Abstract
Purpose of Review
Invasive urodynamics are currently used to diagnose disorders of bladder function. However, due to patient discomfort as well as artifacts induced by catheters and non-physiologic filling, less invasive screening tools that can improve diagnostic information, such as ultrasound are required. The purpose of this review is to assess different modalities of ultrasound as applied to functional bladder imaging. This information will help guide future studies in the use of ultrasound during urodynamics.
Recent Findings
Recently, multiple studies have employed ultrasound to evaluate bladder volume, wall thickness, shape, vibrometry, elastography, compliance, biomechanics, and micromotion during urodynamics. These new techniques have used both 2D and 3D ultrasound techniques to evaluate bladder changes during filling. Continued research is needed to confirm ongoing findings prior to widespread incorporation into clinical practice.
Summary
This review demonstrates the potential use of ultrasound as an adjunct to urodynamics for the diagnostic evaluation of functional bladder disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Why Standard Multichannel Urodynamics Are Not Good Enough
Historically, multichannel urodynamics (UDS) has been considered the gold standard for the assessment of lower urinary tract function in individuals with various forms of voiding and storage dysfunction including neurogenic lower urinary tract dysfunction, incomplete emptying, urinary retention, urinary incontinence, and medication-refractory overactive bladder (OAB). Specifically, the purpose of UDS is to determine underlying or contributory causes such as involuntary detrusor contractions, the presence of bladder outlet obstruction, the identification of a poorly contractile detrusor muscle, poor compliance and the finding of detrusor-sphincter dyssynergia.[1] Although UDS is designed to replicate a patient’s typical filling and voiding cycles, the nature of the testing, usually with supra-physiologic filling and the required placement of invasive urethral and rectal/vaginal catheters, can limit the quality and consistency of the results.[2, 3] In addition, patients report embarrassment and even humiliation during UDS, and the test is expensive and associated with complications including pain, bleeding, and urinary tract infections.[4].
Furthermore, UDS results are poorly repeatable and insensitive, particularly in the detection of detrusor overactivity. Our current nomenclature is also problematic, as at present, detrusor overactivity is exclusively a urodynamic condition. Abnormal contractions detected by other means, including ultrasound, therefore require alternative nomenclature, such as involuntary detrusor activity or a reclassification to indicate the detection modality. Gupta and colleagues found poor reproducibility of UDS both between fills during the same study and in repeat visits, likely due to physiological fluctuation in bladder function and inherent lack of sensitivity in testing instruments.[3] There is also the issue of study quality. The International Continence Society (ICS) has published standardization documents regarding appropriate UDS techniques.[1, 19, 20] However, residency training programs, especially in the U.S., provide limited in-depth UDS training (only 10 procedures are required to achieve the required UDS case minimum). The market often drives the type of equipment utilized, and ICS standardization documents are sometimes not reflective of actual practice patterns. For example, most U.S. practices use the air-charged (T-Doc®) urethral catheters. However, the ICS documents do not definitively support this as an acceptable standard.[1, 19].
Finally, development and refinement of current UDS techniques often requires studies involving normal, healthy volunteers as control subjects. Unfortunately, several groups have reported high rates of artifact in these studies and caution against making interpretive comparisons using UDS data from normal, healthy volunteers as control subjects.[21, 22] Although UDS has been considered the gold standard, it simply is not good enough. So, to improve on this relatively low bar, investigators have explored a wide variety of new technologies and refinements.[23] The current review will focus on the use of ultrasound imaging for improved UDS diagnostics. Several areas that will be highlighted include ultrasound as a measure of bladder volume, wall thickness, shape, vibrometry, elastography, compliance, biomechanics, and micromotion (Table 1). Although ultrasound techniques have been employed in other areas of the lower urinary tract including the pelvic floor muscles and urethra, this review will focus specifically on the use of ultrasound in the assessment of bladder function.
Bladder Volume
One of the key benefits of UDS, is that the urodynamicist can precisely control the rate of bladder infusion. Thus, the volume at which a bladder “event,” such as an involuntary contraction occurs, can be clearly identified. The problem with attempts at developing non-invasive (i.e. catheter-free) ultrasound UDS technologies is the lack of ability to control for filling volume. The simplest technique to measure bladder volume non-invasively involves a linear estimate of fill rate.[24] For example, if a patient presents with an empty bladder, confirmed with a bladder scanning device, and voids 360 ml after a 2-h study, we can calculate the average fill rate as 180 ml/hour or 3.0 ml/min. If we assume that the fill rate remains constant, we can estimate volume at any time point during the study. Unfortunately, unless a patient is in a state of maximum diuresis, the fill rate is often quite variable.[24].
