Abstract
Purpose of Review
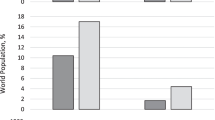
Sex and gender differences exist with regard to the association between depression and cardiovascular disease (CVD). This narrative review describes the prevalence, mechanisms of action, and management of depression and CVD among women, with a particular focus on coronary heart disease (CHD).
Recent Findings
Women versus men with incident and established CHD have a greater prevalence of depression. Comorbid depression and CHD in women may be associated with greater mortality, and treatment inertia. Proposed mechanisms unique to the association among women of depression and CHD include psychosocial, cardiometabolic, behavioral, inflammatory, hormonal, and autonomic factors.
Summary
The literature supports a stronger association between CHD and the prevalence of depression in women compared to men. It remains unclear whether depression treatment influences cardiovascular outcomes, or if treatment effects differ by sex and/or gender. Further research is needed to establish underlying mechanisms as diagnostic and therapeutic targets.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143(8):e254–743.
Cho L, Davis M, Elgendy I, Epps K, Lindley KJ, Mehta PK, et al. Summary of updated recommendations for primary prevention of cardiovascular disease in women: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(20):2602–18.
Brody DJ, Pratt LA, Hughes JP. Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief, no 303. Hyattsville, MD. 2018.
Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull. 2017;143(8):783–822.
•• Vaccarino V, Badimon L, Bremner JD, Cenko E, Cubedo J, Dorobantu M, et al. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur Heart J. 2020;41(17):1687–96. Review of the key aspects of current evidence regarding the association between depression and coronary heart disease, including epidemiological, mechanistic, and management considerations.
Wium-Andersen MK, Wium-Andersen IK, Prescott EIB, Overvad K, Jorgensen MB, Osler M. An attempt to explain the bidirectional association between ischaemic heart disease, stroke and depression: a cohort and meta-analytic approach. Br J Psychiatry. 2020;217(2):434–41.
Nielsen RE, Banner J, Jensen SE. Cardiovascular disease in patients with severe mental illness. Nat Rev Cardiol. 2021;18(2):136–45.
Mehta LS. Cardiovascular disease and depression in women. Heart Fail Clin. 2011;7(1):39–45.
•• Bucciarelli V, Caterino AL, Bianco F, Caputi CG, Salerni S, Sciomer S, et al. Depression and cardiovascular disease: the deep blue sea of women’s heart. Trends Cardiovasc Med. 2020;30(3):170–6. Review of the prevalence, morbidity and mortality, pathophysiology, and mechanistic differences of CVD among women, highlighting sex/gender differences.
Jiang X, Asmaro R, O’Sullivan DM, Modi J, Budnik E, Schnatz PF. Depression may be a risk factor for coronary heart disease in midlife women <65years: a 9-year prospective cohort study. Int J Cardiol. 2018;271:8–12.
Parkin L, Balkwill A, Green J, Reeves GK, Beral V, Floud S, et al. Depression, anxiety, psychotropic drugs, and acute myocardial infarction: large prospective study of United Kingdom women. Psychol Med. 2021:1–7.
Smaardijk VR, Lodder P, Kop WJ, van Gennep B, Maas A, Mommersteeg PMC. Sex- and gender-stratified risks of psychological factors for incident ischemic heart disease: systematic review and meta-analysis. J Am Heart Assoc. 2019;8(9):e010859.
Kouvari M, Panagiotakos DB, Chrysohoou C, Notara V, Georgousopoulou E, Tousoulis D, et al. Sex-discrete role of depressive symptomatology on 10-year first and recurrent cardiovascular disease incidence: results from ATTICA and GREECS prospective studies. Hellenic J Cardiol. 2020;61(5):321–8.
Zhang XE, Cheng B, Wang Q, Wan JJ. Association of gender-specific risk factors in metabolic and cardiovascular diseases: an NHANES-based cross-sectional study. J Investig Med. 2018;66(1):22–31.
Jackson CA, Kerssens J, Fleetwood K, Smith DJ, Mercer SW, Wild SH. Incidence of ischaemic heart disease and stroke among people with psychiatric disorders: retrospective cohort study. Br J Psychiatry. 2020;217(2):442–9.
Matetic A, Shamkhani W, Rashid M, Volgman AS, Van Spall HGC, Coutinho T, et al. Trends of sex differences in clinical outcomes after myocardial infarction in the United States. CJC Open. 2021;3(12 Suppl):S19–27.
Bandyopadhyay D, Chakraborty S, Amgai B, Patel N, Hajra A, Heise L, et al. Acute myocardial infarction in the young—National Trend Analysis with gender-based difference in outcomes. Int J Cardiol. 2020;301:21–8.
Serpytis P, Navickas P, Lukaviciute L, Navickas A, Aranauskas R, Serpytis R, et al. Gender-based differences in anxiety and depression following acute myocardial infarction. Arq Bras Cardiol. 2018;111(5):676–83.
Saelee R, Vaccarino V, Sullivan S, Hammadah M, Shah A, Wilmot K, et al. Longitudinal associations between self-reported experiences of discrimination and depressive symptoms in young women and men post-myocardial infarction. J Psychosom Res. 2019;124:109782.
AbuRuz ME, Al-Dweik G. Depressive symptoms and complications early after acute myocardial infarction: gender differences. Open Nurs J. 2018;12:205–14.
