Abstract
Purpose of Review
For decades, the standard of care for stable ischemic heart disease (SIHD) has been an ischemia-centric approach based on largely observational data suggesting a survival benefit of revascularization in patients with moderate-or-severe ischemia. In this article, we will objectively review the evolution of the ischemia paradigm, the trial evidence comparing revascularization to medical therapy in SIHD, and what contemporary practice should be in 2022.
Recent Findings
Randomized trials, including COURAGE and, most recently, the ISCHEMIA trial, have shown no reduction in “hard outcomes” like death and myocardial infarction (MI) in SIHD compared to medical therapy. The trial excluded high-risk patients with left main disease, low ejection fraction (EF) < 35%, and severe unacceptable angina. Irrespective of the severity of ischemia and the extent of coronary artery disease (CAD), revascularization did not offer any prognostic advantage over medical therapy. On the other hand, there was a durable improvement in symptoms. While there are many caveats to the ISCHEMIA trial, the overall strengths of the trial outweigh these limitations. The findings of ISCHEMIA are consistent with previous trials.
Summary
It is time for the cardiology community to pivot towards medical therapy as the initial step for most patients with SIHD. Physicians should have the “COURAGE” to embrace “ISCHEMIA” and be comfortable with treating ischemia medically.
Similar content being viewed by others
Introduction
For nearly 50 years, cardiologists have taken an “ischemia-centric” approach towards managing stable ischemic heart disease (SIHD), with revascularization the preferred strategy for most patients. However, in the last 15 years, randomized trials have failed to show a reduction in “hard outcomes” with revascularization compared to medical therapy in stable coronary artery disease (CAD). The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial [1••] is the most current and pivotal study. This article will trace the origins of the ischemia paradigm, review the observational and trial evidence, and suggest a framework of what current practice should be in the light of these data.
The Ischemia Paradigm
For several decades, the ischemia paradigm has dominated the treatment and management of SIHD. Studies dating back to the 1970s demonstrated important adverse clinical outcomes in patients with a significantly abnormal exercise stress test [2, 3]. This ischemia paradigm was further cemented into clinical practice by the seminal work of Hachamovitch and colleagues, who demonstrated that the extent and severity of inducible ischemia had incremental prognostic value at any given clinical risk [4, 5]. Furthermore, the survival curves for medical therapy vs. revascularization were shown to diverge at an inflection point of a 10% ischemic burden, with a marked reduction in mortality with revascularization (2% vs. 6.7%; p < 0.0001) if the burden of ischemia crossed 20% [6]. Limitations to these data included the observational nature of the studies, conducted at a single center when neither medical therapy nor PCI were optimal compared to current standards. Nonetheless, based on these findings, stress testing has been used to guide treatment decisions for the invasive management of CAD for several decades. Indeed, the 2011 American College of Cardiology/American Heart Association (ACC/AHA) stable ischemic heart disease guidelines recommended revascularization over medical therapy for the vast majority of patients, giving coronary artery bypass graft surgery (CABG) a class I and percutaneous coronary intervention (PCI) a class IIb indication, reflecting the unequivocal acceptance of revascularization as a means to improve prognosis in CAD [7]. Furthermore, the 2017 Appropriate Use Criteria (AUC) for revascularization in SIHD gave a “maybe appropriate” to “appropriate” rating for revascularization in non-left main disease, depending on LAD involvement, diabetes status, and mode (PCI or CABG) chosen [8]. These guidelines reflect the long-standing “ischemia-centric” approach to CAD [9].