Researchers have addressed this issue by creating various natural filling hydration protocols. In one of these studies,[25] participants recorded bladder sensations while being asked to void and drink known amounts of water at prompted intervals (every 10 min) to maintain a constant state of maximum diuresis. Heeringa and colleagues showed that perceived bladder fullness and urgency are significantly related to bladder volume.[26] In a more recent study using ultrasound, researchers employed an oral hydration protocol with healthy participants to create a bladder filling method with consistent and reliable results.[5] Other groups have used hydration protocols, and the National Institutes of Health funded Lower Urinary Tract Dysfunction Research Network (LURN) study published a detailed protocol describing their technique.[27].
In a study by Sheen and colleagues,[5] the investigators acquired volume measurements using a bladder scanning device every five minutes during filling after a period of oral hydration in normal, healthy volunteers. Bladder scanning measurements were used to calculate real-time bladder volumes during two complete fill-void cycles. Volumes were calculated by fitting a second-order polynomial function to the volume data at each 5% capacity increment of the first (slower) fill and using a linear fill estimate for the second (faster) fill.[5] The investigators found that the initial fill after the onset of oral hydration was a ramp-up phase where the fill rate was accelerating, and the average rate was approximately 7 ml/min. However, maximum diuresis of approximately 15 ml/min was achieved and maintained during the second fill which was found to be reproducible over multiple weekly visits. Importantly, this study details an oral hydration natural filling protocol that could be used as a non-invasive method to estimate bladder volumes either with or without the use of bladder scanning or other bladder ultrasound measurements.
To determine which form of ultrasound provides the most accurate estimate of real-time bladder volume, Vinod and colleagues[6] conducted a study comparing two different forms of ultrasound during oral hydration studies: A bladder scanning device and 3D ultrasound. In this study, end-fill ultrasound volume measurements were compared to voided volumes. Both bladder scanner and 3D ultrasound techniques were found to consistently underestimate voided volumes.[6] However, the data were used to create correction factors based on bladder volume for each modality, as many urology and urogynecology practices utilize different types of ultrasound equipment. Similarly, Zhao and colleagues developed bladder volume correction factors based on bladder shape.[7] The combination of both an oral hydration protocol and defined metrics for accurate estimation of real-time bladder volumes during filling opens the door for future non-invasive urodynamic techniques using ultrasound.
Bladder Wall Thickness and Bladder Weight
Assessment of Bladder Outlet Obstruction
The use of ultrasound imaging to quantify bladder wall thickness (BWT) and bladder weight (BW) has been studied as a screening tool to assess various pathologies including the presence of bladder outlet obstruction and detrusor overactivity. Bladder weight is determined by subtracting luminal from total bladder volume. The technique uses ultrasound to measure the luminal and total bladder radius and assumes a spherical bladder shape.[28] BWT is calculated by taking an average of ultrasound-measured anterior bladder wall thickness over at least three different sites.[29, 30] Investigators found that BWT measurements are highly variable during early filling and remain stable after 50% bladder capacity is achieved.[31] A recent metanalysis by Chen and colleagues[32] examined the results of ultrasound BWT and BW from more than 1800 patients in 16 separate studies which compared these ultrasound metrics to the diagnosis of bladder outlet obstruction. They reported an overall BWT sensitivity of 68% and specificity of 91%. For BW, the sensitivity was 88% and the specificity was 81%, suggesting that both BWT and BW may have potential efficacy for the non-invasive diagnosis of bladder outlet obstruction in men exhibiting lower urinary tract symptoms.
Furthermore, the ultrasound measurements of BWT correlate positively with symptoms scores and clinical parameters in patients with benign prostatic hyperplasia.[33] Lastly, BWT has been found to accurately predict responses to medical/surgical treatment of lower urinary tract symptoms resulting from benign prostatic obstruction.[33] However, the lack of standardization and participant diversity among the available studies requires additional larger, prospective studies prior to widespread implementation into clinical practice.
Overall, the ultrasound evaluation of BW and BWT appears to be simple, highly accurate and non-invasive technique to predict bladder outlet obstruction and to evaluate the clinical outcomes after medical/surgical treatments for benign prostatic hyperplasia. The implementation of these techniques and their standardization will hopefully lead to improved diagnostic algorithms for men with lower urinary tract symptoms and could potentially reduce the requirement for pressure flow-studies.
