Abstract
Purpose of Review
Patients with long-standing ulcerative colitis have an increased risk for the development of colorectal cancer (CRC). Colitis-related dysplasia appears to confer the greatest risk. Colonoscopic surveillance to detect dysplasia has been advocated by gastrointestinal societies. The aim of surveillance is the reduction of mortality and morbidity of CRC through detection and resection of dysplasia or detecting CRC at an earlier and potentially curable stage. Traditional surveillance has relied on mucosal assessment with targeted biopsy of visible lesions and random biopsy sampling on the premise that dysplasia was not visible at endoscopy. Advances in optical technology permitting increased detection of dysplasia and evidence that most dysplasia is visible has had practice-changing implications.
Recent Findings
Emerging evidence favours chromoendoscopy (CE) for dysplasia detection and is gaining wider acceptance through recent international (International Consensus Statement on Surveillance and Management of Dysplasia in Inflammatory Bowel Disease (SCENIC)) recommendations and endorsed by many gastrointestinal societies. Adoption of CE as the gold standard of surveillance has been met with by scepticism, from conflicting data, operational barriers and the need to understand the true impact of increasingly higher dysplasia detection on overall CRC mortality.
Summary
Valid debate notwithstanding, implementation of a risk stratification protocol that includes CE is an effective approach allowing earlier detection of dysplasia and colorectal neoplasia, determination of surveillance intervals with appropriate allocation of resources and limiting morbidity from CRC and colonoscopy itself. Further prospective data should define the true and long-term impact of dysplasia detection with modern techniques.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Beaugerie L, Itzkowitz SH. Cancers complicating inflammatory bowel disease. N Engl J Med. 2015;373(195). https://doi.org/10.1056/NEJMc1505689.
Farraye FA, Odze RD, Eaden J, et al. AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138:746–74. 774 e1–4; quiz e12–3
Itzkowitz SH, Present DH, Crohn's, et al. Consensus conference: colorectal cancer screening and surveillance in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11(3):314–21. https://doi.org/10.1097/01.MIB.0000160811.76729.d5.
•• American Society for Gastrointestinal Endoscopy Standards of Practice C, Shergill AK, Lightdale JR, et al. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015;81:1101–21 e1–13. A comprehensive evidence based update from the ASGE with useful algorithms for managing dysplasia in IBD patients
Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017;11(6):649–70.
Mowat C, Cole A, Windsor A, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011;60:571–607.
Kornbluth A, Sachar DB, Practice Parameters Committee of the American College of G. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105(3):501–23; quiz 524. https://doi.org/10.1038/ajg.2009.727.
Rutter M, Saunders B, Wilkinson K, et al. Severity of inflammation is a risk factor for colorectal neoplasia in ulcerative colitis. Gastroenterology. 2004;126:451–9.
Cairns SR, Scholefield JH, Steele RJ, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010;59(5):666–89. https://doi.org/10.1136/gut.2009.179804.
Colman RJ, Rubin DT. Histological inflammation increases the risk of colorectal neoplasia in ulcerative colitis: a systematic review. Intest Res. 2016;14(3):202–10. https://doi.org/10.5217/ir.2016.14.3.202.
Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013;7:982–1018.
Rutter MD, Riddell RH. Colorectal dysplasia in inflammatory bowel disease: a clinicopathologic perspective. Clin Gastroenterol Hepatol. 2014;12(3):359–67. https://doi.org/10.1016/j.cgh.2013.05.033.
Rutter MD, Saunders BP, Wilkinson KH, Kamm MA, Williams CB, Forbes A. Most dysplasia in ulcerative colitis is visible at colonoscopy. Gastrointest Endosc. 2004;60(3):334–9. https://doi.org/10.1016/S0016-5107(04)01710-9.
