Abstract
In patients with atrial fibrillation (AF), oral anticoagulation is used to prevent stroke and systemic embolism. In a common clinical scenario, AF patients frequently undergo invasive procedures requiring temporary interruption of oral anticoagulation, thereby potentially exposing such patients to increased risk of thromboembolism. Bridging anticoagulation has been used clinically to mitigate this perceived thromboembolic risk, though this practice may also increase risk of periprocedural bleeding. High-quality data has not previously existed to inform decision-making in this clinical situation of bridging anticoagulation. We discuss recent results from the BRIDGE trial and secondary analyses from recent phase 3 randomized clinical trials of direct-acting oral anticoagulant (DOAC) use in non-valvular AF, that inform periprocedural anticoagulation with bridging strategies in AF patients. Updated data from these current trials favor against a strategy of bridging anticoagulation for elective procedures in the majority of AF patients, low or moderate in thromboembolic risk. Bridging anticoagulation is associated with an increased risk of bleeding and no decreased risk of thromboembolism.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Go AS et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245.
Go AS et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001;285(18):2370–5.
Miyasaka Y et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114(2):119–25.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983–8.
American College of Cardiology, F. et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013;127(18):1916–26.
Kovacs MJ et al. Single-arm study of bridging therapy with low-molecular-weight heparin for patients at risk of arterial embolism who require temporary interruption of warfarin. Circulation. 2004;110(12):1658–63.
Spyropoulos AC et al. Clinical outcomes with unfractionated heparin or low-molecular-weight heparin as bridging therapy in patients on long-term oral anticoagulants: the REGIMEN registry. J Thromb Haemost. 2006;4(6):1246–52.
Dunn AS, Spyropoulos AC, Turpie AG. Bridging therapy in patients on long-term oral anticoagulants who require surgery: the Prospective Peri-operative Enoxaparin Cohort Trial (PROSPECT). J Thromb Haemost. 2007;5(11):2211–8.
Douketis JD, Johnson JA, Turpie AG. Low-molecular-weight heparin as bridging anticoagulation during interruption of warfarin: assessment of a standardized periprocedural anticoagulation regimen. Arch Intern Med. 2004;164(12):1319–26.
Garcia DA et al. Risk of thromboembolism with short-term interruption of warfarin therapy. Arch Intern Med. 2008;168(1):63–9.
Wysokinski WE et al. Periprocedural anticoagulation management of patients with nonvalvular atrial fibrillation. Mayo Clin Proc. 2008;83(6):639–45.
Douketis JD et al. Physician preferences for perioperative anticoagulation in patients with a mechanical heart valve who are undergoing elective noncardiac surgery. Chest. 1999;116(5):1240–6.
Schulman S et al. Loading dose vs. maintenance dose of warfarin for reinitiation after invasive procedures: a randomized trial. J Thromb Haemost. 2014;12(8):1254–9.
Ageno W et al. Managing oral anticoagulant therapy in patients with mechanical heart valves undergoing elective surgery: results of a survey conducted among Italian physicians. Blood Coagul Fibrinolysis. 2004;15(8):623–8.
Siegal D et al. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation. 2012;126(13):1630–9.
Garcia DA et al. Perioperative anticoagulation for patients with mechanical heart valves: a survey of current practice. J Thromb Thrombolysis. 2004;18(3):199–203.
Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997;336(21):1506–11.
Katholi RE, Nolan SP, McGuire LB. Living with prosthetic heart valves. Subsequent noncardiac operations and the risk of thromboembolism or hemorrhage. Am Heart J. 1976;92(2):162–7.
Rose AJ, Allen AL, Minichello T, A call to reduce the use of bridging anticoagulation. Circ Cardiovasc Qual Outcomes, 2015.
Douketis JD et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e326S–50. Clinical guidelines from expert review that serve as resource for current recommendations for periprocedural management of anticoagulation.
Douketis JD et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823–33. This randomized control clinical trial is the first such study to prospectively examine in a rigorous fashion to question of whether to use a bridging anticoagulation strategy in certain patients with atrial fibrillation undergoing a procedure.
