Abstract
Purpose of Review
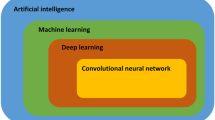
This paper investigates present uses and future potential of artificial intelligence (AI) applied to intracoronary imaging technologies.
Recent Findings
Advances in data analytics and digitized medical imaging have enabled clinical application of AI to improve patient outcomes and reduce costs through better diagnosis and enhanced workflow. Applications of AI to IVUS and IVOCT have produced improvements in image segmentation, plaque analysis, and stent evaluation. Machine learning algorithms are able to predict future coronary events through the use of imaging results, clinical evaluations, laboratory tests, and demographics.
Summary
The application of AI to intracoronary imaging holds significant promise for improved understanding and treatment of coronary heart disease. Even in these early stages, AI has demonstrated the ability to improve the prediction of cardiac events. Large curated data sets and databases are needed to speed the development of AI and enable testing and comparison among algorithms.






Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hanekamp C, Koolen J, Pijls N, Michels H, Bonnier H. Comparison of quantitative coronary angiography, intravascular ultrasound, and coronary pressure measurement to assess optimum stent deployment. Circulation. 1999;99:1015–21.
Kim S-W, Mintz GS, Ohlmann P, Hassani S-E, Fernandez S, Lu L, et al. Frequency and severity of plaque prolapse within cypher and taxus stents as determined by sequential intravascular ultrasound analysis. Am J Cardiol. 2006;98:1206.
Cook S, Wenaweser P, Togni M, Billinger M, Morger C, Seiler C, et al. Incomplete stent apposition and very late stent thrombosis after drug-eluting stent implantation. Circulation. 2007;115:2426–34. https://doi.org/10.1161/circulationaha.106.658237.
Mehta SK, McCrary JR, Frutkin AD, Dolla WJS, Marso SP. Intravascular ultrasound radiofrequency analysis of coronary atherosclerosis: an emerging technology for the assessment of vulnerable plaque. Eur Heart J. 2007;28:1283–8. https://doi.org/10.1093/eurheartj/ehm112.
Siqueira DA, Abizaid AA, Costa Jd R, Feres F, Mattos LA, Staico R, et al. Late incomplete apposition after drug-eluting stent implantation: incidence and potential for adverse clinical outcomes. Eur Heart J. 2007;28:1304–9. https://doi.org/10.1093/eurheartj/ehm114.
Feres F, Costa JR, Abizaid A. Very late thrombosis after drug-eluting stents. Catheter Cardiovasc Interv. 2006;68:83–8.
Bouma BE, Tearney GJ, Yabushita H, Shishkov M, Kauffman CR, DeJoseph Gauthier D, et al. Evaluation of intracoronary stenting by intravascular optical coherence tomography. Heart. 2003;89:317–20. https://doi.org/10.1136/heart.89.3.317.
Pinto TL, Waksman R. Clinical applications of optical coherence tomography. J Interv Cardiol. 2006;19:566.
Jeremias A, Sylvia B, Bridges J, Kirtane AJ, Bigelow B, Pinto DS, et al. Stent thrombosis after successful sirolimus-eluting stent implantation. Circulation. 2004;109:1930–2. https://doi.org/10.1161/01.cir.0000127105.99982.21.
Guagliumi G, Sirbu V. Optical coherence tomography: high resolution intravascular imaging to evaluate vascular healing after coronary stenting. Catheter Cardiovasc Interv. 2008;72:237–47.
Hong SJ, Kim BK, Shin DH, Nam CM, Kim JS, Ko YG, et al. Effect of intravascular ultrasound-guided vs angiography-guided everolimus-eluting stent implantation: the IVUS-XPL randomized clinical trial. JAMA. 2015;314:2155–63. https://doi.org/10.1001/jama.2015.15454.
Kataoka Y, Puri R, Andrews J, Honda S, Nishihira K, Asaumi Y, et al. In vivo visualization of lipid coronary atheroma with intravascular near-infrared spectroscopy. Expert Rev Cardiovasc Ther. 2017;15:775–85. https://doi.org/10.1080/14779072.2017.1367287.
Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–35. https://doi.org/10.1056/NEJMoa1002358.
Wu B, Abbott T, Fishman D, McMurray W, Mor G, Stone K, et al. Comparison of statistical methods for classification of ovarian cancer using mass spectrometry data. Bioinformatics (Oxford, England). 2003;19:1636–43. https://doi.org/10.1093/bioinformatics/btg210.
Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographsaccuracy of a deep learning algorithm for detection of diabetic retinopathyaccuracy of a deep learning algorithm for detection of diabetic retinopathy. JAMA. 2016;316:2402–10. https://doi.org/10.1001/jama.2016.17216.
Berner ES, Ozaydin B. Benefits and risks of machine learning decision support systems benefits and risks of machine learning decision support systems letters. JAMA. 2017;318:2353–4. https://doi.org/10.1001/jama.2017.16619.
Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115–8. https://doi.org/10.1038/nature21056.
Zhu L, Zheng WJ. Informatics, data science, and artificial intelligence informatics, data science, and artificial intelligence informatics, data science, and artificial intelligence. JAMA. 2018;320:1103–4. https://doi.org/10.1001/jama.2018.8211.
Naylor CD. On the prospects for a (deep) learning health care system prospects for a deep learning health care system prospects for a deep learning health care system. JAMA. 2018;320:1099–100. https://doi.org/10.1001/jama.2018.11103.
Hinton G. Deep learning—a technology with the potential to transform health carethe potential of deep learning technology to transform health care the potential of deep learning technology to transform health care. JAMA. 2018;320:1101–2. https://doi.org/10.1001/jama.2018.11100.
Carin L, Pencina MJ. On deep learning for medical image analysis on deep learning for medical image analysis on deep learning for medical image analysis. JAMA. 2018;320:1192–3. https://doi.org/10.1001/jama.2018.13316.
Gianfrancesco MA, Tamang S, Yazdany J, Schmajuk G. Potential biases in machine learning algorithms using electronic health record data potential biases in machine learning algorithms using electronic health record data potential biases in machine learning algorithms using electronic health record data. JAMA Intern Med. 2018;178:1544–7. https://doi.org/10.1001/jamainternmed.2018.3763.