Rubin DT, Rothe JA, Hetzel JT, Cohen RD, Hanauer SB. Are dysplasia and colorectal cancer endoscopically visible in patients with ulcerative colitis? Gastrointest Endosc. 2007;65(7):998–1004. https://doi.org/10.1016/j.gie.2006.09.025.
Munkholm P. Review article: the incidence and prevalence of colorectal cancer in inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18(Suppl 2):1–5. https://doi.org/10.1046/j.1365-2036.18.s2.2.x.
Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48(4):526–35. https://doi.org/10.1136/gut.48.4.526.
Choi CH, Rutter MD, Askari A, et al. Forty-year analysis of colonoscopic surveillance program for neoplasia in ulcerative colitis: an updated overview. Am J Gastroenterol. 2015;110(7):1022–34. https://doi.org/10.1038/ajg.2015.65.
Jess T, Simonsen J, Jorgensen KT, et al. Decreasing risk of colorectal cancer in patients with inflammatory bowel disease over 30 years. Gastroenterology. 2012;143:375–81. e1; quiz e13–4
Ekbom A, Helmick C, Zack M, et al. Ulcerative colitis and colorectal cancer. A population-based study. N Engl J Med. 1990;323:1228–33.
Floren CH, Benoni C, Willen R. Histologic and colonoscopic assessment of disease extension in ulcerative colitis. Scand J Gastroenterol. 1987;22(4):459–62. https://doi.org/10.3109/00365528708991491.
Meucci G, Vecchi M, Astegiano M, et al. The natural history of ulcerative proctitis: a multicenter, retrospective study. Gruppo di Studio per le Malattie Infiammatorie Intestinali (GSMII). Am J Gastroenterol. 2000;95:469–73.
Soetikno RM, Lin OS, Heidenreich PA, Young HS, Blackstone MO. Increased risk of colorectal neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis: a meta-analysis. Gastrointest Endosc. 2002;56(1):48–54. https://doi.org/10.1067/mge.2002.125367.
Saxena AP, Limdi JK, Farraye FA. Zeroing in on endoscopic and histologic mucosal healing to reduce the risk of colorectal neoplasia in inflammatory bowel disease. Gastrointest Endosc. 2017;86(6):1012–4. https://doi.org/10.1016/j.gie.2017.08.029.
Rubin DT, Huo D, Kinnucan JA, et al. Inflammation is an independent risk factor for colonic neoplasia in patients with ulcerative colitis: a case-control study. Clin Gastroenterol Hepatol. 2013;11:1601–8 e1–4.
•• Flores BM, O'Connor A, Moss AC. Impact of mucosal inflammation on risk of colorectal neoplasia in patients with ulcerative colitis: a systematic review and meta-analysis. Gastrointest Endosc 2017. A recent meta-analysis assessing the impact of histological inflammation on colorectal cancer risk in IBD raising further debate on whether mucosal healing alone is sufficient to reduce colitis-associated colorectal cancer risk.
•• Laine L, Kaltenbach T, Barkun A, et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015;148:639–651 e28. An international consensus with practice-changing implications to dysplasia surveillance and endorsed by most GI societies.
Rogler G. Chronic ulcerative colitis and colorectal cancer. Cancer Lett. 2014;345(2):235–41. https://doi.org/10.1016/j.canlet.2013.07.032.
Chiba T, Marusawa H, Ushijima T. Inflammation-associated cancer development in digestive organs: mechanisms and roles for genetic and epigenetic modulation. Gastroenterology. 2012;143(3):550–63. https://doi.org/10.1053/j.gastro.2012.07.009.
Hussain SP, Hofseth LJ, Harris CC. Radical causes of cancer. Nat Rev Cancer. 2003;3(4):276–85. https://doi.org/10.1038/nrc1046.
Redston MS, Papadopoulos N, Caldas C, et al. Common occurrence of APC and K-ras gene mutations in the spectrum of colitis-associated neoplasias. Gastroenterology. 1995;108:383–92.