Steinberg BA et al. Use and outcomes associated with bridging during anticoagulation interruptions in patients with atrial fibrillation: findings from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Circulation. 2015;131(5):488–94. In this “real world study” from a large clinical registry, the lack of efficacy and increased risk is suggested for a periprocedural bridging anticoagulation strategy.
Clark NP et al. Bleeding, recurrent venous thromboembolism, and mortality risks during warfarin interruption for invasive procedures. JAMA Int Med. 2015;175(7):1163–8.
White RH, Ginsberg JS. Low-molecular-weight heparins: are they all the same? Br J Haematol. 2003;121(1):12–20.
Connolly SJ et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51. This open label clinical trial examined the use of the novel oral anticoagulant dabigatran in patients with atrial fibrillation, showing superiority of a 150 mg twice daily dose of dabigatran as compared with warfarin.
Giugliano RP et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Granger CB et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92. This randomized clinical trial showed that apixaban as compared with warfarin patients with atrial fibrillation demonstrated a significant reduction in stroke or systemic embolism with a reduction in major bleeding.
Graham DJ et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2015;131(2):157–64.
Beyer-Westendorf J et al. Peri-interventional management of novel oral anticoagulants in daily care: results from the prospective Dresden NOAC registry. Eur Heart J. 2014;35(28):1888–96.
Healey JS et al. Periprocedural bleeding and thromboembolic events with dabigatran compared with warfarin: results from the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) randomized trial. Circulation. 2012;126(3):343–8. A secondary analysis from the RE-LY examining the use of dabigatran around procedures.
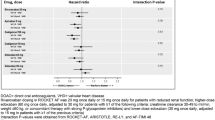
Sherwood MW et al. Outcomes of temporary interruption of rivaroxaban compared with warfarin in patients with nonvalvular atrial fibrillation: results from the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation (ROCKET AF). Circulation. 2014;129(18):1850–9. The outcomes of patients treated with rivaroxaban versus warfarin and who required interruptions of study drug for either complications or procedures were examined in this secondary analysis of the ROCKET AF trial.
Garcia D et al. Management and clinical outcomes in patients treated with apixaban vs warfarin undergoing procedures. Blood. 2014;124(25):3692–8. An analysis from the ARISTOTLE study that even suggested the potential safe continuation of apixaban through certain procedures.
Desai NR et al. Patterns of initiation of oral anticoagulants in patients with atrial fibrillation—quality and cost implications. Am J Med. 2014;127(11):1075–82.e1.
Patel MR et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91. This randomized clinical trial showed non-inferiority of rivaroxaban as compared to warfarin in atrial fibrillation patients with moderate to high risk for thromboembolism.
Connolly SJ et al. The long-term multicenter observational study of dabigatran treatment in patients with atrial fibrillation (RELY-ABLE) study. Circulation. 2013;128(3):237–43.
Douketis JD et al. Perioperative bridging anticoagulation during dabigatran or warfarin interruption among patients who had an elective surgery or procedure. Substudy of the RE-LY trial. Thromb Haemost. 2015;113(3):625–32. Another secondary analysis of the RE-LY trial specifically examining periprocedural bridging strategies in either patients treated with dabigatran or warfarin.
Birnie DH et al. Pacemaker or defibrillator surgery without interruption of anticoagulation. N Engl J Med. 2013;368(22):2084–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Krishnamoorthy reported working on projects funded by research grants at the Duke Clinical Research Institute from the NHLBI, Novartis, Daiichi Sankyo, Eli Lilly, and Maquet and support to attend educational conferences from HeartWare, Thoratec, and Medtronic.
Dr. Ortel reported receiving consulting fees from Instrumentation Laboratory, CSL Behring, and Daiichi-Sankyo and grant support from the Instrumentation Laboratory, the NHLBI, and the Centers for Disease Control and Prevention.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Invasive Electrophysiology and Pacing
Rights and permissions
About this article
Cite this article
Krishnamoorthy, A., Ortel, T. A Bridge to Nowhere? Benefits and Risks for Periprocedural Anticoagulation in Atrial Fibrillation. Curr Cardiol Rep 18, 101 (2016). https://doi.org/10.1007/s11886-016-0779-9
Published:
DOI: https://doi.org/10.1007/s11886-016-0779-9