Hatt M, Parmar C, Qi J, Naqa IE. Machine (deep) learning methods for image processing and radiomics. IEEE Transactions on Radiation and Plasma Medical Sciences. 2019;3:104–8. https://doi.org/10.1109/TRPMS.2019.2899538.
Yan J, Yang X, Sun X, Chen Z, Liu H. A lightweight ultrasound probe for wearable human–machine interfaces. IEEE Sensors J. 2019;19:5895–903. https://doi.org/10.1109/JSEN.2019.2905243.
Tweedy L, Witzel P, Heinrich D, Insall RH, Endres RG. Screening by changes in stereotypical behavior during cell motility. Sci Rep. 2019;9:8784. https://doi.org/10.1038/s41598-019-45305-w.
Lou B, Doken S, Zhuang T, Wingerter D, Gidwani M, Mistry N, et al. An image-based deep learning framework for individualising radiotherapy dose: a retrospective analysis of outcome prediction. The Lancet Digital Health. 2019;1:e136–47. https://doi.org/10.1016/S2589-7500(19)30058-5.
Eraslan G, Avsec Z, Gagneur J, Theis FJ. Deep learning: new computational modelling techniques for genomics. Nat Rev Genet. 2019;20:389–403. https://doi.org/10.1038/s41576-019-0122-6.
Mintz GS, Nissen SE, Anderson WD, Bailey SR, Erbel R, Fitzgerald PJ, et al. American College of Cardiology clinical expert consensus document on standards for acquisition, measurement and reporting of intravascular ultrasound studies (ivus): a report of the american college of cardiology task force on clinical expert consensus documents developed in collaboration with the european society of cardiology endorsed by the society of cardiac angiography and interventions. J Am Coll Cardiol. 2001;37:1478–92.
Nair A, Kuban BD, Obuchowski N, Vince DG. Assessing spectral algorithms to predict atherosclerotic plaque composition with normalized and raw intravascular ultrasound data. Ultrasound Med Biol. 2001;27:1319–31.
• Nair A, Kuban BD, Tuzcu EM, Schoenhagen P, Nissen SE, Vince DG. Coronary plaque classification with intravascular ultrasound radiofrequency data analysis. Circulation. 2002;106:2200–6. https://doi.org/10.1161/01.cir.0000035654.18341.5e. Successful clinical implementation of AI for intra-coronary imaging which added previously unavailable information and reduced subjectivity in image interpretation.
Nair A, Margolis MP, Kuban BD, Vince DG. Automated coronary plaque characterisation with intravascular ultrasound backscatter: ex vivo validation. EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2007a;3:113.
Nissen SE. Atherosclerosis in 2010: new therapeutic insights. Nat Rev Cardiol. 8:70–2.
Nicholls SJ, Uno K, Tuzcu EM, Nissen SE. Lessons from coronary intravascular ultrasound on the importance of raising high-density lipoprotein cholesterol. Curr Atheroscler Rep. 12:301–7. https://doi.org/10.1007/s11883-010-0125-4.
Lavoie AJ, Bayturan O, Uno K, Hsu A, Wolski K, Schoenhagen P, et al. Plaque progression in coronary arteries with minimal luminal obstruction in intravascular ultrasound atherosclerosis trials. Am J Cardiol. 105:1679–83. https://doi.org/10.1016/j.amjcard.2010.01.345.
Nicholls SJ, Hsu A, Wolski K, Hu B, Bayturan O, Lavoie A, et al. Intravascular ultrasound-derived measures of coronary atherosclerotic plaque burden and clinical outcome. J Am Coll Cardiol. 55:2399–407. https://doi.org/10.1016/j.jacc.2010.02.026.
Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis. JAMA. 2006;295:1556–65. https://doi.org/10.1001/jama.295.13.jpc60002.
Nissen SE, Tuzcu EM, Schoenhagen P, Brown BG, Ganz P, Vogel RA, et al. Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis. JAMA. 2004;291:1071–80. https://doi.org/10.1001/jama.291.9.1071.
Andrews J, Puri R, Kataoka Y, Nicholls SJ, Psaltis PJ. Therapeutic modulation of the natural history of coronary atherosclerosis: lessons learned from serial imaging studies. Cardiovasc Diagn Ther. 2016;6:282–303. https://doi.org/10.21037/cdt.2015.10.02.
Ako J, Morino Y, Honda Y, Hassan A, Sonoda S, Yock PG, et al. Late incomplete stent apposition after sirolimus-eluting stent implantation: a serial intravascular ultrasound analysis. J Am Coll Cardiol. 2005;46:1002–5. https://doi.org/10.1016/j.jacc.2005.05.068.
Mintz GS, Shah VM, Weissman NJ. Regional remodeling as the cause of late stent malapposition. Circulation. 2003;107:2660–3. https://doi.org/10.1161/01.cir.0000074778.46065.24.
Hong M-K, Mintz GS, Lee CW, Kim Y-H, Lee S-W, Song J-M, et al. Incidence, mechanism, predictors, and long-term prognosis of late stent malapposition after bare-metal stent implantation. Circulation. 2004;109:881–6. https://doi.org/10.1161/01.cir.0000116751.88818.10.
Costa MA, Angiolillo DJ, Tannenbaum M, Driesman M, Chu A, Patterson J, et al. Impact of Stent Deployment Procedural Factors on Long-Term Effectiveness and Safety of Sirolimus-Eluting Stents (Final Results of the Multicenter Prospective STLLR Trial). Am J Cardiol. 2008;101:1704–11.
Matsumoto D, Shite J, Shinke T, Otake H, Tanino Y, Ogasawara D, et al. Neointimal coverage of sirolimus-eluting stents at 6-month follow-up: evaluated by optical coherence tomography. Eur Heart J. 2007;28:961–7. https://doi.org/10.1093/eurheartj/ehl413.
Kawase Y, Hoshino K, Yoneyama R, McGregor J, Hajjar RJ, Jang I-K, et al. In vivo volumetric analysis of coronary stent using optical coherence tomography with a novel balloon occlusion-flushing catheter: a comparison with intravascular ultrasound. Ultrasound Med Biol. 2005;31:1343.