Rubin CE, Haggitt RC, Burmer GC, Brentnall TA, Stevens AC, Levine DS, et al. DNA aneuploidy in colonic biopsies predicts future development of dysplasia in ulcerative colitis. Gastroenterology. 1992;103(5):1611–20. https://doi.org/10.1016/0016-5085(92)91185-7.
Burmer GC, Rabinovitch PS, Haggitt RC, Crispin d, Brentnall TA, Kolli VR, et al. Neoplastic progression in ulcerative colitis: histology, DNA content, and loss of a p53 allele. Gastroenterology. 1992;103(5):1602–10. https://doi.org/10.1016/0016-5085(92)91184-6.
Cartwright CA, Coad CA, Egbert BM. Elevated c-Src tyrosine kinase activity in premalignant epithelia of ulcerative colitis. J Clin Invest. 1994;93(2):509–15. https://doi.org/10.1172/JCI117000.
Kisiel JB, Konijeti GG, Piscitello AJ, Chandra T, Goss TF, Ahlquist d, et al. Stool DNA analysis is cost effective for colorectal cancer surveillance in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14(12):1778–87. https://doi.org/10.1016/j.cgh.2016.07.018.
Kanthan R, Senger JL, Kanthan SC. Fecal molecular markers for colorectal cancer screening. Gastroenterol Res Pract. 2012;2012:184343.
Kaminski MF, Hassan C, Bisschops R, et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2014;46(5):435–49. https://doi.org/10.1055/s-0034-1365348.
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 2003;58:S3–43, 6, DOI: https://doi.org/10.1016/S0016-5107(03)02159-X.
Siegel CA, Schwartz LM, Woloshin S, Cole EB, Rubin DT, Vay T, et al. When should ulcerative colitis patients undergo colectomy for dysplasia? Mismatch between patient preferences and physician recommendations. Inflamm Bowel Dis. 2010;16(10):1658–62. https://doi.org/10.1002/ibd.21233.
Watanabe T, Ajioka Y, Mitsuyama K, et al. Comparison of targeted vs random biopsies for surveillance of ulcerative colitis-associated colorectal cancer. Gastroenterology. 2016;151:1122–30.
Wang YR, Cangemi JR, Loftus EV Jr, Picco MF. Rate of early/missed colorectal cancers after colonoscopy in older patients with or without inflammatory bowel disease in the United States. Am J Gastroenterol. 2013;108(3):444–9. https://doi.org/10.1038/ajg.2012.429.
Kiesslich R, Fritsch J, Holtmann M, et al. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003;124:880–8.
Matsumoto T, Nakamura S, Jo Y, Yao T, Iida M. Chromoscopy might improve diagnostic accuracy in cancer surveillance for ulcerative colitis. Am J Gastroenterol. 2003;98(8):1827–33. https://doi.org/10.1111/j.1572-0241.2003.07580.x.
Hurlstone DP, McAlindon ME, Sanders DS, Keogh R, Lobo AJ, Cross SS. Further validation of high-magnification chromoscopic-colonoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2004;126(1):376–8. https://doi.org/10.1053/j.gastro.2003.05.021.
Subramanian V, Mannath J, Ragunath K, et al. Meta-analysis: the diagnostic yield of chromoendoscopy for detecting dysplasia in patients with colonic inflammatory bowel disease. Aliment Pharmacol Ther. 2011;33:304–12.
Konijeti GG, Shrime MG, Ananthakrishnan AN, Chan AT. Cost-effectiveness analysis of chromoendoscopy for colorectal cancer surveillance in patients with ulcerative colitis. Gastrointest Endosc. 2014;79(3):455–65. https://doi.org/10.1016/j.gie.2013.10.026.
•• Iannone A, Ruospo M, Wong G, et al. Chromoendoscopy for surveillance in ulcerative colitis and Crohn’s disease: a systematic review of randomized trials. Clin Gastroenterol Hepatol 2017;(11):1684-1697. An important meta-analysis summarising the evidence for chromoendoscopy for dysplasia surveillance in IBD.