Assessment of Detrusor Overactivity
Another application of BWT is the non-invasive identification of detrusor overactivity. In one study,[29] investigators assessed whether BWT measured through ultrasound could replace other screening tools as a noninvasive test for detrusor overactivity. In the study, women underwent both invasive transvaginal ultrasound and urodynamic studies to determine which had a higher detection rate. Transvaginal ultrasound showed a low sensitivity (43%) in women with OAB, indicating limited utility of this technique in this context.[29].
Assessment of Detrusor Underactivity
Studies have shown that ultrasound might be feasible in the diagnosis of detrusor underactivity. One study involving 33 patients compared BWT with possible filling volume[34] and showed an 87% accuracy in detecting detrusor underactivity. Indeed, all men in the study with a bladder capacity greater than 445 mL and BWT less than 1.23 mm were found to have detrusor underactivity.[34] Building on this work, another group used suprapubic ultrasound to measure BWT and created a nomogram to improve future clinical accuracy.[9] Ultrasound in conjunction with linear regression identified a significant difference in BWT between those with detrusor underactivity and control patients demonstrating a possible clinical benefit when assessing individuals affected by this disorder.[9].
Bladder Shape
Why shape matters
According to the Law of Laplace, the wall tension (T) in the bladder is related to the radius (R) of the organ multiplied by the internal fluid pressure (P): T ∝ PR. Therefore, any deviation from a bladder's unconstrained shape would create regions of increased wall tension during filling and could lead to heightened sensation. Picture a balloon (Fig. 1). When the balloon is inflated, it has a wide body with high wall tension and a narrow tail with low wall tension. Therefore, in biomechanical terms, shape matters.[35, 36] This is somewhat intuitive; for example, a woman in late-stage pregnancy or with large fibroids may have a pancake-shaped or distorted bladder due to compression. A child with severe constipation will often present with urinary frequency and urgency. A patient with prior pelvic surgery and adhesive bowel disease may have constrained bladder filling, forcing the bladder to assume an irregular shape. Again, shape matters.
In a partially inflated balloon (A, B), pressure (p) is constant throughout (p1 = p2). However, due to differences in shape, wall tension varies (t1 < t2). This balloon analogy demonstrates how wall tension can vary based on bladder location. Because many bladders have irregular shapes as shown in C, D, E. Therefore, bladder shape matters, but 3D shape can't be assessed using UDS (but can be assessed with ultrasound imaging)
Furthermore, tension-sensitive afferent nerves in the bladder[37] likely contribute to the sensation of bladder filling which can subsequently lead to urgency. Acute or chronic changes in a bladder’s material properties (elasticity) or geometry (volume and shape) may also affect bladder wall tension, and therefore, the activation of nerves responsible for bladder sensation. Several imaging techniques, including magnetic resonance imaging and computed tomography, have been used to examine bladder shape.[38] Normal bladders vary in shape,[11, 12, 39] and bladder compliance is related to shape.[35, 36] Because a clinical urodynamic study measures pressures, but not shape, variations in bladder shape and the corresponding localized variations in wall tension and tension sensor output cannot currently be evaluated. Nagle et al.[17] demonstrated how ultrasound urodynamics can be used to measure biomechanical parameters during filling, including strain, tension, stress, and elastic modulus of the bladder wall.
As shown in Fig. 2, bladder filling that is constrained by external forces, as seen acutely in the setting of positional changes during cystometrics,[40] and chronically, in the setting of pregnancy,[41] obesity,[42] or constipation,[43] can increase the load on tension-sensing nerves and lead to a reduced micturition threshold volume.
In this illustration, a spherical bladder reaches its micturition threshold at 400 mL with an equatorial wall strip length equal to 1/2 the circumference, or 14.4 cm (red strip, point A). If the bladder is contrained by 25% in one radial direction to form an oblate sphere (arrows), it reaches the same threshold strip length (14.4 cm) and therfore approximately the same tension sensor load at a dramatically lower volume of \(\backsim\) 300 mL (orange strip, point B)
How to measure bladder shape
Accepting that bladder shape may be an important driver of bladder sensation and contractility and may relate to disorders of urinary urgency, a clear research and clinical objective for urodynamics is the development of tools that can accurately determine aspects of bladder shape. Ultrasound can be used for this purpose. In a comparative-fill urodynamic study, ultrasound was used to determine changes in volume for participants with OAB.[8] During analysis, there were three different image calculations used: 3D volume, 2D spheroid geometry, and 2D spheroid geometry with a correction factor.[44] 3D bladder ultrasound was found to be the most precise.[8] During continuous filling, 3D ultrasound was more likely to recognize abnormally shaped bladders than either of the 2D counterparts.[8] This showed that 3D bladder ultrasound would offer the best imaging modality moving forward for detecting and measuring irregularities and changes in bladder shape.