Kume T, Akasaka T, Kawamoto T, Watanabe N, Toyota E, Neishi Y, et al. Assessment of coronary arterial plaque by optical coherence tomography. Am J Cardiol. 2006;97:1172.
Madjid M, Zarrabi A, Litovsky S, Willerson JT, Casscells W. Finding vulnerable atherosclerotic plaques: is it worth the effort? Arterioscler Thromb Vasc Biol. 2004;24:1775–82. https://doi.org/10.1161/01.atv.0000142373.72662.20.
Stamper D, Weissman NJ, Brezinski M. Plaque characterization with optical coherence tomography. J Am Coll Cardiol. 2006;47:69–79.
Puri R, Worthley MI, Nicholls SJ. Intravascular imaging of vulnerable coronary plaque: current and future concepts. Nat Rev Cardiol. 2011;8:131–9.
Oemrawsingh RM, Garcia-Garcia HM, van Geuns RJ, Lenzen MJ, Simsek C, de Boer SP, et al. Integrated Biomarker and Imaging Study 3 (IBIS-3) to assess the ability of rosuvastatin to decrease necrotic core in coronary arteries. EuroIntervention : journal of EuroPCR in collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2016;12:734–9. https://doi.org/10.4244/eijv12i6a118.
Jaguszewski M, Klingenberg R, Landmesser U. Intracoronary near-infrared spectroscopy (NIRS) imaging for detection of lipid content of coronary plaques: current experience and future perspectives. Curr Cardiovasc Imaging Rep. 2013;6:426–30. https://doi.org/10.1007/s12410-013-9224-2.
Michail M, Serruys PW, Stettler R, Crake T, Torii R, Tenekecioglu E, et al. Intravascular multimodality imaging: feasibility and role in the evaluation of coronary plaque pathology. Eur Heart J Cardiovasc Imaging. 2017;18:613–20. https://doi.org/10.1093/ehjci/jew330.
Fard AM, Vacas-Jacques P, Hamidi E, Wang H, Carruth RW, Gardecki JA, et al. Optical coherence tomography--near infrared spectroscopy system and catheter for intravascular imaging. Opt Express. 2013;21:30849–58. https://doi.org/10.1364/oe.21.030849.
Kanwar SS, Stone GW, Singh M, Virmani R, Olin J, Akasaka T, et al. Acute coronary syndromes without coronary plaque rupture. Nat Rev Cardiol. 2016;13:257–65. https://doi.org/10.1038/nrcardio.2016.19.
Libby P, Pasterkamp G, Crea F, Jang I-K. Reassessing the mechanisms of acute coronary syndromes. Circ Res. 2019;124:150–60. https://doi.org/10.1161/CIRCRESAHA.118.311098.
Ahmadi A, Stone GW, Leipsic J, Shaw LJ, Villines TC, Kern MJ, et al. Prognostic determinants of coronary atherosclerosis in stable ischemic heart disease: anatomy, physiology, or morphology? Circ Res. 2016;119:317–29. https://doi.org/10.1161/CIRCRESAHA.116.308952.
• Partida RA, Libby P, Crea F, Jang IK. Plaque erosion: a new in vivo diagnosis and a potential major shift in the management of patients with acute coronary syndromes. Eur Heart J. 2018;39:2070–6. https://doi.org/10.1093/eurheartj/ehx786. Review of plaque rupture and plaque erosion suggesting that plaque erosion should be treated pharmacologically rather than mechanically, highlighting the need for IC imaging to determine rupture vs erosion.
Burke A, Virmani R. Pathophysiology of acute myocardial infarction. Med Clin North Am. 2007;91:553–72.
Burke A, Virmani R, Galis Z, Haudenschild C, Muller J. Task force #2--what is the pathologic basis for new atherosclerosis imaging techniques? J Am Coll Cardiol. 2003;41:1874–86.
Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47:C13–8. https://doi.org/10.1016/j.jacc.2005.10.065.
Narula J, Nakano M, Virmani R, Kolodgie FD, Petersen R, Newcomb R, et al. Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J Am Coll Cardiol. 2013;61:1041–51. https://doi.org/10.1016/j.jacc.2012.10.054.
Otsuka F, Joner M, Prati F, Virmani R, Narula J. Clinical classification of plaque morphology in coronary disease. Nat Rev Cardiol. 2014;11:379–89. https://doi.org/10.1038/nrcardio.2014.62.
Hellings WE, Peeters W, Moll FL, Piers SR, van Setten J, Van der Spek PJ, et al. Composition of carotid atherosclerotic plaque is associated with cardiovascular outcome: a prognostic study. Circulation. 2010;121:1941–50. https://doi.org/10.1161/CIRCULATIONAHA.109.887497.
Ritman EL, Lerman A. The dynamic vasa vasorum. Cardiovasc Res. 2007;75:649–58. https://doi.org/10.1016/j.cardiores.2007.06.020.
Kolodgie FD, Gold HK, Burke AP, Fowler DR, Kruth HS, Weber DK, et al. Intraplaque hemorrhage and progression of coronary atheroma. N Engl J Med. 2003;349:2316–25. https://doi.org/10.1056/NEJMoa035655.
Moreno PR, Purushothaman KR, Fuster V, Echeverri D, Truszczynska H, Sharma SK, et al. Plaque neovascularization is increased in ruptured atherosclerotic lesions of human aorta: implications for plaque vulnerability. Circulation. 2004;110:2032–8. https://doi.org/10.1161/01.cir.0000143233.87854.23.
Moreno PR, Purushothaman KR, Fuster V, O'Connor WN. Intimomedial interface damage and adventitial inflammation is increased beneath disrupted atherosclerosis in the aorta: implications for plaque vulnerability. Circulation. 2002;105:2504–11.
Mulligan-Kehoe MJ, Simons M. Vasa vasorum in normal and diseased arteries. Circulation. 2014;129:2557–66. https://doi.org/10.1161/CIRCULATIONAHA.113.007189.