Landscape Preceding the ISCHEMIA Trial
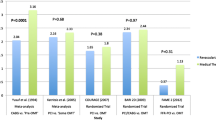
In the years following the Hachamavotich paper [6], several trials explored the role of medical therapy versus revascularization in patients with inducible ischemia based on stress testing. They failed to demonstrate a favorable effect of revascularization on hard endpoints like death or myocardial infarction (MI) (Table 1) [10–13]. The most seminal of these studies was the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial [12] which randomized 2287 patients with single or multivessel stable CAD to PCI with optimal medical therapy (OMT) vs. OMT alone. Patients with severe angina, markedly positive stress test, low ejection fraction (EF), or ventricular arrhythmias were excluded. At the initial 5-year follow-up [12] (and extended out to 15 years [14] ), there was no difference in death, MI, or hospitalization for acute coronary syndrome (ACS) in patients treated medically or with PCI. While an initial reduction in symptoms was seen at 1 and 3 years, at the 5-year mark, freedom from angina was essentially identical in both arms (74% vs. 72%). In the years following the publication of COURAGE, there was a visible reduction in PCI volumes for SIHD [15], albeit perhaps not as widespread as expected. Criticisms of the COURAGE trial included randomization of patients after angiography (thereby introducing biases, particularly of excluding complex and/or high-risk anatomy), exclusion of high-risk patients with severe angina and low EF, the fact that COURAGE was conducted in an era of bare metal stents and skepticism of the feasibility of OMT in the “real” world [16]. Parallel data from the Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME) 2 trial [17, 18] that compared PCI vs. medical therapy in patients with SIHD and an abnormal fractional flow reserve (FFR), an invasive surrogate for ischemia, indicated no conclusive benefit of revascularization. At 5 years, there was no difference in death (HR 0.98 [95% CI 0.55–1.75]) and a non-significant (albeit strong) trend of reduction in spontaneous MI (HR 0.66 [95% CI 0.43–1.00]). As with COURAGE, there was a higher rate of urgent revascularization, with at least half of the interventions being related to ACS. In the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI-2D) trial [13], over 2000 patients with diabetes and SIHD were first stratified into a revascularization strategy (CABG or PCI) based on anatomical suitability, following which each strategy was randomized to undergo revascularization or just OMT. At 5 years, there was no difference in mortality, although spontaneous MI was significantly reduced with revascularization (but only in the CABG stratum). Cumulatively, these studies challenged the notion that the adverse prognosis from ischemia was modifiable by revascularization, with benefits seen limited only to urgent revascularization, not the “hard” endpoints [19]. However, it was also clear that studies like COURAGE leaned towards the exclusion of very high-risk patients, with barely one-third of the cohort in the nuclear sub-study having moderate-or-severe ischemia [20]. Furthermore, close to 80% of patients in COURAGE had relatively less complex (single or double vessel) CAD [21].
ISCHEMIA Trial − Findings
Against this backdrop, guidelines and appropriate use criteria continued to recommend revascularization for prognosis in patients with an intermediate to high-risk stress test, highlighting the lack of equipoise in approaching these patients [8]. The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial [1••] was designed to address the shortfalls of the previous trials, specifically, whether revascularization improved outcomes, compared to medical therapy, in patients with SIHD and moderate-or-severe inducible ischemia. A total of 5179 patients with moderate-or-severe ischemia (core laboratory validated) were randomized (after a blinded cardiac computed tomography angiography [CTA] to exclude left main or non-obstructive disease) to an invasive strategy of revascularization with OMT vs. OMT alone. Very high-risk patients, including those with unacceptable angina despite medical therapy, EF < 35%, recent ACS or revascularization, and left main disease on a blinded cardiac CTA, were excluded. After a median follow-up of 3.2 years, there was no difference in the primary endpoint of cardiovascular death, MI, hospitalization for unstable angina, heart failure, or resuscitated cardiac arrest. All-cause or cardiac mortality was not different between the treatment groups. Revascularization conferred an early hazard of procedural MI (4.8% vs. 2.9%; ∆ = − 1.9% [− 0.9%, − 3.0%]) that was balanced by a late benefit for spontaneous MI (11.7% vs. 13.9%; ∆ = − 2.2% [− 4.4%, − 0.1%]). Although the “highest” risk patients were excluded from the trial to the investigators’ credit, this was a far sicker cohort than COURAGE with moderate or severe ischemia in ~ 80% of patients, multivessel disease in 77%, and close to 90% had involvement of the LAD. A striking finding of ISCHEMIA was that revascularization failed to show a benefit over medical therapy in subgroups unequivocally considered to benefit from CABG or PCI—those with extensive disease burden, severe ischemia, and involvement of the LAD. In a separate analysis, patients achieving complete revascularization, anatomic (43.6%), or functional (58.5%) appeared to fare significantly better than those who did not [22]; however, this analysis is subject to confounders and is, at best, hypothesis-generating. The only significant benefit of revascularization seen was durable improvement symptoms and quality of life scores [23], though, not surprisingly, the benefits were limited to the 21% of subjects with daily or weekly angina.