Bladder Shape as a Diagnostic Tool
Although the bladder has often been modeled as a sphere or spheroid,[35, 36, 45] imaging has revealed that bladder shape is highly variable and asymmetrical. Studies have demonstrated banana-like shapes in people with pelvic lipomatosis[46] and that bladder shape changes during filling which, as a consequence, can alter its function.[47] Multiple studies have evaluated bladder shape as a potential diagnostic tool for OAB. In a study performed during urodynamics and natural filling, the investigators used ultrasound to determine bladder shape differences between asymptomatic patients and OAB patients.[10] They identified changes in bladder shape associated with detrusor muscle contraction, showing an increase incidence of ellipsoid shapes in participants with OAB. This was found mainly in the transverse plane. In contrast, a prospective study using 3D ultrasound showed that bladder shape irregularities were most consistently identified in the sagittal plane, and that these irregularities were also associated with OAB.[12].
In another study of women with and without OAB, transabdominal 3D ultrasound was used to determine height-to-width ratios of the bladder in multiple planes as a measure of shape.[11] Ratios were compared at low (20% capacity) and high volumes (100% capacity) to calculate strain. In both groups, change in height during filling was more pronounced than changes in other planes, indicating that bladder filling is not spherical but mainly occurs in the vertical (craniocaudal) plane. However, the key difference was that OAB patients were more likely to have non-spherical bladder shapes than controls. This study suggested that irregular bladder shapes may be a causative mechanism of OAB and that a shape-mediated OAB phenotype could be identified, non-invasively, using ultrasound during bladder filling. Future clinical tests using ultrasound will require an automated method for shape and volume measurement that is both reliable and reproducible, given that most aspects of bladder shape change as the bladder fills.
Bladder Vibrometry and Elastography
Vibrometry
As an alternative approach to urodynamics, investigators have used ultrasound with Lamb wave pulsation to determine the flexibility and movement of bladder wall tissues.[13, 48] With this technique, the ultrasound device emits a wavelike pulsation to move bladder wall tissue, and this movement is used to determine tissue properties including elasticity.[13] To calculate elasticity, assumptions were required to estimate bladder wall thickness and bladder curvature. In subsequent studies[14] bladder vibrometry was used as tool to identify detrusor overactivity in individuals with neurogenic bladder dysfunction. This study created a detrusor overactivity index which correlated vibrometry measurements with urodynamically identified detrusor overactivity, demonstrating the potentially feasibility of this technique as a non-invasive alternative to UDS.
Elastography
Elastography uses ultrasound shear waves to measure tissue stiffness based on the response to applied stress. This novel technique has been used to measure increased bladder wall fibrosis (increased thickness) associated with detrusor overactivity.[15] The authors of this study propose that the bladder becomes less compliant due to increased detrusor activity. As a result, increased shear wave stress is needed to cause movement in the anterior bladder wall.[15] The investigators showed a strong positive correlation between both measured anterior and posterior bladder wall shear wave stress and pressure, showing proof of principle that ultrasound elastography could potentially be used as a non-invasive measure of detrusor overactivity. Another more recent study used ultrasound elastography of the bladder in the assessment of patients with known neurogenic bladder dysfunction.[49] Using urodynamic metrics of detrusor overactivity and poor compliance as markers of neurogenic bladder dysfunction, the authors found that shear wave velocity was increased in approximately 80% of patients with neurogenic bladder. They conclude that bladder elastography has high specificity for identification of UDS parameters associated with neurogenic bladder dysfunction.
Bladder Compliance and Biomechanics
Compliance
A recent study completed by Zhang and colleagues[16] used ultrasound bladder vibrometry to measure bladder wall compliance. In this urodynamic study, Lambda wave speed correlated with both intravascular and detrusor pressure. Furthermore, a compliance index, created using Lambda wave speed and filling volume, was comparable to standardized UDS compliance measurements (change in volume over change in pressure). Bladders were considered non-compliant with a vibrometry index of less than 100 mL·s2·m−2. The resulting sensitivity (86.4%) and specificity (71.9%) demonstrated acceptable accuracy as an alternative, and non-invasive, measurement of detrusor compliance.