Choi BJ, Matsuo Y, Aoki T, Kwon TG, Prasad A, Gulati R, et al. Coronary endothelial dysfunction is associated with inflammation and vasa vasorum proliferation in patients with early atherosclerosis. Arterioscler Thromb Vasc Biol. 2014;34:2473–7. https://doi.org/10.1161/ATVBAHA.114.304445.
ten Kate GL, Sijbrands EJ, Valkema R, ten Cate FJ, Feinstein SB, van der Steen AF, et al. Molecular imaging of inflammation and intraplaque vasa vasorum: a step forward to identification of vulnerable plaques? J Nucl Cardiol. 2010;17:897–912. https://doi.org/10.1007/s12350-010-9263-x.
Burke AP, Farb A, Malcom GT, Liang Y, Smialek JE, Virmani R. PLaque rupture and sudden death related to exertion in men with coronary artery disease. JAMA. 1999;281:921–6. https://doi.org/10.1001/jama.281.10.921.
Fleiner M, Kummer M, Mirlacher M, Sauter G, Cathomas G, Krapf R, et al. Arterial neovascularization and inflammation in vulnerable patients: early and late signs of symptomatic atherosclerosis. Circulation. 2004;110:2843–50. https://doi.org/10.1161/01.cir.0000146787.16297.e8.
Virmani R, Kolodgie FD, Burke AP, Finn AV, Gold HK, Tulenko TN, et al. Atherosclerotic plaque progression and vulnerability to rupture: angiogenesis as a source of intraplaque hemorrhage. Arterioscler Thromb Vasc Biol. 2005;25:2054–61. https://doi.org/10.1161/01.atv.0000178991.71605.18.
Saia F, Komukai K, Capodanno D, Sirbu V, Musumeci G, Boccuzzi G, et al. Eroded versus ruptured plaques at the culprit site of STEMI: in vivo pathophysiological features and response to primary PCI. J Am Coll Cardiol Img. 2015;8:566–75. https://doi.org/10.1016/j.jcmg.2015.01.018.
Arbustini E, Narula N, Kodama T. Clinical imaging of ACS with ruptured or intact fibrous caps. J Am Coll Cardiol Img. 2015;8:576–8. https://doi.org/10.1016/j.jcmg.2015.03.004.
Sugiyama T, Yamamoto E, Bryniarski K, Xing L, Lee H, Isobe M, et al. Nonculprit plaque characteristics in patients with acute coronary syndrome caused by plaque erosion vs plaque rupture: a 3-vessel optical coherence tomography study. JAMA Cardiol. 2018;3:207–14. https://doi.org/10.1001/jamacardio.2017.5234.
Niccoli G, Montone RA, Di Vito L, Gramegna M, Refaat H, Scalone G, et al. Plaque rupture and intact fibrous cap assessed by optical coherence tomography portend different outcomes in patients with acute coronary syndrome. Eur Heart J. 2015;36:1377–84. https://doi.org/10.1093/eurheartj/ehv029.
Hu S, Zhu Y, Zhang Y, Dai J, Li L, Dauerman H, et al. Management and outcome of patients with acute coronary syndrome caused by plaque rupture versus plaque erosion: an intravascular optical coherence tomography study. J Am Heart Assoc. 2017;6. https://doi.org/10.1161/jaha.116.004730.
Yonetsu T, Lee T, Murai T, Suzuki M, Matsumura A, Hashimoto Y, et al. Plaque morphologies and the clinical prognosis of acute coronary syndrome caused by lesions with intact fibrous cap diagnosed by optical coherence tomography. Int J Cardiol. 2016;203:766–74. https://doi.org/10.1016/j.ijcard.2015.11.030.
Witzenbichler B, Maehara A, Weisz G, Neumann FJ, Rinaldi MJ, Metzger DC, et al. Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents: the assessment of dual antiplatelet therapy with drug-eluting stents (ADAPT-DES) study. Circulation. 2014;129:463–70. https://doi.org/10.1161/CIRCULATIONAHA.113.003942.
Jang JS, Song YJ, Kang W, Jin HY, Seo JS, Yang TH, et al. Intravascular ultrasound-guided implantation of drug-eluting stents to improve outcome: a meta-analysis. JACC. Cardiovascular Interventions. 2014;7:233–43. https://doi.org/10.1016/j.jcin.2013.09.013.
Maehara A, Ben-Yehuda O, Ali Z, Wijns W, Bezerra HG, Shite J, et al. Comparison of stent expansion guided by optical coherence tomography versus intravascular ultrasound: the ILUMIEN II study (observational study of optical coherence tomography [OCT] in patients undergoing fractional flow reserve [FFR] and percutaneous coronary intervention). JACC Cardiovascular interventions. 2015;8:1704–14. https://doi.org/10.1016/j.jcin.2015.07.024.
Maehara A, Mintz GS, Witzenbichler B, Weisz G, Neumann FJ, Rinaldi MJ, et al. Relationship between intravascular ultrasound guidance and clinical outcomes after drug-eluting stents. Circ Cardiovasc Interv. 2018;11:e006243. https://doi.org/10.1161/circinterventions.117.006243.
Shameer K, Johnson KW, Glicksberg BS, Dudley JT, Sengupta PP. Machine learning in cardiovascular medicine: are we there yet? Heart. 2018;104:1156–64. https://doi.org/10.1136/heartjnl-2017-311198.
Jordan MI, Mitchell TM. Machine learning: trends, perspectives, and prospects. Science. 2015;349:255–60. https://doi.org/10.1126/science.aaa8415.
Zhang Z, Sejdic E. Radiological images and machine learning: trends, perspectives, and prospects. Comput Biol Med. 2019;108:354–70. https://doi.org/10.1016/j.compbiomed.2019.02.017.
Kawasaki M, Bouma BE, Bressner J, Houser SL, Nadkarni SK, MacNeill BD, et al. Diagnostic accuracy of optical coherence tomography and integrated backscatter intravascular ultrasound images for tissue characterization of human coronary plaques. J Am Coll Cardiol. 2006;48:81–8.