ISCHEMIA Trial − Caveats and Strengths
There are several caveats to the ISCHEMIA trial that need to be considered.
First, due to slow enrollment and funding constraints, the investigators were compelled to reduce the sample size from the originally planned 8000 to approximately 5000. Consequently, the primary endpoint was revised to a composite outcome to maintain statistical power. While, no doubt, this reduced the robustness of the trial, the investigators had well outlined the nuances and pragmatism behind this decision before the trial results were presented [24].
Second, close to 25% of the patients included were based on exercise testing without stress imaging. This was a step to improve recruitment and was not part of the initial design. The inclusion of such patients makes the enrolled population somewhat more heterogeneous. However, the exercise test criteria “were developed to approximate severe ischemia, taking into account the potentially higher false-positive rate.” The CTA inclusion criteria were more stringent (≥ 70% stenosis in the proximal or mid-epicardial vessels) to ensure that only those with severe ischemia were included when exercise testing was the basis of inclusion [25].
Third, although ISCHEMIA included a much higher risk group compared to previous trials, the lack of benefit of an invasive strategy may still have been the result of selecting a less severe cohort. The exclusion of patients with severe angina, low EF, and left main disease (8.7% of the enrolled cohort) clearly dilutes the risk. Furthermore, among the patients randomized, ~ 14% had mild or no ischemia, and only 44.8% had severe inducible ischemia [26]. In an analysis of the National Cardiovascular Data Registry CathPCI Registry representing contemporary practice in the USA, Chatterjee et al. found that barely one-third of patients undergoing PCI for SIHD would have met enrollment criteria for the ISCHEMIA trial [27]. Similar findings were reported by De Luca and colleagues from Europe, with only 4% of patients undergoing PCI for SIHD meeting “ISCHEMIA-like” criteria [28]. Moreover, the actual denominator of eligible patients who were not enrolled in the trial is unknown as no such registry was maintained. Although these data question the general applicability of the ISCHEMIA trial results to “every day” patients, the external validity of a > 5000 patient trial conducted in over 30 countries cannot be understated.
Fourth, over one-fourth of the patients randomized to an initial conservative strategy underwent unplanned angiography, and 21% underwent revascularization. These crossovers dilute the difference between the two study groups. Of course, this is inevitable in any such trial and does not take away from the fundamental premise of the trial—to determine whether an initial strategy of conservative management is similar to invasive treatment at the outset. The trial showed that for the majority, this initial strategy does not have to be an invasive one.
Finally, while a robust benefit on symptoms was seen in ISCHEMIA, the recent ORBITA trial [29••] suggested a significant placebo effect of PCI. In this relatively small study, patients randomized to both “real” and sham PCI showed an improvement in exercise time with no statistical difference between the two groups. Thus, a placebo effect may have played a role in improving symptoms in ISCHEMIA. That said, the durability of this benefit in ISCHEMIA is unlikely to be entirely a placebo effect.
At the same time, it is essential to appreciate the strengths of this trial. First, even though not as large as initially planned, ISCHEMIA is the largest trial ever conducted to compare revascularization with medical therapy in SIHD. Second, randomization occurred before angiography, mitigating some of the biases in COURAGE and other trials. Third, there was core laboratory interpretation of the stress testing data and rigorous adjudication of clinical events. Fourth, while perhaps the highest risk patients were excluded from the trial, ISCHEMIA enrolled a cohort that previously was unequivocally felt to benefit from revascularization [8]. Fifth, medical and interventional therapies in the trial were contemporary and well-executed. Finally, follow-up was > 90% in this trial.