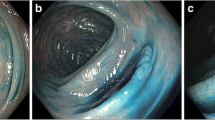
•• Soetikno R, Sanduleanu S, Kaltenbach T. An atlas of the nonpolypoid colorectal neoplasms in inflammatory bowel disease. Gastrointest Endosc Clin N Am. 2014;24(3):483–520. An essential resource for endoscopists for lesion recognition and chromoendoscopy. https://doi.org/10.1016/j.giec.2014.04.003.
Rutter MD, Saunders BP, Schofield G, Forbes A, Price AB, Talbot IC. Pancolonic indigo carmine dye spraying for the detection of dysplasia in ulcerative colitis. Gut. 2004;53(2):256–60. https://doi.org/10.1136/gut.2003.016386.
Soetikno R, Subramanian V, Kaltenbach T, et al. The detection of nonpolypoid (flat and depressed) colorectal neoplasms in patients with inflammatory bowel disease. Gastroenterology. 2013;144:1349–52. 1352 e1–6
Moussata D, Allez M, Cazals-Hatem D, et al. Are random biopsies still useful for the detection of neoplasia in patients with IBD undergoing surveillance colonoscopy with chromoendoscopy? Gut 2017.
Navaneethan U, Jegadeesan R, Gutierrez NG, et al. Progression of low-grade dysplasia to advanced neoplasia based on the location and morphology of dysplasia in ulcerative colitis patients with extensive colitis under colonoscopic surveillance. J Crohns Colitis. 2013;7:e684–91.
van den Broek FJ, Stokkers PC, Reitsma JB, et al. Random biopsies taken during colonoscopic surveillance of patients with longstanding ulcerative colitis: low yield and absence of clinical consequences. Am J Gastroenterol. 2014;109(5):715–22. https://doi.org/10.1038/ajg.2011.93.
Hurlstone DP, Sanders DS, Atkinson R, Hunter MD, McAlindon ME, Lobo AJ, et al. Endoscopic mucosal resection for flat neoplasia in chronic ulcerative colitis: can we change the endoscopic management paradigm? Gut. 2007;56(6):838–46. https://doi.org/10.1136/gut.2006.106294.
Higgins PD. Miles to go on the SCENIC route: should chromoendoscopy become the standard of care in IBD surveillance? Am J Gastroenterol. 2015;110:1035–7.
Kiesslich R, Goetz M, Lammersdorf K, et al. Chromoscopy-guided endomicroscopy increases the diagnostic yield of intraepithelial neoplasia in ulcerative colitis. Gastroenterology. 2007;132:874–82.
Wu L, Li P, Wu J, Cao Y, Gao F. The diagnostic accuracy of chromoendoscopy for dysplasia in ulcerative colitis: meta-analysis of six randomized controlled trials. Color Dis. 2012;14(4):416–20. https://doi.org/10.1111/j.1463-1318.2010.02505.x.
Marion JF, Sands BE. The SCENIC consensus statement on surveillance and management of dysplasia in inflammatory bowel disease: praise and words of caution. Gastroenterology. 2015;148(3):462–7. https://doi.org/10.1053/j.gastro.2015.01.029.
Goldstone R, Itzkowitz S, Harpaz N, et al. Progression of low-grade dysplasia in ulcerative colitis: effect of colonic location. Gastrointest Endosc. 2011;74:1087–93.
Venkatesh PG, Jegadeesan R, Gutierrez NG, et al. Natural history of low grade dysplasia in patients with primary sclerosing cholangitis and ulcerative colitis. J Crohns Colitis. 2013;7:968–73.
Pekow JR, Hetzel JT, Rothe JA, Hanauer SB, Turner JR, Hart J, et al. Outcome after surveillance of low-grade and indefinite dysplasia in patients with ulcerative colitis. Inflamm Bowel Dis. 2010;16(8):1352–6. https://doi.org/10.1002/ibd.21184.