Kawasaki M, Takatsu H, Noda T, Sano K, Ito Y, Hayakawa K, et al. In vivo quantitative tissue characterization of human coronary arterial plaques by use of integrated backscatter intravascular ultrasound and comparison with angioscopic findings. Circulation. 2002;105:2487–92.
Nasu K, Tsuchikane E, Katoh O, Vince DG, Virmani R, Surmely J-F, et al. Accuracy of in vivo coronary plaque morphology assessment: a validation study of in vivo virtual histology compared with in vitro histopathology. J Am Coll Cardiol. 2006;47:2405–12.
Okubo M, Kawasaki M, Ishihara Y, Takeyama U, Kubota T, Yamaki T, et al. Development of integrated backscatter intravascular ultrasound for tissue characterization of coronary plaques. Ultrasound Med Biol. 2008;34:655–63.
Sathyanarayana S, Carlier S, Li W, Thomas L, et al. Characterisation of atherosclerotic plaque by spectral similarity of radiofrequency intravascular ultrasound signals. EuroIntervention : Journal of EuroPCR in Collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2009;5:133–9.
Thim T, Hagensen MK, Wallace-Bradley D, Granada JF, Kaluza GL, Drouet L, et al. Unreliable assessment of necrotic core by VHTM IVUS in porcine coronary artery disease. Circulation: Cardiovascular Imaging. 2010:CIRCIMAGING-109.
Van JH, De GM, Ennekens G, Van PH, Herman A, Vrints C. Validation of in vivo plaque characterisation by virtual histology in a rabbit model of atherosclerosis. EuroIntervention: Journal of EuroPCR in Collaboration with the Working Group on Interventional Cardiology of the European Society of Cardiology. 2009;5:149–56.
Athanasiou LS, Karvelis PS, Tsakanikas VD, Naka KK, Michalis LK, Bourantas CV, et al. A novel semiautomated atherosclerotic plaque characterization method using grayscale intravascular ultrasound images: comparison with virtual histology. IEEE Trans Inf Technol Biomed. 2012;16:391–400.
Brunenberg E, Pujol O, ter Haar Romeny B, Radeva P. Automatic IVUS segmentation of atherosclerotic plaque with stop & go snake,. 2006, pp. 9-16.
Caballero KL, Barajas J, Pujol O, Salvatella N, Radeva P. In-vivo ivus tissue classification: a comparison between rf signal analysis and reconstructed images. 2006, pp. 137-146.
V. G. Giannoglou, D. G. Stavrakoudis, and J. B. Theocharis, "IVUS-based characterization of atherosclerotic plaques using feature selection and SVM classification," 2012, pp. 715-720.
Giannoglou VG, Stavrakoudis DG, Theocharis JB, Petridis V. Genetic fuzzy rule based classification systems for coronary plaque characterization based on intravascular ultrasound images. Eng Appl Artif Intell. 2015;38:203–20.
Hwang YN, Lee JH, Kim GY, Shin ES, Kim SM. Characterization of coronary plaque regions in intravascular ultrasound images using a hybrid ensemble classifier. Comput Methods Prog Biomed. 2018;153:83–92.
Kim GY, Lee JH, Hwang YN, Kim SM. A novel intensity-based multi-level classification approach for coronary plaque characterization in intravascular ultrasound images. Biomed Eng Online, in Press. 2018.
O. Pujol, P. Radeva, J. Vitria, and J. Mauri, "Adaboost to classify plaque appearance in IVUS images," 2004, pp. 629-636.
O. Pujol, D. Rotger, P. Radeva, O. Rodriguez, and J. Mauri, "Near real-time plaque segmentation of IVUS," 2003, pp. 69-72.
Selvathi D, Emimal N, Selvaraj H. Automated characterization of atheromatous plaque in intravascular ultrasound images using neuro fuzzy classifier. International Journal of Electronics and Telecommunications. 2012;58:425–31.
Taki A, Hetterich H, Roodaki A, Setarehdan SK, Unal G, Rieber J, et al. A new approach for improving coronary plaque component analysis based on intravascular ultrasound images. Ultrasound Med Biol. 2010;36:1245–58.
Taki A, Roodaki A, Setarehdan SK, Avansari S, Unal G, Navab N. An IVUS image-based approach for improvement of coronary plaque characterization. Comput Biol Med. 2013;43:268–80.
Vince DG, Dixon KJ, Cothren RM, Cornhill JF. Comparison of texture analysis methods for the characterization of coronary plaques in intravascular ultrasound images. Comput Med Imaging Graph. 2000a;24:221–9.
Zhang X, McKay CR, Sonka M. Tissue characterization in intravascular ultrasound images. IEEE Trans Med Imaging. 1998;17:889–99.
Escalera S, Pujol O, Mauri J, Radeva P. Intravascular ultrasound tissue characterization with sub-class error-correcting output codes. Journal of Signal Processing Systems. 2009;55:35–47.
Granada JF, Wallace-Bradley D, Win HK, Alviar CL, Builes A, Lev EI, et al. In vivo plaque characterization using intravascular ultrasound–virtual histology in a porcine model of complex coronary lesions. Arterioscler Thromb Vasc Biol. 2007;27:387–93.
Brown AJ, Obaid DR, Costopoulos C, Parker RA, Calvert PA, Teng Z, et al. Direct comparison of virtual-histology intravascular ultrasound and optical coherence tomography imaging for identification of thin-cap fibroatheroma clinical perspective. Circulation: Cardiovascular Imaging. 2015;8:e003487.
Maehara A, Mintz GS, Stone GW. OCT versus IVUS: accuracy versus clinical utility. JACC: Cardiovasc Imaging. 2013.
Murray SW, Stables RH, Hart G, Palmer ND. Defining the magnitude of measurement variability in the virtual histology analysis of acute coronary syndrome plaques. European Heart Journal–Cardiovascular Imaging. 2012;14:167–74.
de Korte CL, Sierevogel MJ, Mastik F, Strijder C, Schaar JA, Velema E, et al. Identification of atherosclerotic plaque components with intravascular ultrasound elastography in vivo: a Yucatan pig study. Circulation. 2002;105:1627–30.