Why was the ISCHEMIA Trial Not “Positive”
The critical question at hand is why, given the strong relationship between ischemia and prognosis, did outcomes fail to improve with revascularization. This brings us to the concept that ischemia represents different things in patients with ACS and SIHD, even though it confers an adverse prognosis in both situations (Fig. 1). In an ACS, ischemia reflects the biology of the acutely ruptured (or eroded) plaque wherein an often previously non-obstructive but “vulnerable” lesion (marked by inflammation, a lipid-rich core, and a thin cap) rapidly becomes flow limiting [30, 31]. That plaque is at high risk for occluding, resulting in an infarct. Revascularization, be it surgical or percutaneous, bypasses or “seals” that vulnerable plaque and prevents an early prognostic event. This is reflected in the large body of literature supporting revascularization in the setting of ACS [32, 33]. On the other hand, in SIHD, the plaque biology is different. These plaques lack the “vulnerable” features, have less inflammation, a thick cap, and are less prone to rupture [34]. Ischemia in this setting is a surrogate marker of the underlying disease—advanced atherosclerosis. The driver of prognosis is atherosclerosis (which is often diffuse), with ischemia predicting future ACS events often in locations remote from the ischemia-producing lesion [35]. Treating the “tight spot” relieves the symptoms of ischemia but does not change extensive atherosclerosis, unlike OMT. In an analysis of the differential impact of disease burden and degree of ischemia on prognosis in ISCHEMIA, Raynolds et al. [36] reported that the degree of ischemia was not associated with all-cause mortality (p for trend = 0.33) and only weakly related to myocardial infarction (p for trend = 0.04). On the other hand, the extent of CAD (defined by the modified Duke prognostic score) was strongly associated with both death (p for trend < 0.001) and myocardial infarction (p for trend < 0.001) [36]. Similar findings were noted in the ISCHEMIA-CKD trial [37]. More importantly, revascularization compared to medical therapy did not improve outcomes in patients with severe ischemia or extensive CAD, once again emphasizing that ischemia may not be a modifiable treatment target in SIHD [36].
Figure showing the differential implications of ischemia in SIHD (upper panel) and acute coronary syndrome (lower panel) (see text for details). Ischemia is associated with an adverse prognosis in both. While ischemia-producing lesions in SIHD may progress with time, the adverse prognosis is related to the larger number of mild plaques that have the propensity to destabilize and produce ACS. In ACS, ischemia represents the biology of the unstable plaque that may rapidly progress to an occlusive MI if not revascularized. While revascularization may mitigate this early risk, the longer term risk related to the other plaques persists, as does the risk of stent-related events. ACS, acute coronary syndrome; NIH, neointimal hyperplasia
Putting ISCHEMIA and Other Trials Together
It is time for cardiologists to move away from an “ischemia-centric” approach in SIHD and target the disease (atherosclerosis) rather than the marker (ischemia). ISCHEMIA has demonstrated that patients fitting the trial inclusion criteria can be treated safely with medical therapy even with severe ischemia. Thus, anatomic definition to rule out left main stenosis and left ventricular imaging to assess EF would be necessary to choose the right patients with ischemia for an initial strategy of medical therapy. The former is of particular importance as the finding of significant left main disease in a patient with severe ischemia in an unrelated territory is not an uncommon experience (Fig. 2).
A 57-year-old man presented with “atypical chest pain.” Pharmacological stress myocardial perfusion scan demonstrates a large area of severe inducible ischemia in the inferior/inferolateral wall. The patient was referred for cardiac CT angiography, which was considerably delayed at the height of the COVID-19 pandemic. He presented 6 months later with acute coronary syndrome. Angiography revealed critical left main disease (white arrow), severe disease in the left anterior descending artery (double arrows), and an occluded right coronary artery that was filled via L-R collaterals (asterisk)
A proposed approach is outlined in Fig. 3, wherein several “nodes” of decision-making can be visualized. Central to the evaluation of a patient with chest pain is the initial history and physical examination. For a small minority of patients, a history diagnostic of accelerating and/or unstable symptoms will offer the first node of decision-making, and catheterization would be the next appropriate step. For the rest, stress testing would mark the next decision node, ideally with imaging to enable ventricular function assessment. A “profoundly” abnormal stress test (for example, exercise-induced hypotension, severe chest pain, early-onset widespread EKG changes, or ST-segment elevation with stress) would prompt referral for angiography and likely revascularization. For the rest, the test will either be normal or abnormal (but not “profoundly”). Those with no or mild ischemia would be appropriate to treat medically without further evaluation unless symptoms are limiting. A significant number will have moderate or severe ischemia, which will present the clinician with the third decision point (Fig. 3). In the days before ISCHEMIA, these patients would be referred for catheterization and revascularization based on prevailing guidelines. Following the ISCHEMIA trial, there is enough equipoise between medical therapy and revascularization to allow a discussion with the patient regarding testing to exclude left main disease. This will need to be a shared decision-making event with the patient, and no doubt, some patients will prefer the more invasive approach and should be referred for angiography. The rest could be imaged with a cardiac CTA. A minority will have left main disease and should undergo cardiac catheterization, while the majority with no left main stenosis could be treated medically. Following initiation of medical therapy, the clinician is faced with the final decision node—recurrence of symptoms and failure of medical treatment for which angiography and revascularization would be the next step. Thus, as shown in Fig. 3, most patients with chest pain and SIHD can be managed with an initial strategy of medical therapy. Key elements modulating the entire decision-making process are the extent of symptoms, left ventricular function, and patient preference.