Bladder Biomechanics
In a study conducted by Nagle and colleagues,[17] the investigators performed ultrasound in conjunction with UDS to determine bladder biomechanical parameters including pressure, volume, strain, tension, and stress. While many of these measurements required direct measurements of intravesical pressure, perimeter strain (change in perimeter over change in volume) only required ultrasound imaging and represents a possible assessment tool for OAB. In conjunction with UDS, the authors propose that ultrasound could be used as a future tool to identify different subtypes of OAB.
Bladder Compression and Provoked Compliance
Dynamic elasticity describes a material property of the bladder wall whereby wall tension, and therefore sensation, can be acutely lowered by passive filling/emptying and restored by contractile activity.[50, 51] In fact, dynamic elasticity has been identified using comparative-fill UDS.[51, 52] The challenge is that comparative-fill UDS are difficult, invasive and time-consuming. To address this issue, bladder compression has been studied in an isolated porcine bladder model and has been shown to acutely alter dynamic elasticity.[53, 54] Consequently, abdominal compression with an ultrasound probe provides a novel method to acutely alter bladder shape (increase strain) and an imaging modality that can be used to quantify the degree of strain. When combined with UDS, changes in bladder shape due to compression divided by changes in pressure have been used to define a new provoked compliance metric.[55] Ultimately, provoked compliance may represent a useful alternative to standard measures of bladder compliance.
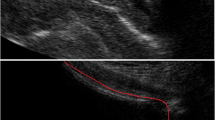
Bladder Wall Micromotion
In a study by Nagle and colleagues, M-mode ultrasound of the anterior bladder wall was used to identify both the outer and luminal edges prior to micromotion calculation.(18) Micromotion was defined as greater than 0.1 mm change in wall thickness after controlling for macro-movements such as breathing. The results demonstrated that approximately 40% of OAB women were found to have ultrasound-identified micromotion, but no asymptomatic women were found to have micromotion. In addition, micromotion correlated strongly with the presence of involuntary detrusor contractions, indicating that this technique has potential utility as a non-invasive detector of micromotion.
Conclusion
Ultrasound is a promising tool that has the potential to supplement or even replace invasive UDS in the future. Multiple ultrasound UDS research studies have been conducted. Nevertheless, the results have mainly been limited in scale and, as yet, there has not been widespread clinical adoption of any new techniques. Research is ongoing regarding which bladder parameters will ultimately prove useful as reliable, reproducible and discriminatory markers for functional bladder pathology. Currently, bladder wall thickness, shape, vibrometry, elastography, compliance, biomechanics, and micromotion are being investigated as novel ultrasound UDS techniques. Continued research with larger, comparative multi-institutional studies will be required before ultrasound UDS becomes accepted as a diagnostic tool in the assessment, management and understanding of functional bladder disorders.
Data Availability
No datasets were generated or analysed during the current study.
References
Rosier P, Schaefer W, Lose G, Goldman HB, Guralnick M, Eustice S, Dickinson T, Hashim H. International continence society good urodynamic practices and terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn. 2017;36(5):1243–60.
Erdem E, Akbay E, Doruk E, Cayan S, Acar D, Ulusoy E. How reliable are bladder perceptions during cystometry? Neurourol Urodyn. 2004;23(4):306–10.
Gupta A, Defreitas G, Lemack GE. The reproducibility of urodynamic findings in healthy female volunteers: results of repeated studies in the same setting and after short-term follow-up. Neurourol Urodyn. 2004;23(4):311–6.
Abelson B, Majerus S, Sun D, Gill BC, Versi E, Damaser MS. Ambulatory urodynamic monitoring: state of the art and future directions. Nat Rev Urol. 2019;16(5):291–301.
Sheen D, Kolli H, Nagle AS, Cullingsworth Z, Vinod NN, Naimi HA, De Wachter SG, Mazzeo SE, Stothers L, Speich JE, Klausner AP. Validation of a real-time bladder sensation meter during oral hydration in healthy adults: repeatability and effects of fill rate and ultrasound probe pressure. Low Urin Tract Symptoms. 2019;11(4):224–31.
Vinod NN, Nagle AS, Naimi HA, Kolli H, Sheen D, Nandanan N, Carucci LR, Speich JE, Klausner AP. Bladder volume correction factors measured with 3D ultrasound and BladderScan. Can J Urol. 2019;26(4):9829–34.
Zhao L, Liao L, Gao L, Gao Y, Chen G, Cong H, Wang Y, Liao X. Effects of bladder shape on accuracy of measurement of bladder volume using portable ultrasound scanner and development of correction method. Neurourol Urodyn. 2019;38(2):653–9.