Katouzian A, Sathyanarayana S, Baseri B, Konofagou EE, Carlier SG. Challenges in atherosclerotic plaque characterization with intravascular ultrasound (IVUS): from data collection to classification. IEEE Trans Inf Technol Biomed. 2008;12:315–27.
Diethrich EB, Pauliina Margolis M, Reid DB, Burke A, Ramaiah V, Rodriguez-Lopez JA, et al. Virtual histology intravascular ultrasound assessment of carotid artery disease: the carotid artery plaque virtual histology evaluation (CAPITAL) study. Journal of Endovascular Therapy : an Official Journal of the International Society of Endovascular Specialists. 2007;14:676–86. https://doi.org/10.1583/1545-1550(2007)14[676:VHIUAO]2.0.CO;2.
•• Zhang L, Wahle A, Chen Z, Lopez JJ, Kovarnik T, Sonka M. Predicting locations of high-risk plaques in coronary arteries in patients receiving statin therapy. IEEE Transactions on Medical Imaging. 2018;37:151–61. https://doi.org/10.1109/tmi.2017.2725443. Demonstration of combining data from multiple sources to greatly improve risk stratification for coronary artery disease.
Hastie T, Tibshirani R, Friedman J. The elements of statistical learning: data mining, inference, and prediction. 2nd ed. New York: Springer; 2009.
Nair A, Calvetti D, Kuban BD, Vince DG. Novel technique for normalization of intravascular ultrasound backscatter data: improvement in spatial accuracy of tissue maps. Am J Cardiol Suppl S. 2004a;94:123E.
Nair A, Calvetti D, Vince DG. Regularized autoregressive analysis of intravascular ultrasound backscatter: improvement in spatial accuracy of tissue maps. IEEE Trans Ultrason Ferroelectr Freq Control. 2004b;51:420–31. https://doi.org/10.1109/TUFFC.2004.1295427.
Breiman L. Random forests. Mach Learn. 2001;45:5–32. https://doi.org/10.1023/a:1010933404324.
Campos CM, Fedewa RJ, Garcia-Garcia HM, Vince DG, Margolis MP, Lemos PA, et al. Ex vivo validation of 45 MHz intravascular ultrasound backscatter tissue characterization. Eur Heart J Cardiovasc Imaging. 2015;16:1112–9. https://doi.org/10.1093/ehjci/jev039.
Muramatsu T, Garcia-Garcia HM, Brugaletta S, Heo JH, Onuma Y, Fedewa RJ, et al. Reproducibility of intravascular ultrasound radiofrequency data analysis (virtual histology) with a 45-MHz rotational imaging catheter in ex vivo human coronary arteries. J Cardiol. 2015;65:134–42. https://doi.org/10.1016/j.jjcc.2014.05.004.
Moradi M, Abolmaesumi P, Siemens DR, Sauerbrei EE, Boag AH, Mousavi P. Augmenting detection of prostate cancer in transrectal ultrasound images using SVM and RF time series. IEEE Trans Biomed Eng. 2009;56:2214–24. https://doi.org/10.1109/TBME.2008.2009766.
Caixinha M, Amaro J, Santos M, Perdigao F, Gomes M, Santos J. In-vivo automatic nuclear cataract detection and classification in an animal model by ultrasounds. IEEE Trans Biomed Eng. 2016;63:2326–35. https://doi.org/10.1109/TBME.2016.2527787.
Karatzoglou A, Meyer D, Hornik K. Support vector machines in R. J Stat Softw. 2006;15.
Meier DS, Cothren RM, Vince DG, Cornhill JF. Automated morphometry of coronary arteries with digital image analysis of intravascular ultrasound. Am Heart J. 1997;133:681–90.
Kass M, Witkin A, Terzopoulos D. Snakes: active contour models. Int J Comput Vis. 1988;1:321–s. https://doi.org/10.1007/BF00133570.
Mendizabal-Ruiz G, Kakadiaris IA. A physics-based intravascular ultrasound image reconstruction method for lumen segmentation. Comput Biol Med. 2016;75:19–29. https://doi.org/10.1016/j.compbiomed.2016.05.007.
Klingensmith JD, Vince DG. B-spline methods for interactive segmentation and modeling of lumen and vessel surfaces in three-dimensional intravascular ultrasound. Comput Med Imaging Graph. 2002;26:429–38.
Klingensmith VDJD, Nair A, Kuban BD. System and method for identifying a vascular border. USA Patent 8,630,492, January 14, 2014.
Ronneberger O, Fischer P, Brox T. U-Net: convolutional networks for biomedical image segmentation. Lect Notes Comput Sc. 2015;9351:234–41. https://doi.org/10.1007/978-3-319-24574-4_28.
Yang J, Faraji M, Basu A. Robust segmentation of arterial walls in intravascular ultrasound images using Dual Path U-Net. Ultrasonics. 2019;96:24–33. https://doi.org/10.1016/j.ultras.2019.03.014.
Su S, Hu Z, Lin Q, Hau WK, Gao Z, Zhang H. An artificial neural network method for lumen and media-adventitia border detection in IVUS. Comput Med Imaging Graph. 2017;57:29–39. https://doi.org/10.1016/j.compmedimag.2016.11.003.
Qian CJ, Yang XP. An integrated method for atherosclerotic carotid plaque segmentation in ultrasound image. Comput Methods Program Biomed. 2018;153:19–32. https://doi.org/10.1016/j.cmpb.2017.10.002.
Attizzani GF, Bezerra HG. Contemporary assessment of stent strut coverage by OCT. Int J Card Imaging. 2013;29:23–7. https://doi.org/10.1007/s10554-012-0046-0.
Wang A, Eggermont J, Dekker N, Garcia-Garcia HM, Pawar R, Reiber JHC, et al. Automatic stent strut detection in intravascular optical coherence tomographic pullback runs. Int J Card Imaging. 2013;29:29–38. https://doi.org/10.1007/s10554-012-0064-y.
Bruining N, Sihan K, Ligthart J, Winter SD, Regar E. Automated three-dimensional detection of intracoronary stent struts in optical coherence tomography images. 2011 Computing in Cardiology. 2011:221–4.