Marion JF, Waye JD, Israel Y, Present DH, Suprun M, Bodian C, et al. Chromoendoscopy is more effective than standard colonoscopy in detecting dysplasia during long-term surveillance of patients with colitis. Clin Gastroenterol Hepatol. 2016;14(5):713–9. https://doi.org/10.1016/j.cgh.2015.11.011.
Gasia MF, Ghosh S, Panaccione R, Ferraz JG, Kaplan GG, Leung Y, et al. Targeted biopsies identify larger proportions of patients with colonic neoplasia undergoing high-definition colonoscopy, dye chromoendoscopy, or electronic virtual chromoendoscopy. Clin Gastroenterol Hepatol. 2016;14(5):704–12 e4. https://doi.org/10.1016/j.cgh.2015.12.047.
Deepak P, Hanson GJ, Fletcher JG, Tremaine WJ, Pardi DS, Kisiel JB, et al. Incremental diagnostic yield of chromoendoscopy and outcomes in inflammatory bowel disease patients with a history of colorectal dysplasia on white-light endoscopy. Gastrointest Endosc. 2016;83(5):1005–12. https://doi.org/10.1016/j.gie.2015.09.021.
Krugliak Cleveland N, Colman RJ, Rodriquez D, Hirsch A, Cohen RD, Hanauer SB, et al. Surveillance of IBD using high definition colonoscopes does not miss adenocarcinoma in patients with low-grade dysplasia. Inflamm Bowel Dis. 2016;22(3):631–7. https://doi.org/10.1097/MIB.0000000000000634.
Mooiweer E, van der Meulen-de Jong AE, Ponsioen CY, et al. Chromoendoscopy for surveillance in inflammatory bowel disease does not increase neoplasia detection compared with conventional colonoscopy with random biopsies: results from a large retrospective study. Am J Gastroenterol. 2015;110(7):1014–21. https://doi.org/10.1038/ajg.2015.63.
Fumery M, Dulai PS, Gupta S, Prokop LJ, Ramamoorthy S, Sandborn WJ, et al. Incidence, risk factors, and outcomes of colorectal cancer in patients with ulcerative colitis with low-grade dysplasia: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2017;15(5):665–74 e5. https://doi.org/10.1016/j.cgh.2016.11.025.
Marion JF, Waye JD, Present DH, Israel Y, Bodian C, Harpaz N, et al. Chromoendoscopy-targeted biopsies are superior to standard colonoscopic surveillance for detecting dysplasia in inflammatory bowel disease patients: a prospective endoscopic trial. Am J Gastroenterol. 2008;103(9):2342–9. https://doi.org/10.1111/j.1572-0241.2008.01934.x.
Kaltenbach T, McQuaid KR, Soetikno R, Laine L. Improving detection of colorectal dysplasia in inflammatory bowel disease surveillance. Gastrointest Endosc. 2016;83(5):1013–4. https://doi.org/10.1016/j.gie.2015.11.003.
Carballal S, Maisterra S, Lopez-Serrano A, et al. Real-life chromoendoscopy for neoplasia detection and characterisation in long-standing IBD. Gut. 2016;
Picco MF, Pasha S, Leighton JA, Bruining D, Loftus EV Jr, Thomas CS, et al. Procedure time and the determination of polypoid abnormalities with experience: implementation of a chromoendoscopy program for surveillance colonoscopy for ulcerative colitis. Inflamm Bowel Dis. 2013;19(9):1913–20. https://doi.org/10.1097/MIB.0b013e3182902aba.
Davies J, Burke D, Olliver JR, et al. Methylene blue but not indigo carmine causes DNA damage to colonocytes in vitro and in vivo at concentrations used in clinical chromoendoscopy. Gut. 2007;56:155–6.
