Abstract
Purpose of Review
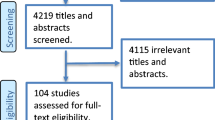
To perform a systematic review and meta-analysis of the prevalence of diabetes in patients with hyperuricemia and gout.
Recent Findings
Previous studies have confirmed that hyperuricemia and gout are associated with an increased risk of diabetes. A previous meta-analysis indicated that the prevalence of diabetes in patients with gout is 16%.
Summary
Thirty-eight studies (458,256 patients) were included in the meta-analysis. The combined prevalence of diabetes among patients with hyperuricemia and gout were 19.10% (95% confidence interval [CI]: 17.60-20.60; I2 = 99.40%) and 16.70% (95% CI: 15.10-18.30; I2 = 99.30%), respectively. Patients from North America showed a higher prevalence of diabetes (hyperuricemia: 20.70% [95% CI: 16.80-24.60], gout: 20.70% [95% CI: 16.80-24.60]) than those from other continents. Older patients with hyperuricemia and those using diuretics showed a higher prevalence of diabetes than younger patients and those who were not using diuretics. Studies with a small sample size, case-control design, and low quality score had a higher prevalence of diabetes than studies with a large sample size, other designs, and a high quality score. The prevalence of diabetes among patients with hyperuricemia and gout is high. Controlling plasma glucose and uric acid levels of patients with hyperuricemia and gout is critical for the prevention of diabetes.





Similar content being viewed by others
Data Availability
The datasets are available from the corresponding author on reasonable request.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183: 109119.
Magliano DJBE. IDF Diabetes Atlas. Brussels: International Diabetes Federation; 2021.
Maiuolo J, Oppedisano F, Gratteri S, Muscoli C, Mollace V. Regulation of uric acid metabolism and excretion. Int J Cardiol. 2016;213:8–14.
Chen-Xu M, Yokose C, Rai SK, Pillinger MH, Choi HK. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007–2016. Arthritis Rheumatol. 2019;71(6):991–9.
Nutmakul T. A review on benefits of quercetin in hyperuricemia and gouty arthritis. Saudi Pharm J. 2022;30(7):918–26.
Kim SC, Liu J, Solomon DH. Risk of incident diabetes in patients with gout: a cohort study. Arthritis Rheumatol. 2015;67(1):273–80.
Wang T, Bi Y, Xu M, Huang Y, Xu Y, Li X, et al. Serum uric acid associates with the incidence of type 2 diabetes in a prospective cohort of middle-aged and elderly Chinese. Endocrine. 2011;40(1):109–16.
Choi HK, De Vera MA, Krishnan E. Gout and the risk of type 2 diabetes among men with a high cardiovascular risk profile. Rheumatology (Oxford). 2008;47(10):1567–70.
Tung YC, Lee SS, Tsai WC, Lin GT, Chang HW, Tu HP. Association Between Gout and Incident Type 2 Diabetes Mellitus: A Retrospective Cohort Study. Am J Med. 2016;129(11):e17–25.
•• Zhao R, Wang Y, Fu T, Zhou W, Ge X, Sha X, et al. Gout and risk of diabetes mellitus: meta-analysis of observational studies. Psychol Health Med. 2020;25(8):917–30. A meta-analysis discussing the prevalence of diabetes among patients with gout.
Chhana A, Lee G, Dalbeth N. Factors influencing the crystallization of monosodium urate: a systematic literature review. BMC Musculoskelet Disord. 2015;16:296.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama 2000; 283(15): 2008–12.
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A. Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol. 2006;6:31.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Stewart S, Rome K, Eason A, House ME, Horne A, Doyle AJ, et al. Predictors of activity limitation in people with gout: a prospective study. Clin Rheumatol. 2018;37(8):2213–9.
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8(1):2–10.
Chen SY, Chen CL, Shen ML. Manifestations of metabolic syndrome associated with male gout in different age strata. Clin Rheumatol. 2007;26(9):1453–7.
Chua CG, Thong BY. Inflammatory Arthritis Among Military Servicemen From a Rheumatology Center in Singapore. Mil Med 2021.
Hsu CY, Lin CL, Kao CH. Gout is associated with organic and psychogenic erectile dysfunction. Eur J Intern Med. 2015;26(9):691–5.
Janssens HJ, Arts PG, Schalk BW, Biermans MC. Gout and rheumatoid arthritis, both to keep in mind in cardiovascular risk management: A primary care retrospective cohort study. Joint Bone Spine. 2017;84(1):59–64.
Joo K, Kwon SR, Lim MJ, Jung KH, Joo H, Park W. Prevention of comorbidity and acute attack of gout by uric acid lowering therapy. J Korean Med Sci. 2014;29(5):657–61.