Gurmeric S, Isguder GG, Carlier S, Unal G. A new 3-D automated computational method to evaluate in-stent neointimal hyperplasia in in-vivo intravascular optical coherence tomography pullbacks. Med Image Comput Comput Assist Interv. 2009;12:776–85. https://doi.org/10.1007/978-3-642-04271-3_94.
Lu H, Gargesha M, Wang Z, Chamie D, Attizzani GF, Kanaya T, et al. Automatic stent detection in intravascular OCT images using bagged decision trees. Biomed Opt Express. 2012;3:2809–24. https://doi.org/10.1364/BOE.3.002809.
Tsantis S, Kagadis GC, Katsanos K, Karnabatidis D, Bourantas G, Nikiforidis GC. Automatic vessel lumen segmentation and stent strut detection in intravascular optical coherence tomography. Med Phys. 2012;39:503–13. https://doi.org/10.1118/1.3673067.
Wang Z, Jenkins MW, Linderman GC, Bezerra HG, Fujino Y, Costa MA, et al. 3-D stent detection in intravascular OCT using a Bayesian network and graph search. IEEE Trans Med Imaging. 2015;34:1549–61. https://doi.org/10.1109/TMI.2015.2405341.
Xu C, Schmitt JM, Akasaka T, Kubo T, Huang K. Automatic detection of stent struts with thick neointimal growth in intravascular optical coherence tomography image sequences. Phys Med Biol. 2011;56:6665–75. https://doi.org/10.1088/0031-9155/56/20/010.
Ughi GJ, Van Dyck CJ, Adriaenssens T, Hoymans VY, Sinnaeve P, Timmermans J-P, et al. Automatic assessment of stent neointimal coverage by intravascular optical coherence tomography. Eur Heart J Cardiovasc Imaging. 2014;15:195–200. https://doi.org/10.1093/ehjci/jet134.
Adriaenssens T, Ughi GJ, Dubois C, Onsea K, De Cock D, Bennett J, et al. Automated detection and quantification of clusters of malapposed and uncovered intracoronary stent struts assessed with optical coherence tomography. Int J Card Imaging. 2014;30:839–48. https://doi.org/10.1007/s10554-014-0406-z.
Nam HS, Kim C-S, Lee JJ, Song JW, Kim JW, Yoo H. Automated detection of vessel lumen and stent struts in intravascular optical coherence tomography to evaluate stent apposition and neointimal coverage. Med Phys. 2016;43:1662–75. https://doi.org/10.1118/1.4943374.
Lu H, Lee J, Ray S, Tanaka K, Bezerra HG, Rollins AM, et al. Automated stent coverage analysis in intravascular OCT (IVOCT) image volumes using a support vector machine and mesh growing. Biomed Opt Express. 2019;10:2809–28. https://doi.org/10.1364/BOE.10.002809.
Phipps JE, Vela D, Hoyt T, Halaney D, Mancuso JJ, Buja LM, et al. Macrophages and intravascular optical coherence tomography bright spots: a quantitative study. JACC Cardiovasc Imaging. 2015;8:63–72. https://doi.org/10.1016/j.jcmg.2014.07.027.
Tearney Guillermo J, Yabushita H, Houser Stuart L, Aretz HT, Jang I-K, Schlendorf Kelly H, et al. Quantification of macrophage content in atherosclerotic plaques by optical coherence tomography. Circulation. 2003;107:113–9. https://doi.org/10.1161/01.CIR.0000044384.41037.43.
Wang Z, Jia H, Tian J, Soeda T, Vergallo R, Minami Y, et al. Computer-aided image analysis algorithm to enhance in vivo diagnosis of plaque erosion by intravascular optical coherence tomography. Circ Cardiovasc Imaging. 2014;7:805–10. https://doi.org/10.1161/CIRCIMAGING.114.002084.
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the international working group for intravascular optical coherence tomography standardization and validation. J Am Coll Cardiol. 2012;59:1058–72. https://doi.org/10.1016/j.jacc.2011.09.079.
van Soest G, Goderie T, Regar E, Koljenović S, van Leenders GLJH, Gonzalo N, et al. Atherosclerotic tissue characterization in vivo by optical coherence tomography attenuation imaging. J Biomed Opt. 2010;15:011105. https://doi.org/10.1117/1.3280271.
Gargesha M, Shalev R, Prabhu D, Tanaka K, Rollins AM, Costa M, et al. Parameter estimation of atherosclerotic tissue optical properties from three-dimensional intravascular optical coherence tomography. J Med Imaging (Bellingham). 2015;2. https://doi.org/10.1117/1.JMI.2.1.016001.
Vermeer KA, Mo J, Weda JJA, Lemij HG, Boer JF d. Depth-resolved model-based reconstruction of attenuation coefficients in optical coherence tomography. Biomed Opt Express. 2014;5:322–37. https://doi.org/10.1364/BOE.5.000322.
Liu S, Sotomi Y, Eggermont J, Nakazawa G, Torii S, Ijichi T, et al. Tissue characterization with depth-resolved attenuation coefficient and backscatter term in intravascular optical coherence tomography images. J Biomed Opt. 2017;22:1–16. https://doi.org/10.1117/1.JBO.22.9.096004.
Athanasiou LS, Exarchos TP, Naka KK, Michalis LK, Prati F, Fotiadis DI. Atherosclerotic plaque characterization in optical coherence tomography images. In 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, 2011, pp. 4485-4488.
Ughi GJ, Adriaenssens T, Sinnaeve P, Desmet W, D’hooge J. Automated tissue characterization of in vivo atherosclerotic plaques by intravascular optical coherence tomography images. Biomed Optics Express. 2013;4:1014–30.
Zhou P, Zhu T, He C, Li Z. Automatic classification of atherosclerotic tissue in intravascular optical coherence tomography images. J Opt Soc Am A Opt Image Sci Vis. 2017;34:1152–9. https://doi.org/10.1364/JOSAA.34.001152.
Rico-Jimenez JJ, Campos-Delgado DU, Villiger M, Otsuka K, Bouma BE, Jo JA. Automatic classification of atherosclerotic plaques imaged with intravascular OCT. Biomed Opt Express. 2016;7:4069–85. https://doi.org/10.1364/BOE.7.004069.