Nagle AS, Bernardo RJ, Varghese J, Carucci LR, Klausner AP, Speich JE. Comparison of 2D and 3D ultrasound methods to measure serial bladder volumes during filling: Steps toward development of non-invasive ultrasound urodynamics. Bladder (San Franc). 2018;5(1).
De Nunzio C, Lombardo R, Cicione A, Trucchi A, Carter S, Tema G, Nacchia A, Vicentini C, Tubaro A. The role of bladder wall thickness in the evaluation of detrusor underactivity: Development of a clinical nomogram. Neurourol Urodyn. 2020;39(4):1115–23.
Gray T, Phillips L, Li W, Buchanan C, Campbell P, Farkas A, Abdi S, Radley S. Evaluation of bladder shape using transabdominal ultrasound: Feasibility of a novel approach for the detection of involuntary detrusor contractions. Ultrasound. 2019;27(3):167–75.
Glass Clark S, Nagle AS, Bernardo R, Vinod N, Carucci L, Carroll A, Speich J, Klausner AP. Use of ultrasound urodynamics to identify differences in bladder shape between individuals with and without overactive bladder. Female Pelvic Med Reconstr Surg. 2020;26(10):635–9.
Li R, Nagle AS, Maddra KM, Vinod N, Prince SA, Tensen SI, Thapa D, Sebastian B, Sethi D, Alattar A, Carucci LR, Klausner AP, Speich JE. Irregular bladder shapes identified in women with overactive bladder: an ultrasound nomogram. Am J Clin Exp Urol. 2021;9(5):367–77.
Nenadic I, Mehrmohammadi M, Urban MW, Alizad A, Greenleaf JF, Fatemi M. In vivo patient measurements of bladder elasticity using Ultrasound Bladder Vibrometry (UBV). Conf Proc IEEE Eng Med Biol Soc. 2013;2013:113–6.
Rosen DP, Husmann DA, Mynderse LA, Kelly TF Jr, Alizad A, Fatemi M. Detrusor overactivity assessment using ultrasound bladder vibrometry. Physiol Meas. 2021;42(10)
Sturm RM, Yerkes EB, Nicholas JL, Snow-Lisy D, Diaz Saldano D, Gandor PL, Halline CG, Rosoklija I, Rychlik K, Johnson EK, Cheng EY. Ultrasound shear wave elastography: a novel method to evaluate bladder pressure. J Urol. 2017;198(2):422–9.
Zhang X, Husmann DA, Mynderse LA, Alizad A, Fatemi M. Non-invasive assessment of urinary bladder compliance using ultrasound: first validation study based on clinical urodynamic study. Ann Transl Med. 2021;9(7):547.
Nagle AS, Klausner AP, Varghese J, Bernardo RJ, Colhoun AF, Barbee RW, Carucci LR, Speich JE. Quantification of bladder wall biomechanics during urodynamics: A methodologic investigation using ultrasound. J Biomech. 2017;61:232–41.
Nagle AS, Cullingsworth ZE, Li R, Carucci LR, Klausner AP, Speich JE. Bladder wall micromotion measured by non-invasive ultrasound: initial results in women with and without overactive bladder. Am J Clin Exp Urol. 2021;9(1):44–52.
Rosier P, Gammie A, Valdevenito JP, Speich J, Smith P, Sinha S, members of the ICSWGPFS. ICS-SUFU standard: Theory, terms, and recommendations for pressure-flow studies performance, analysis, and reporting. Part 2: analysis of PFS, reporting, and diagnosis. Neurourol Urodyn. 2023;42(8):1603–27.
Rosier P, Valdevenito JP, Smith P, Sinha S, Speich J, Gammie A, Members of the ICSWGPFS. ICS-SUFU standard: Theory, terms, and recommendations for pressure-flow studies performance, analysis, and reporting. Part 1: background theory and practice. Neurourol Urodyn. 2023;42(8):1590–602.
Swavely NR, Speich JE, Klausner AP. Artifacts and abnormal findings may limit the use of asymptomatic volunteers as controls for studies of multichannel urodynamics. Minerva Urologica e Nefrologica = The Italian Journal of Urology and Nephrology. 2021;73(5):655–61.
Leitner L, Walter M, Sammer U, Knupfer SC, Mehnert U, Kessler TM. Urodynamic investigation: a valid tool to define normal lower urinary tract function? PLoS One. 2016;11(10):e0163847.
Gammie A, Speich JE, Damaser MS, Gajewski JB, Abrams P, Rosier P, Arlandis S, Tarcan T, Finazzi Agro E. What developments are needed to achieve less-invasive urodynamics? ICI-RS 2019. Neurourol Urodyn. 2020;39 Suppl 3(n/a):S36–S42.