Primatesta P, Plana E, Rothenbacher D. Gout treatment and comorbidities: a retrospective cohort study in a large US managed care population. BMC Musculoskelet Disord. 2011;12:103.
Chen SY, Chen CL, Shen ML, Kamatani N. Trends in the manifestations of gout in Taiwan. Rheumatology (Oxford). 2003;42(12):1529–33.
Chen Y, Cheng J, Chen Y, Wang N, Xia F, Chen C, et al. Association between serum vitamin D and uric acid in the eastern Chinese population: a population-based cross-sectional study. BMC Endocr Disord. 2020;20(1):79.
Collier A, Stirling A, Cameron L, Hair M, Crosbie D. Gout and diabetes: a common combination. Postgrad Med J. 2016;92(1089):372–8.
Hirsch JD, Terkeltaub R, Khanna D, Singh J, Sarkin A, Shieh M, et al. Gout disease-specific quality of life and the association with gout characteristics. Patient Relat Outcome Meas. 2010;2010:1–8.
Huang CC, Huang PH, Chen JH, Lan JL, Tsay GJ, Lin HY, et al. An Independent Risk of Gout on the Development of Deep Vein Thrombosis and Pulmonary Embolism: A Nationwide, Population-Based Cohort Study. Medicine (Baltimore). 2015;94(51): e2140.
Juraschek SP, Kovell LC, Miller ER 3rd, Gelber AC. Gout, urate-lowering therapy, and uric acid levels among adults in the United States. Arthritis Care Res (Hoboken). 2015;67(4):588–92.
Pang S, Jiang Q, Sun P, Li Y, Zhu Y, Liu J, et al. Hyperuricemia prevalence and its association with metabolic disorders: a multicenter retrospective real-world study in China. Ann Transl Med. 2021;9(20):1550.
Richette P, Clerson P, Périssin L, Flipo RM, Bardin T. Revisiting comorbidities in gout: a cluster analysis. Ann Rheum Dis. 2015;74(1):142–7.
Robinson PC, Merriman TR, Herbison P, Highton J. Hospital admissions associated with gout and their comorbidities in New Zealand and England 1999–2009. Rheumatology (Oxford). 2013;52(1):118–26.
Roddy E, Muller S, Hayward R, Mallen CD. The association of gout with sleep disorders: a cross-sectional study in primary care. BMC Musculoskelet Disord. 2013;14:119.
Schlesinger N, Radvanski DC, Cheng JQ, Kostis JB. Erectile Dysfunction Is Common among Patients with Gout. J Rheumatol. 2015;42(10):1893–7.
Scire CA, Manara M, Cimmino MA, Govoni M, Salaffi F, Punzi L, et al. Gout impacts on function and health-related quality of life beyond associated risk factors and medical conditions: results from the KING observational study of the Italian Society for Rheumatology (SIR). Arthritis Res Ther. 2013;15(5):R101.
Te Kampe R, Janssen M, van Durme C, Jansen TL, Boonen A. Sex Differences in the Clinical Profile Among Patients With Gout: Cross-sectional Analyses of an Observational Study. J Rheumatol. 2021;48(2):286–92.
Tee M, Lustre Ii C, Abrilla A, Afos IE, Cañal JP. Prevalence of Urolithiasis by Ultrasonography Among Patients with Gout: A Cross-Sectional Study from the UP-Philippine General Hospital. Res Rep Urol. 2020;12:423–31.
Yu Q, Shen HC, Hu YC, Chen YF, Tung TH. Prevalence and Metabolic Factors of Hyperuricemia in an Elderly Agricultural and Fishing Population in Taiwan. Arch Rheumatol. 2017;32(2):149–57.
Golmohammadi S, Tavasoli M, Asadi N. Prevalence and Risk Factors of Hyperuricemia in Patients with Chronic Kidney Disease and Non-Alcoholic Fatty Liver. Clin Exp Gastroenterol. 2020;13:299–304.
González-Senac NM, Bailén R, Torres RJ, de Miguel E, Puig JG. Metabolic syndrome in primary gout. Nucleosides Nucleotides Nucleic Acids. 2014;33(4–6):185–91.
Irfan M, Jawaid W, Hashmat O, Nisa Q, Khastoori DR 2nd, Shahbaz NN. Association Between Hyperuricemia and Acute Ischemic Stroke in Patients at a Tertiary Care Hospital. Cureus. 2020;12(10): e10899.
Janssens HJ, van de Lisdonk EH, Bor H, van den Hoogen HJ, Janssen M. Gout, just a nasty event or a cardiovascular signal? A study from primary care. Fam Pract. 2003;20(4):413–6.
Kravchenko D, Bergner R, Behning C, Schäfer VS. How to Differentiate Gout, Calcium Pyrophosphate Deposition Disease, and Osteoarthritis Using Just Four Clinical Parameters. Diagnostics (Basel) 2021; 11(6).