Figure showing a proposed algorithm for evaluating and managing chest pain in patients with stable coronary artery disease, incorporating a non “ischemia-centric” approach. Numbers point to “nodes” of decision-making (see text for details). EF, ejection fraction; MOD, moderate; CTA, CT angiography; RX, therapy
Should Ischemia Testing Be Replaced by Anatomical Testing?
Should cardiac CTA replace stress testing? Given the more robust prognostic value of the extent of anatomic disease over ischemic burden [36], this may seem reasonable. Indeed, the UK National Institute for Health and Care Excellence (NICE) recommended cardiac CTA as the first-line test for SIHD back in 2016 [38]. More recently, the ACC/AHA/SCAI chest pain guidelines also suggested cardiac CTA maybe a reasonable initial choice for evaluating chest pain [39•]. It is important to note, however, that ISCHEMIA did not test the question of functional vs. anatomical imaging, and any extrapolations would be spurious. While it may be plausible to make a switch to anatomical (CTA) imaging, there are several reasons why this may not be feasible. First, at least in the USA, there is limited availability of CTA services [41] compared to stress testing. Second, cardiac CTA is often technically challenging in many patients—particularly those with renal impairment, inability to comply with breath-holding, elevated and irregular heart rates, and extensive calcium precluding evaluation of segments. However, more modern scanners can overcome heart rate issues quite effectively. Furthermore, the left main is a large vessel and less prone to motion artifacts. Thus, uninterpretable segments in the remaining tree (due to motion or calcium) may be irrelevant if left main disease can be confidently excluded, as the initial approach would be medical regardless of the remaining anatomy. Third, the added prognostic value of exercise testing and left ventricular function assessment during stress imaging adds considerable value to the evaluation. Finally, with the increasing availability of hybrid SPECT-CT machines [42], SPECT imaging can now be enhanced with an estimate of coronary calcium, creating an optimal “blend” of functional and anatomical assessment. Thus, for availability and pragmatic reasons, ischemia testing will continue to provide a good starting point for chest pain evaluation, and it is unlikely to be replaced by anatomical testing [43].
Where Should Things Stand in 2022?
The ischemia paradigm has had a good run for several decades. In patients with SIHD and moderate-or-severe ischemia, revascularization provides durable symptomatic relief, especially in those with significant angina at the outset. However, it confers no clear prognostic benefit irrespective of ischemic burden. The caveats are that the highest risk patients (severe symptoms, recent ACS, heart failure, low EF, and left main disease) were excluded from the trial. In 2022, medical therapy for SIHD is reasonable as an initial step if prognosis is the concern—as long the patient does not fit any of the exclusions. However, in 2022, revascularization for SIHD is also reasonable as an initial step if symptoms are compelling. While there may not be a prognostic benefit, improving quality of life is as important a goal of therapy as enhancing prognosis is. For ACS, revascularization should continue to be the initial approach for most patients. Guidelines continue to give considerable importance to ischemic burden, and the most recent European guidelines give revascularization in patients with a large territory of ischemia (> 10% myocardium) a class I indication [44]. However, it is encouraging that the most recent iteration of the ACC/AHA revascularization guidelines [40] downgraded revascularization (via either CABG or PCI) in patients with non-left main SIHD and normal EF to a class IIB indication, representing a change from the prior 2011 CABG guidelines [45].
Have We Come Full Circle?