Medina Lucena H, Tincello DG. Validation of a water-load protocol to define the pattern of bladder sensation. Int Urogynecol J. 2019;30(5):767–72.
De Wachter SG, Heeringa R, Van Koeveringe GA, Winkens B, Van Kerrebroeck PE, Gillespie JI. "Focused introspection" during naturally increased diuresis: description and repeatability of a method to study bladder sensation non-invasively. Neurourol Urodyn. 2014;33(5):502–6.
Heeringa R, van Koeveringe GA, Winkens B, van Kerrebroeck PE, de Wachter SG. Degree of urge, perception of bladder fullness and bladder volume--how are they related? J Urol. 2011;186(4):1352–7.
Lai HH, Naliboff B, Liu AB, Amundsen CL, Shimony JS, Magnotta VA, Shaffer JJ, Gilliam RL, Wiseman JB, Helmuth ME, Andreev VP, Kirkali Z, Harte SE, Group LS. The LURN research network neuroimaging and sensory testing (NIST) study: design, protocols, and operations. Contemp Clin Trials. 2018;74:76–87.
Kojima M, Inui E, Ochiai A, Naya Y, Ukimura O, Watanabe H. Noninvasive quantitative estimation of infravesical obstruction using ultrasonic measurement of bladder weight. J Urol. 1997;157(2):476–9.
Latthe P, Middleton L, Rachaneni S, McCooty S, Daniels J, Coomarasamy A, Balogun M, Duckett J, Thakar R, Goranitis I, Roberts T, Deeks J, Group BUSC. Ultrasound bladder wall thickness and detrusor overactivity: a multicentre test accuracy study. BJOG. 2017;124(9):1422–9.
Rachaneni S, McCooty S, Middleton LJ, Parker VL, Daniels JP, Coomarasamy A, Verghese TS, Balogun M, Goranitis I, Barton P, Roberts TE, Deeks JJ, Latthe P, Bladder Ultrasound Study Collaborative G. Bladder ultrasonography for diagnosing detrusor overactivity: test accuracy study and economic evaluation. Health Technol Assess. 2016;20(7):1–150.
Oelke M, Hofner K, Jonas U, Ubbink D, de la Rosette J, Wijkstra H. Ultrasound measurement of detrusor wall thickness in healthy adults. Neurourol Urodyn. 2006;25(4):308–18.
Chen YZ, Peng L, Zhang C, Xu S, Luo DY. Bladder sonomorphological tests in diagnosing bladder outlet obstruction in patients with lower urinary tract symptoms: a systematic review and meta-analysis. Urol Int. 2023;107(4):327–35.
Presicce F, DEN C, Gacci M, Finazzi Agro E, Tubaro A. Non-invasive ultrasound measurements in male patients with LUTS and benign prostatic obstruction: implication for diagnosis and treatment. Minerva Urol Nefrol. 2017;69(3):220–33.
Rademakers KL, van Koeveringe GA, Oelke M, Force Research Group, Maastricht and Hannover. Ultrasound detrusor wall thickness measurement in combination with bladder capacity can safely detect detrusor underactivity in adult men. World J Urol. 2017;35(1):153–9.
Damaser MS, Lehman SL. Does it matter, the shape of the bladder? Neurourol Urodyn. 1993;12(3):277–80.
Damaser MS, Lehman SL. The effect of urinary bladder shape on its mechanics during filling. J Biomech. 1995;28(6):725–32.
Kanai A, Andersson KE. Bladder afferent signaling: recent findings. J Urol. 2010;183(4):1288–95.
Hiorns MP. Imaging of the urinary tract: the role of CT and MRI. Pediatr Nephrol. 2011;26(1):59–68.
Maddra KM, Li R, Nagle AS, Klausner AP, Speich JE. Repeatability of ultrasound-defined bladder shape metrics in healthy volunteers. Res Rep Urol. 2022;14:185–92.
Uluocak N, Oktar T, Acar O, Incesu O, Ziylan O, Erkorkmaz U. Positional changes in voiding dynamics of children with non-neurogenic bladder dysfunction. Urology. 2008;72(3):530–5.
van Brummen HJ, Bruinse HW, van de Pol G, Heintz AP, van der Vaart CH. Bothersome lower urinary tract symptoms 1 year after first delivery: prevalence and the effect of childbirth. BJU Int. 2006;98(1):89–95.