Xu C, Schmitt JM, Carlier SG, Virmani R. Characterization of atherosclerosis plaques by measuring both backscattering and attenuation coefficients in optical coherence tomography. J Biomed Opt. 2008;13:034003.
Abdolmanafi A, Duong L, Dahdah N, Cheriet F. Deep feature learning for automatic tissue classification of coronary artery using optical coherence tomography. Biomed Opt Express. 2017;8:1203–20. https://doi.org/10.1364/BOE.8.001203.
Yong YL, Tan LK, McLaughlin RA, Chee KH, Liew YM. Linear-regression convolutional neural network for fully automated coronary lumen segmentation in intravascular optical coherence tomography. J Biomed Opt. 2017;22:1–9. https://doi.org/10.1117/1.JBO.22.12.126005.
Abdolmanafi A, Duong L, Dahdah N, Adib IR, Cheriet F. Characterization of coronary artery pathological formations from OCT imaging using deep learning. Biomed Opt Express. 2018;9:4936–60. https://doi.org/10.1364/BOE.9.004936.
Krizhevsky A, Sutskever I, Hinton GE. ImageNet classification with deep convolutional neural networks. Commun ACM. 2017;60:84–90. https://doi.org/10.1145/3065386.
He S, Zheng J, Maehara A, Mintz G, Tang D, Anastasio M, et al. Convolutional neural network based automatic plaque characterization from intracoronary optical coherence tomography images. Medical Imaging 2018: Image Processing. 107:2018. https://doi.org/10.1117/12.2293957.
Gessert N, Lutz M, Heyder M, Latus S, Leistner DM, Abdelwahed YS, et al. Automatic plaque detection in IVOCT pullbacks using convolutional neural networks. IEEE Trans Med Imaging. 2019;38:426–34. https://doi.org/10.1109/TMI.2018.2865659.
He K, Zhang X, Ren S, Sun J. Deep residual learning for image recognition. In 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), 2016, pp. 770-778.
Huang G, Liu Z, Maaten LVD, Weinberger KQ. Densely connected convolutional networks. In 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), 2017, pp. 2261-2269.
Prabhu D, Kolluru C, Gharaibeh Y, Mehanna E, Wen D, Wu H, et al. Automated A-line plaque classification of intravascular optical coherence tomography using 3D cryo-image/histology validation. J Biomed Opt. 2019a;24:1–15.
Prabhu D, Bezerra HG, Chaitanya K, Gharaibeh Y, Emile M, Hao W, et al. Automated A-line coronary plaque classification of intravascular OCT images using hand-crafted features and large datasets. J Biomed Optics. 2019b;24(10):106002. https://doi.org/10.1117/1.JBO.24.10.106002.
Lee J, Prabhu D, Kolluru C, Gharaibeh Y, Zimin VN, Bezerra HG, Wilson DL. Automated plaque characterization using deep learning on coronary intravascular optical coherence tomographic images, Biomed Optics Express. 2019;10:6497–6515.
Wang Z, Chamie D, Bezerra HG, Yamamoto H, Kanovsky J, Wilson DL, et al. Volumetric quantification of fibrous caps using intravascular optical coherence tomography. Biomed Optics Express. 2012;3:1413–26. https://doi.org/10.1364/BOE.3.001413.
Wang Z, Kyono H, Bezerra HG, Wang H, Gargesha M, Alraies C, et al. Semiautomatic segmentation and quantification of calcified plaques in intracoronary optical coherence tomography images. J Biomed Opt. 2010;15:061711. https://doi.org/10.1117/1.3506212.
Kolluru C, Prabhu D, Gharaibeh Y, Bezerra H, Guagliumi G, Wilson D. Deep neural networks for A-line-based plaque classification in coronary intravascular optical coherence tomography images. J Med Imaging (Bellingham). 2018;5:044504. https://doi.org/10.1117/1.JMI.5.4.044504.
Gharaibeh Y, Dong P, Prabhu D, Kolluru C, Lee J, Zimin V et al. Deep learning segmentation of coronary calcified plaque from intravascular optical coherence tomography (IVOCT) images with application to finite element modeling of stent deployment. In Medical Imaging 2019: Image-Guided Procedures, Robotic Interventions, and Modeling, 2019, p. 109511C.
Le AS, Aoki H, Murase F, Ishida K. A novel method for classifying driver mental workload under naturalistic conditions with information from near-infrared spectroscopy. Front Hum Neurosci. 2018;12:431–1. https://doi.org/10.3389/fnhum.2018.00431.
Esperança PM, Blagborough AM, Da DF, Dowell FE, Churcher TS. Detection of Plasmodium berghei infected Anopheles stephensi using near-infrared spectroscopy. Parasit Vectors. 2018;11:377–7. https://doi.org/10.1186/s13071-018-2960-z.
Funding
This project was supported by the National Heart, Lung, and Blood Institute through grants R01-HL114406 and R01-HL143484. The content of this report is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rishi Puri, Eitan Fleischman, Juhwan Lee, David Prabhu, David Wilson, and Aaron Fleischman declare that they have no conflict of interest.
Russell Fedewa reports non-financial support from Siemens Medical Solutions USA, Inc., and grants from US Army Medical Research and Material Command CDMRP PRMRP W81XWH-16-1-0608. In addition, Dr. Fedewa has a patent on Advanced ultrasonic detection of different tissue types (WO2019075483A1) pending to Cleveland Clinic.
D. Geoffrey Vince reports grants from Cleveland Clinic (NIH R01 HL64686), and royalty payments from Volcano. In addition, Dr. Vince has a patent issued (6,200,268: Vascular Plaque Characterization. Vince DG, Kuban BD, Nair A. Issued March 13, 2001).
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiac PET, CT, and MRI
Rights and permissions
About this article
Cite this article
Fedewa, R., Puri, R., Fleischman, E. et al. Artificial Intelligence in Intracoronary Imaging. Curr Cardiol Rep 22, 46 (2020). https://doi.org/10.1007/s11886-020-01299-w
Published:
DOI: https://doi.org/10.1007/s11886-020-01299-w