Repici A, Di Stefano AF, Radicioni MM, et al. Methylene blue MMX tablets for chromoendoscopy. Safety tolerability and bioavailability in healthy volunteers. Contemp Clin Trials. 2012;33(2):260–7. https://doi.org/10.1016/j.cct.2011.11.006.
Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson d, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143(3):844–57. https://doi.org/10.1053/j.gastro.2012.06.001.
Engelsgjerd M, Farraye FA, Odze RD. Polypectomy may be adequate treatment for adenoma-like dysplastic lesions in chronic ulcerative colitis. Gastroenterology. 1999;117(6):1288–94; discussion 1488-91. https://doi.org/10.1016/S0016-5085(99)70278-7.
Odze RD, Farraye FA, Hecht JL, Hornick JL. Long-term follow-up after polypectomy treatment for adenoma-like dysplastic lesions in ulcerative colitis. Clin Gastroenterol Hepatol. 2004;2(7):534–41. https://doi.org/10.1016/S1542-3565(04)00237-X.
Rubin PH, Friedman S, Harpaz N, et al. Colonoscopic polypectomy in chronic colitis: conservative management after endoscopic resection of dysplastic polyps. Gastroenterology. 1999;117:1295–300.
Vieth M, Behrens H, Stolte M. Sporadic adenoma in ulcerative colitis: endoscopic resection is an adequate treatment. Gut. 2006;55:1151–5.
Wanders LK, Dekker E, Pullens B, et al. Cancer risk after resection of polypoid dysplasia in patients with longstanding ulcerative colitis: a meta-analysis. Clin Gastroenterol Hepatol. 2014;12:756–64.
Ten Hove JR, Mooiweer E, Dekker E, et al. Low rate of dysplasia detection in mucosa surrounding dysplastic lesions in patients undergoing surveillance for inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2017;15(2):222–8 e2. https://doi.org/10.1016/j.cgh.2016.08.035.
Smith LA, Baraza W, Tiffin N, et al. Endoscopic resection of adenoma-like mass in chronic ulcerative colitis using a combined endoscopic mucosal resection and cap assisted submucosal dissection technique. Inflamm Bowel Dis. 2008;14:1380–6.
Blonski W, Kundu R, Furth EF, et al. High-grade dysplastic adenoma-like mass lesions are not an indication for colectomy in patients with ulcerative colitis. Scand J Gastroenterol. 2008;43:817–20.
Ullman T, Croog V, Harpaz N, et al. Progression of flat low-grade dysplasia to advanced neoplasia in patients with ulcerative colitis. Gastroenterology. 2003;125:1311–9.
Thomas T, Abrams KA, Robinson RJ, et al. Meta-analysis: cancer risk of low-grade dysplasia in chronic ulcerative colitis. Aliment Pharmacol Ther. 2007;25(6):657–68. https://doi.org/10.1111/j.1365-2036.2007.03241.x.
Befrits R, Ljung T, Jaramillo E, et al. Low-grade dysplasia in extensive, long-standing inflammatory bowel disease: a follow-up study. Dis Colon rectum. 2002;45:615–20.
Hata K, Watanabe T, Kazama S, et al. Earlier surveillance colonoscopy programme improves survival in patients with ulcerative colitis associated colorectal cancer: results of a 23-year surveillance programme in the Japanese population. Br J Cancer. 2003;89:1232–6.
Lim CH, Dixon MF, Vail A, Forman D, Lynch d, Axon AT. Ten year follow up of ulcerative colitis patients with and without low grade dysplasia. Gut. 2003;52(8):1127–32. https://doi.org/10.1136/gut.52.8.1127.
Bernstein CN, Blanchard JF, Kliewer E, Wajda A. Cancer risk in patients with inflammatory bowel disease: a population-based study. Cancer. 2001;91(4):854–62. https://doi.org/10.1002/1097-0142(20010215)91:4<854::AID-CNCR1073>3.0.CO;2-Z.