Liao XP, Zhu HW, Zeng F, Tang ZH. The association and interaction analysis of hypertension and uric acid on cardiovascular autonomic neuropathy. J Endocrinol Invest. 2015;38(10):1075–82.
Nagahama K, Inoue T, Kohagura K, Ishihara A, Kinjo K, Ohya Y. Hyperuricemia predicts future metabolic syndrome: a 4-year follow-up study of a large screened cohort in Okinawa. Japan Hypertens Res. 2014;37(3):232–8.
Pillinger MH, Bangalore S, Klein AB, Baumgartner S, Morlock R. Cardiovascular Disease and Gout: Real-World Experience Evaluating Patient Characteristics, Treatment Patterns, and Health Care Utilization. J Manag Care Spec Pharm. 2017;23(6):677–83.
Rodríguez G, Soriano LC, Choi HK. Impact of diabetes against the future risk of developing gout. Ann Rheum Dis. 2010;69(12):2090–4.
Stepanova NLSLL. Hyperuricemia Predicts Residual Diuresis Decline in Peritoneal Dialysis Patients. Electr J Gen Med. 2021;18(1):em270.
Takeuchi F, Yamamoto K, Isono M, Katsuya T, Akiyama K, Ohnaka K, et al. Genetic impact on uric acid concentration and hyperuricemia in the Japanese population. J Atheroscler Thromb. 2013;20(4):351–67.
Tanaka A, Taguchi I, Teragawa H, Ishizaka N, Kanzaki Y, Tomiyama H, et al. Febuxostat does not delay progression of carotid atherosclerosis in patients with asymptomatic hyperuricemia: A randomized, controlled trial. PLoS Med. 2020;17(4): e1003095.
Wu EQ, Patel PA, Mody RR, Yu AP, Cahill KE, Tang J, et al. Frequency, risk, and cost of gout-related episodes among the elderly: does serum uric acid level matter? J Rheumatol. 2009;36(5):1032–40.
Zhang Y, Yang Y, Xue L, Wen J, Bo L, Tang M, et al. Clinical characteristics of patients under 40 years old with early-onset hyperuricaemia: a retrospective monocentric study in China. BMJ Open. 2019;9(8): e025528.
Dehghan A, van Hoek M, Sijbrands EJ, Hofman A, Witteman JC. High serum uric acid as a novel risk factor for type 2 diabetes. Diabetes Care. 2008;31(2):361–2.
Sluijs I, Beulens JW, van der AD, Spijkerman AM, Schulze MB, van der Schouw YT. Plasma uric acid is associated with increased risk of type 2 diabetes independent of diet and metabolic risk factors. J Nutr 2013; 143(1):80-5.
Kodama S, Saito K, Yachi Y, Asumi M, Sugawara A, Totsuka K, et al. Association between serum uric acid and development of type 2 diabetes. Diabetes Care. 2009;32(9):1737–42.
Bardin T, Richette P. Definition of hyperuricemia and gouty conditions. Curr Opin Rheumatol. 2014;26(2):186–91.
•• Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–49. This study reported that North America had the highest prevalence of diabetes from 1980 to 2013.
Yuan S, Larsson SC. An atlas on risk factors for type 2 diabetes: a wide-angled Mendelian randomisation study. Diabetologia. 2020;63(11):2359–71.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81.
•• Kumar S, Gupta R, Suppiah R. Gout in women: differences in risk factors in young and older women. N Z Med J. 2012;125(1363):39–45. A retrospective study showed that male patients with gout are more likely to be older than 50 years and use diuretics than female patients with gout.
•• Wallace KL, Riedel AA, Joseph-Ridge N, Wortmann R. Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol. 2004;31(8):1582–7. An important study demonstrated that the prevalence of gout or uric acid increases with age.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (grant number 81903302), the Young Elite Scientists Sponsorship Program by China Association for Science and Technology (grant number YESS20200151), and the 345 Talent Project of Shengjing Hospital of China Medical University (grant number M0294).
Author information
Authors and Affiliations
Contributions
Jinguo Jiang: Conceptualization, Formal analysis, Visualization, Writing-original draft. Tingjing Zhang: Writing-review & editing. Yashu Liu: Writing-review & editing. Qing Chang: Writing-review & editing. Yuhong Zhao: Writing-review & editing. Chuanji Guo: Conceptualization, Resources, Writing-review & editing, Supervision. Yang Xia: Conceptualization, Resources, Writing-review & editing, Supervision, Funding acquisition.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, J., Zhang, T., Liu, Y. et al. Prevalence of Diabetes in Patients with Hyperuricemia and Gout: A Systematic Review and Meta-analysis. Curr Diab Rep 23, 103–117 (2023). https://doi.org/10.1007/s11892-023-01506-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11892-023-01506-2