Following the ISCHEMIA trial, it may appear to the casual observer that the concept of medical therapy for SIHD is a novel and ground-breaking idea. The fact is that even in the Coronary Artery Surgery Study (CASS), a randomized trial conducted in the 1970s comparing medical therapy to CABG in patients with SIHD but without severe left main disease or low EF (< 35%), at 5-year revascularization was not superior to medical therapy in reducing the risk of death or MI. This was when medical therapy was vastly inferior to current standards, consisting mainly of beta-blockers and nitrates [46]. The authors concluded that “patients similar to those enrolled in this trial can safely defer bypass surgery until symptoms worsen to the point that surgical palliation is required” [47]. At longer term follow-up, a survival benefit became apparent, but only in high-risk subsets of patients with proximal LAD stenosis ≥ 70% and a low EF (< 50%) or the group with triple vessel disease and low EF (< 50%) [48]. Lown and colleagues reported in 1981 that patients with “profound ST-segment depression” on exercise did not fare better with CABG compared to medical therapy of that time [49]. Thus, we have come full circle from a time when the evidence suggested that a large number of patients with SIHD could be managed without revascularization unless symptoms were compelling, to a period when observational data suggested a significant prognostic benefit of revascularization, to the ISCHEMIA era where a revascularization-driven ischemia-centric approach does not alter prognosis in most patients.
Dogmatism vs. Pragmatism
As is always the case in medicine, it is important to refrain from dogma and adopt a pragmatic and balanced approach as there is never a “one size fits all” approach for all patients. ISCHEMIA shows that an initial strategy of medical therapy in SIHD is not prognostically adverse even in patients with moderate or severe inducible ischemia. That said, it is likely that the highest risk patients were not part of the trial. This is particularly probable in countries participating in ISCHEMIA where revascularization is widely available and thresholds to proceed are relatively low. Therefore, for some patients with “extensive” inducible ischemia, physician judgment based on tangible and intangible variables may still prompt an initial invasive strategy. Appropriate patient engagement would be of vital importance in such cases. Furthermore, although ISCHEMIA failed to demonstrate an overall reduction in MI, the trial did show a reduction in spontaneous MI in the invasive arm—it just happened to be counterbalanced by an increase in procedural infarction. It continues to be debated whether periprocedural MI should be part of an endpoint because of its sensitivity to different definitions and the fact that only very large MIs are truly prognostic [50]. On the other hand, the importance of spontaneous MI is largely uncontested. Trials like BARI-2D [13] (significant reduction) and FAME 2 [17, 18] (trend) have also suggested that fewer spontaneous MIs occur in patients undergoing revascularization. Whether this reduction in spontaneous MI is truly a revascularization effect or is just ascertainment bias (which may prompt a diagnosis of MI more often in non-revascularized patients) is difficult to tease out. Hence, it is prudent to avoid being dogmatic about no benefit of revascularization as long-term follow-up of the ISCHEMIA cohort may show a late signal of benefit. The ISCHEMIA-EXTENDed study will hopefully shed more light on this in the years to come [51].
Conclusion
It is time for the cardiology community to pivot towards medical therapy as the initial step for most patients with SIHD. Physicians should have the “COURAGE” to embrace “ISCHEMIA” and be comfortable treating SIHD medically. At the same time, cardiologists should not be discouraged from offering revascularization when symptoms are limiting—it is “okay” to improve a patient’s quality of life. It is also important to understand that while revascularization was not superior, it was not inferior to medical therapy either. As is the case with most therapies, it comes down to a candid and transparent discussion with the patient regarding benefits and risks in a shared decision-making process. A final and rather sobering fact is that the 5-year “hard” event rate (death/MI) was ~ 20% in COURAGE and ~ 15% in ISCHEMIA—despite excellent therapy in a controlled trial setting. Clearly, a lot more needs to be done to improve these outcomes.
Abbreviations
- ACC:
-
American College of Cardiology
- ACS:
-
Acute coronary syndrome
- AHA:
-
American Heart Association
- AUC:
-
Appropriate use criteria
- BARI-2D:
-
Bypass angioplasty revascularization investigation 2 diabetes
- CABG:
-
Coronary artery bypass surgery
- CAD:
-
Coronary artery disease
- COURAGE:
-
Clinical outcomes utilizing revascularization and aggressive drug evaluation
- CTA:
-
Computed tomography angiography
- EF:
-
Ejection fraction
- FAME:
-
Fractional flow reserve versus angiography for multivessel evaluation
- ISCHEMIA:
-
International study of comparative health effectiveness with medical and invasive approaches
- MI:
-
Myocardial infarction
- OMT:
-
Optimal medical therapy
- PCI:
-
Percutaneous coronary intervention
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395–1407. Pivotal trial, demonstrating in a large randomized cohort that revascularization was not superior to medical therapy in patients with moderate-severe ischemia, but without left main disease or low ejection fraction.