Dekker E, van den Broek FJ, Reitsma JB, et al. Narrow-band imaging compared with conventional colonoscopy for the detection of dysplasia in patients with longstanding ulcerative colitis. Endoscopy. 2007;39(3):216–21. https://doi.org/10.1055/s-2007-966214.
Ignjatovic A, East JE, Subramanian V, Suzuki N, Guenther T, Palmer N, et al. Narrow band imaging for detection of dysplasia in colitis: a randomized controlled trial. Am J Gastroenterol. 2012;107(6):885–90. https://doi.org/10.1038/ajg.2012.67.
van den Broek FJ, Fockens P, van Eeden S, et al. Narrow-band imaging versus high-definition endoscopy for the diagnosis of neoplasia in ulcerative colitis. Endoscopy. 2011;43(02):108–15. https://doi.org/10.1055/s-0030-1255956.
Pellise M, Lopez-Ceron M, Rodriguez de Miguel C, et al. Narrow-band imaging as an alternative to chromoendoscopy for the detection of dysplasia in long-standing inflammatory bowel disease: a prospective, randomized, crossover study. Gastrointest Endosc. 2011;74:840–8.
Leifeld L, Rogler G, Stallmach A, Schmidt C, Zuber-Jerger I, Hartmann F, et al. White-light or narrow-band imaging colonoscopy in surveillance of ulcerative colitis: a prospective multicenter study. Clin Gastroenterol Hepatol. 2015;13(10):1776–81 e1. https://doi.org/10.1016/j.cgh.2015.04.172.
Neumann H, Kiesslich R. Endomicroscopy and endocytoscopy in IBD. Gastrointest Endosc Clin N Am. 2013;23(3):695–705. https://doi.org/10.1016/j.giec.2013.03.006.
Gunther U, Kusch D, Heller F, et al. Surveillance colonoscopy in patients with inflammatory bowel disease: comparison of random biopsy vs. targeted biopsy protocols. Int J Color Dis. 2011;26:667–72.
Hlavaty T, Huorka M, Koller T, et al. Colorectal cancer screening in patients with ulcerative and Crohn’s colitis with use of colonoscopy, chromoendoscopy and confocal endomicroscopy. Eur J Gastroenterol Hepatol. 2011;23:680–9.
Rispo A, Castiglione F, Staibano S, et al. Diagnostic accuracy of confocal laser endomicroscopy in diagnosing dysplasia in patients affected by long-standing ulcerative colitis. World J Gastrointest Endosc. 2012;4:414–20.
Naymagon S, Marion JF. Surveillance in inflammatory bowel disease: chromoendoscopy and digital mucosal enhancement. Gastrointest Endosc Clin N Am. 2013;23:679–94.
Subramanian V, Ragunath K. Advanced endoscopic imaging: a review of commercially available technologies. Clin Gastroenterol Hepatol. 2014;12(3):368–76 e1. https://doi.org/10.1016/j.cgh.2013.06.015.
Committee AT. Confocal laser endomicroscopy. Gastrointest Endosc. 2014;80:928–38.
Committee AT, Kwon RS, Wong Kee Song LM, et al. Endocytoscopy. Gastrointest Endosc. 2009;70(4):610–3. https://doi.org/10.1016/j.gie.2009.06.030.
Kisiel JB, Yab TC, Nazer Hussain FT, Taylor WR, Garrity-Park MM, Sandborn WJ, et al. Stool DNA testing for the detection of colorectal neoplasia in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013;37(5):546–54. https://doi.org/10.1111/apt.12218.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Inflammatory Bowel Disease
Rights and permissions
About this article
Cite this article
Limdi, J.K., Farraye, F.A. An Update on Surveillance in Ulcerative Colitis. Curr Gastroenterol Rep 20, 7 (2018). https://doi.org/10.1007/s11894-018-0612-2
Published:
DOI: https://doi.org/10.1007/s11894-018-0612-2