Chancellor MB, Oefelein MG, Vasavada S. Obesity is associated with a more severe overactive bladder disease state that is effectively treated with once-daily administration of trospium chloride extended release. Neurourol Urodyn. 2010;29(4):551–4.
Kim JH, Lee JH, Jung AY, Lee JW. The prevalence and therapeutic effect of constipation in pediatric overactive bladder. Int Neurourol J. 2011;15(4):206–10.
Bih LI, Ho CC, Tsai SJ, Lai YC, Chow W. Bladder shape impact on the accuracy of ultrasonic estimation of bladder volume. Arch Phys Med Rehabil. 1998;79(12):1553–6.
Habteyes FG, Komari SO, Nagle AS, Klausner AP, Heise RL, Ratz PH, Speich JE. Modeling the influence of acute changes in bladder elasticity on pressure and wall tension during filling. J Mech Behav Biomed Mater. 2017;71:192–200.
Zhang Y, Wu S, Xi Z, Wang X, Jiang X. Measuring diagnostic accuracy of imaging parameters in pelvic lipomatosis. Eur J Radiol. 2012;81(11):3107–14.
Lotz HT, van Herk M, Betgen A, Pos F, Lebesque JV, Remeijer P. Reproducibility of the bladder shape and bladder shape changes during filling. Med Phys. 2005;32(8):2590–7.
Nenadic IZ, Qiang B, Urban MW, de Araujo Vasconcelo LH, Nabavizadeh A, Alizad A, Greenleaf JF, Fatemi M. Ultrasound bladder vibrometry method for measuring viscoelasticity of the bladder wall. Phys Med Biol. 2013;58(8):2675–95.
Sarkarian M, Arjomandi A, Musapour I, Hanafi MQ. Can bladder shear wave elastography be an alternative method for detection of neurogenic bladder instead of urodynamic study? J Family Med Prim Care. 2020;9(2):921–4.
Colhoun AF, Speich JE, Dolat MT, Habibi JR, Guruli G, Ratz PH, Barbee RW, Klausner AP. Acute length adaptation and adjustable preload in the human detrusor. Neurourol Urodyn. 2016;35(7):792–7.
Colhoun AF, Klausner AP, Nagle AS, Carroll AW, Barbee RW, Ratz PH, Speich JE. A pilot study to measure dynamic elasticity of the bladder during urodynamics. Neurourol Urodyn. 2017;36(4):1086–90.
Cullingsworth ZE, Klausner AP, Li R, Nagle AS, Carroll AW, Roseman JT 2nd, Speich JE. Comparative-fill urodynamics in individuals with and without detrusor overactivity supports a conceptual model for dynamic elasticity regulation. Neurourol Urodyn. 2020;39(2):707–14.
Duval DLM, Weprin S, Nandanan N, Cullingsworth ZE, Swavely NR, Balthazar A, Mangino MJ, Speich JE, Klausner AP. Regulation of bladder dynamic elasticity: a novel method to increase bladder capacity and reduce pressure using pulsatile external compressive exercises in a porcine model. Int Urol Nephrol. 2021;53(9):1819–25.
Balthazar A, Cullingsworth ZE, Nandanan N, Anele U, Swavely NR, Speich JE, Klausner AP. An external compress-release protocol induces dynamic elasticity in the porcine bladder: A novel technique for the treatment of overactive bladder? Neurourol Urodyn. 2019;38(5):1222–8.
Smolen J, Keshishian C, Vossenberg AJ, Kodama S, Khandpur R, Dunlap J, Alattar A, Pummill I, Grob G, Ghatas MP, Burkett LS, Siff LN, Klausner AP, Speich JE. A novel method for deriving bladder provoked compliance from abdominal compressions during ultrasound urodynamics. J Eurol. 2023;209(Supplement 4):e30.
Funding
Dr. Speich and Dr. Klausner received funding from NIH grant R01DK101719.
Author information
Authors and Affiliations
Contributions
B.M. and H.H. wrote the main manuscript text. B.M. and J.S prepared figures. J.S. S.R., L.B. and A.K. edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
Dr. Adam P Klausner and Dr. John E Speich report ownership interest in Vesi Corporation.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Dr. Adam P Klausner and Dr. John E Speich report ownership interest in Vesi Corporation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McCormack, B., Hampton, H.L., Speich, J.E. et al. Ultrasound Urodynamics: A Review of Ultrasound Imaging Techniques for Enhanced Bladder Functional Diagnostics. Curr Bladder Dysfunct Rep (2024). https://doi.org/10.1007/s11884-024-00758-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s11884-024-00758-2