Ellestad MH, Wan MK. Predictive implications of stress testing. Follow-up of 2700 subjects after maximum treadmill stress testing. Circulation. 1975;51(2):363–369.
Cole JP, Ellestad MH. Significance of chest pain during treadmill exercise: correlation with coronary events. Am J Cardiol. 1978;41(2):227–32.
Berman DS, Hachamovitch R. Risk assessment in patients with stable coronary artery disease: incremental value of nuclear imaging. J Nucl Cardiol. 1996;3(6 Pt 2):S41-49.
Hachamovitch R, Berman DS, Kiat H, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease: incremental prognostic value and use in risk stratification. Circulation. 1996;93(5):905–14.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107(23):2900–7.
Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60(24):2564–603.
Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2017;69(17):2212–41.
Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;64(18):1929–49.
Hambrecht R, Walther C, Mobius-Winkler S, et al. Percutaneous coronary angioplasty compared with exercise training in patients with stable coronary artery disease: a randomized trial. Circulation. 2004;109(11):1371–8.
Hueb W, Lopes NH, Gersh BJ, et al. Five-year follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2007;115(9):1082–9.
Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503–16.
Group BDS, Frye RL, August P, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360(24):2503–15.
Sedlis SP, Hartigan PM, Teo KK, et al. Effect of PCI on long-term survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373(20):1937–46.
Howard DH, Shen YC. Trends in PCI volume after negative results from the COURAGE trial. Health Serv Res. 2014;49(1):153–70.
Maron DJ, Boden WE, Weintraub WS, Calfas KJ, O’Rourke RA. Is optimal medical therapy as used in the COURAGE trial feasible for widespread use? Curr Treat Options Cardiovasc Med. 2011;13(1):16–25.
Xaplanteris P, Fournier S, Pijls NHJ, et al. Five-year outcomes with PCI guided by fractional flow reserve. N Engl J Med. 2018;379(3):250–9.
De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991–1001.
Stergiopoulos K, Boden WE, Hartigan P, et al. Percutaneous coronary intervention outcomes in patients with stable obstructive coronary artery disease and myocardial ischemia: a collaborative meta-analysis of contemporary randomized clinical trials. JAMA Intern Med. 2014;174(2):232–40.
Shaw LJ, Weintraub WS, Maron DJ, et al. Baseline stress myocardial perfusion imaging results and outcomes in patients with stable ischemic heart disease randomized to optimal medical therapy with or without percutaneous coronary intervention. Am Heart J. 2012;164(2):243–50.
Mancini GB, Bates ER, Maron DJ, et al. Quantitative results of baseline angiography and percutaneous coronary intervention in the COURAGE trial. Circ Cardiovasc Qual Outcomes. 2009;2(4):320–7.
Stone GW. Impact of completeness of revascularization on clinical outcomes with stable ischemic heart disease treated with an invasive versus conservative strategy: the ISCHEMIA trial. In: Presented at: ACC 2021 May 17, 2021. 2021.
Spertus JA, Jones PG, Maron DJ, et al. Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med. 2020;382(15):1408–19.
Maron DJ, Harrington RA, Hochman JS. Planning and conducting the ISCHEMIA trial. Circulation. 2018;138(14):1384–6.
Group ITR, Maron DJ, Hochman JS, et al. International study of comparative health effectiveness with medical and invasive approaches (ISCHEMIA) trial: rationale and design. Am Heart J. 2018;201:124–35.
Hochman JS, Reynolds HR, Bangalore S, et al. Baseline Characteristics and risk profiles of participants in the ISCHEMIA randomized clinical trial. JAMA Cardiol. 2019;4(3):273–86.
Chatterjee S, Fanaroff AC, Parzynski C, et al. Comparison of patients undergoing percutaneous coronary intervention in contemporary U.S. practice with ISCHEMIA trial population. JACC Cardiovasc Interv. 2021;14(21):2344–2349.
De Luca L, Uguccioni M, Meessen J, et al. External applicability of the ISCHEMIA trial: an analysis of a prospective, nationwide registry of patients with stable coronary artery disease. EuroIntervention. 2020;16(12):e966–73.
•• Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018;391(10115)31–40. Important study demonstrating, for the first time, a placebo effect of PCI on symptoms in patients with stable ischemic heart disease.
Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000;20(5):1262–75.
Crea F, Libby P. Acute coronary syndromes: the way forward from mechanisms to precision treatment. Circulation. 2017;136(12):1155–66.
Bavry AA, Kumbhani DJ, Rassi AN, Bhatt DL, Askari AT. Benefit of early invasive therapy in acute coronary syndromes: a meta-analysis of contemporary randomized clinical trials. J Am Coll Cardiol. 2006;48(7):1319–25.
Hansen KW, Sorensen R, Madsen M, et al. Effectiveness of an early versus a conservative invasive treatment strategy in acute coronary syndromes: a nationwide cohort study. Ann Intern Med. 2015;163(10):737–46.
Davies MJ. A macro and micro view of coronary vascular insult in ischemic heart disease. Circulation. 1990;82(3 Suppl):II38–46.
Gersh BJ, Boden WE, Bhatt DL, Stone PH, Crea F, Luscher TF. To stent or not to stent? Treating angina after ISCHEMIA-introduction. Eur Heart J. 2021;42(14):1387–8.
Reynolds HR, Shaw LJ, Min JK, et al. Outcomes in the ISCHEMIA trial based on coronary artery disease and ischemia severity. Circulation. 2021;144(13):1024–38.
Bainey KR, Fleg JL, Hochman JS, et al. Predictors of outcome in the ISCHEMIA-CKD trial: anatomy versus ischemia. Am Heart J. 2022;243:187–200.
Moss AJ, Williams MC, Newby DE, Nicol ED. The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep. 2017;10(5):15.
• Writing Committee M, Gulati M, Levy PD, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Cardiovasc Comput Tomogr. 2022;16(1):54-122. Most recent chest pain guidelines.
Writing Committee M, Lawton JS, Tamis-Holland JE, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2022;79(2):e21–129.
Goldfarb JW, Weber J. Trends in cardiovascular MRI and CT in the U.S. Medicare population from 2012 to 2017. Radiol Cardiothorac Imaging. 2021;3(1):e200112.
Dorbala S, Di Carli MF, Delbeke D, et al. SNMMI/ASNC/SCCT guideline for cardiac SPECT/CT and PET/CT 1.0. J Nucl Med. 2013;54(8):1485–1507.
Thompson RC, Al-Mallah MH, Beanlands RSB, et al. ASNC’s thoughts on the AHA/ACC chest pain guidelines. J Nucl Cardiol. 2022;29(1):19–23.
Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165.
Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2011;58(24):e123–210.
Investigators CP, Their A. Myocardial infarction and mortality in the coronary artery surgery study (CASS) randomized trial. N Engl J Med. 1984;310(12):750–8.
Coronary artery surgery study (CASS). a randomized trial of coronary artery bypass surgery. Survival data. Circulation. 1983;68(5):939–950.
Chaitman BR, Ryan TJ, Kronmal RA, Foster ED, Frommer PL, Killip T. Coronary artery surgery study (CASS): comparability of 10 year survival in randomized and randomizable patients. J Am Coll Cardiol. 1990;16(5):1071–8.
Podrid PJ, Graboys TB, Lown B. Prognosis of medically treated patients with coronary-artery disease with profound ST-segment depression during exercise testing. N Engl J Med. 1981;305(19):1111–6.
McCarthy CP, Januzzi JL. Periprocedural MI as an endpoint in clinical trials. J Am Coll Cardiol. 2022;79(6):527–9.
ISCHEMIA-EXTENDed Follow-up. In: https://ClinicalTrials.gov/show/NCT04894877. Accessed 6 Jan 2022.
Author information
Authors and Affiliations
Contributions
AHJ contributed significantly to the manuscript by creating trial summaries, Table 1, and Figs. 1 and 2. AHJ also wrote initial drafts of several important portions of the manuscript. AHJ also assisted in proofreading the manuscript and double-checking the references. FHJ wrote the major share of the manuscript and conceptualized the outline and structure of the paper.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Public Health Policy
Rights and permissions
About this article
Cite this article
Jafary, F.H., Jafary, A.H. Ischemia Trial: Does the Cardiology Community Need to Pivot or Continue Current Practices?. Curr Cardiol Rep 24, 1059–1068 (2022). https://doi.org/10.1007/s11886-022-01725-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-022-01725-1