42:90–100. https://doi.org/10.1016/j.canep.2016.03.009.
Haggar FA, Preen DB, Pereira G, Holman CD, Einarsdottir K. Cancer incidence and mortality trends in Australian adolescents and young adults, 1982-2007. BMC Cancer. 2012;12:151. https://doi.org/10.1186/1471-2407-12-151.
Bailey CE, Hu CY, You YN, Bednarski BK, Rodriguez-Bigas MA, Skibber JM, et al. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surg. 2015;150(1):17–22. https://doi.org/10.1001/jamasurg.2014.1756.
•• Pearlman R, Frankel WL, Swanson B, Zhao W, Yilmaz A, Miller K, et al. Prevalence and spectrum of germline cancer susceptibility gene mutations among patients with early-onset colorectal cancer. JAMA Oncol. 2017;3(4):464–71. https://doi.org/10.1001/jamaoncol.2016.5194 Population-based cohort study in Ohio demonstrating the frequency and wide spectrum of germline muations among young adults diagnosed with colorectal cancer.
•• Stoffel EM, Koeppe E, Everett J, Ulintz P, Kiel M, Osborne J, et al. Germline genetic features of young individuals with colorectal cancer. Gastroenterology. 2018;154(4):897–905.e1. https://doi.org/10.1053/j.gastro.2017.11.004 Large, single center study demonstrating 1 in 5 persons diagnosed with colorectal cancer at age younger than 50 years carries a germline mutation associated with their cancer.
Murphy CC, Singal AG, Baron JA, Sandler RS. Decrease in incidence of young-onset colorectal cancer before recent increase. Gastroenterology. 2018;155:1716–1719.e4. https://doi.org/10.1053/j.gastro.2018.07.045.
Liu PH, Wu K, Ng K, Zauber AG, Nguyen LH, Song M, et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol 2019;5(1):37–44.
Imperiale TF, Kahi CJ, Stuart JS, Qi R, Born LJ, Glowinski EA, et al. Risk factors for advanced sporadic colorectal neoplasia in persons younger than age 50. Cancer Detect Prev. 2008;32(1):33–8. https://doi.org/10.1016/j.cdp.2008.01.003.
Murphy CC, Sanoff HK, Stitzenberg KB, Baron JA, Sandler RS, Yang YC, et al. RE: Colorectal cancer incidence patterns in the United States, 1974–2013. J Natl Cancer Inst. 2017;109(8). https://doi.org/10.1093/jnci/djx104.
Croswell JM, Ransohoff DF, Kramer BS. Principles of cancer screening: lessons from history and study design issues. Semin Oncol. 2010;37(3):202–15. https://doi.org/10.1053/j.seminoncol.2010.05.006.
Wilson JMG, Jungner G. Principles and practice of screening for disease. Geneva: World Health Organization; 1968.
Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319(9):525–32.
Morson B. The polyp-cancer sequence in the large bowel. Thousand Oaks: SAGE Publications; 1974.
Arminski TC, McLean DW. Incidence and distribution of adenomatous polyps of the colon and rectom based on 1,000 autopsy examinations. Dis Colon Rectum. 1964;7:249–61.
Blatt LJ. Polyps of the colon and rectum. Dis Colon Rectum. 1961;4(4):277–82.
Chapman I. Adenomatous polypi of large intestine: incidence and distribution. Ann Surg. 1963;157(2):223–6.
Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Results of screening colonoscopy among persons 40 to 49 years of age. N Engl J Med. 2002;346(23):1781–5. https://doi.org/10.1056/nejm200206063462304.
Lieberman DA, Holub JL, Moravec MD, Eisen GM, Peters D, Morris CD. Prevalence of colon polyps detected by colonoscopy screening in asymptomatic black and white patients. JAMA. 2008;300(12):1417–22. https://doi.org/10.1001/jama.300.12.1417.
• Jung YS, Ryu S, Chang Y, Yun KE, Park JH, Kim HJ, et al. Risk factors for colorectal neoplasia in persons aged 30 to 39 years and 40 to 49 years. Gastrointest Endosc. 2015;81(3):637-45.e7. https://doi.org/10.1016/j.gie.2014.09.031 Large study of asymptomatic patients undergoing routine colorectal cancer screening showing low prevalence of colonic neoplasia in young adults.
Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer control study. N Engl J Med. 1993;328(19):1365–71. https://doi.org/10.1056/nejm199305133281901.
Selby JV, Friedman GD, Quesenberry CP Jr, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326(10):653–7. https://doi.org/10.1056/nejm199203053261001.
Newcomb PA, Norfleet RG, Storer BE, Surawicz TS, Marcus PM. Screening sigmoidoscopy and colorectal cancer mortality. J Natl Cancer Inst. 1992;84(20):1572–5.
Holme Ø, Løberg M, Kalager M, Bretthauer M, Hernán MA, Aas E, et al. Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: a randomized clinical trial. JAMA. 2014;312(6):606–15.
Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012;366(25):2345–57.
U.S. Preventive Services Task Force. Guide to clinical preventive services. Alexandria, VA: International Medical Publishing; 1996.
•• Knudsen AB, Zauber AG, Rutter CM, Naber SK, Doria-Rose VP, Pabiniak C, et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the US Preventive Services Task Force. JAMA. 2016. https://doi.org/10.1001/jama.2016.6828 Results of microsimulation modeling studies used to inform 2016 U.S. Preventive Services Task Force recommendations for colorectal cancer screening in average-risk adults.
Quintero E, Castells A, Bujanda L, Cubiella J, Salas D, Lanas A, et al. Colonoscopy versus fecal immunochemical testing in colorectal-cancer screening. N Engl J Med. 2012;366(8):697–706. https://doi.org/10.1056/NEJMoa1108895.
Levin TR, Zhao W, Conell C, Seeff LC, Manninen DL, Shapiro JA, et al. Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med. 2006;145(12):880–6.
U.S. Preventive Services Task Force. USPSTF and Cost Considerations. 2017. https://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-and-cost-considerations. Accessed December 2018.
•• Marcus PM, Pashayan N, Church TR, Doria-Rose VP, Gould MK, Hubbard RA, et al. Population-based precision cancer screening: a symposium on evidence, epidemiology, and next steps. Cancer Epidemiol Biomarkers Prev. 2016;25(11):1449–55. https://doi.org/10.1158/1055-9965.Epi-16-0555 Review of National Cancer Institue-sponosred symposium on precision cancer screening, including a discussion of available evidence and challenges for implementation.
• Jeon J, Du M, Schoen RE, Hoffmeister M, Newcomb PA, Berndt SI, et al. Determining risk of colorectal cancer and starting age of screening based on lifestyle, environmental, and genetic factors. Gastroenterology. 2018;154(8):2152-64.e19. https://doi.org/10.1053/j.gastro.2018.02.021 Risk calculation models using a combination of lifestyle and environmental factors and genetic variants determin risk of CRC and optimal age to begin screening.
Funding
National Center for Advancing Translational Sciences (KL2TR001103) and National Cancer Institute (P30CA142543) at the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Caitlin Murphy declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on GI Oncology
Rights and permissions
About this article
Cite this article
Murphy, C.C. Colorectal Cancer in the Young: Does Screening Make Sense?. Curr Gastroenterol Rep 21, 28 (2019). https://doi.org/10.1007/s11894-019-0695-4
Published:
DOI: https://doi.org/10.1007/s11894-019-0695-4