Pogosova N, Kotseva K, De Bacquer D, von Kanel R, De Smedt D, Bruthans J, et al. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur J Prev Cardiol. 2017;24(13):1371–80.
Guimaraes PO, Granger CB, Stebbins A, Chiswell K, Held C, Hochman JS, et al. Sex differences in clinical characteristics, psychosocial factors, and outcomes among patients with stable coronary heart disease: insights from the STABILITY (stabilization of atherosclerotic plaque by initiation of darapladib therapy) trial. J Am Heart Assoc. 2017;6(9):e006695.
Kocyigit D, Tokgozoglu L, Kayikcioglu M, Altay S, Aydogdu S, Barcin C, et al. Is there a gender gap in secondary prevention of coronary artery disease in Turkey? Turk Kardiyol Dern Ars. 2018;46(8):683–91.
Figueiredo JHC, Silva N, Pereira BB, Oliveira GMM. Major depression and acute coronary syndrome-related factors. Arq Bras Cardiol. 2017;108(3):217–27.
Stanicki P, Szarpak J, Wieteska M, Kaczynska A, Milanowska J. Postoperative depression in patients after coronary artery bypass grafting (CABG)—a review of the literature. Pol Przegl Chir. 2020;92(6):32–8.
Aguayo E, Lyons R, Juo YY, Bailey KL, Seo YJ, Dobaria V, et al. Impact of new-onset postoperative depression on readmission outcomes after surgical coronary revascularization. J Surg Res. 2019;233:50–6.
Rawashdeh SI, Ibdah R, Kheirallah KA, Al-Kasasbeh A, Raffee LA, Alrabadi N, et al. Prevalence estimates, severity, and risk factors of depressive symptoms among coronary artery disease patients after ten days of percutaneous coronary intervention. Clin Pract Epidemiol Ment Health. 2021;17:103–13.
Feng L, Li L, Liu W, Yang J, Wang Q, Shi L, et al. Prevalence of depression in myocardial infarction: a PRISMA-compliant meta-analysis. Medicine (Baltimore). 2019;98(8):e14596.
• Buckland SA, Pozehl B, Yates B. Depressive symptoms in women with coronary heart disease: a systematic review of the longitudinal literature. J Cardiovasc Nurs. 2019;34(1):52–9. Systematic review of longitudinal studies on the prevalence, changes in symptoms over time, and differences in diagnostic modalities among women with depressive symptoms and coronary heart disease, including comparisons by sex/gender where available.
Tran J, Norton R, Conrad N, Rahimian F, Canoy D, Nazarzadeh M, et al. Patterns and temporal trends of comorbidity among adult patients with incident cardiovascular disease in the UK between 2000 and 2014: a population-based cohort study. PLoS Med. 2018;15(3):e1002513.
Piwonski J, Piwonska A, Jedrusik P, Stokwiszewski J, Rutkowski M, Bandosz P, et al. Depressive symptoms and cardiovascular diseases in the adult Polish population. Results of the NATPOL2011 study. Kardiol Pol. 2019;77(1):18–23.
Kim NH, Lee YH, Kim M. Community-dwelling individuals with coronary artery disease have higher risk of depression than the general population in female, but not in male. Korean Circ J. 2021;51(9):752–63.
May HT, Horne BD, Knight S, Knowlton KU, Bair TL, Lappe DL, et al. The association of depression at any time to the risk of death following coronary artery disease diagnosis. Eur Heart J Qual Care Clin Outcomes. 2017;3(4):296–302.
Smilowitz NR, Mahajan AM, Roe MT, Hellkamp AS, Chiswell K, Gulati M, et al. Mortality of myocardial infarction by sex, age, and obstructive coronary artery disease status in the ACTION Registry-GWTG (acute coronary treatment and intervention outcomes network registry-get with the guidelines). Circ Cardiovasc Qual Outcomes. 2017;10(12):e003443.
• Cenko E, Yoon J, Kedev S, Stankovic G, Vasiljevic Z, Krljanac G, et al. Sex differences in outcomes after STEMI: effect modification by treatment strategy and age. JAMA Intern Med. 2018;178(5):632–9. Study of mortality following STEMI, showing greater mortality among women under the age of 60 years compared to similarly aged men; there is no sex/gender gap in mortality in older women.
Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med. 1999;341(4):217–25.
Manfrini O, Cenko E, Bugiardini R. Gender differences in residual risk factors for major adverse cardiovascular events following ACS and how to bridge the gap. Curr Atheroscler Rep. 2020;22(11):65.
Hagstrom E, Norlund F, Stebbins A, Armstrong PW, Chiswell K, Granger CB, et al. Psychosocial stress and major cardiovascular events in patients with stable coronary heart disease. J Intern Med. 2018;283(1):83–92.
Wu Q, Kling JM. Depression and the risk of myocardial infarction and coronary death: a meta-analysis of prospective cohort studies. Medicine (Baltimore). 2016;95(6):e2815.
Vaccarino V, Bremner JD. Behavioral, emotional and neurobiological determinants of coronary heart disease risk in women. Neurosci Biobehav Rev. 2017;74(Pt B):297–309.
Humphries KH, Izadnegahdar M, Sedlak T, Saw J, Johnston N, Schenck-Gustafsson K, et al. Sex differences in cardiovascular disease—impact on care and outcomes. Front Neuroendocrinol. 2017;46:46–70.
Oram S, Khalifeh H, Howard LM. Violence against women and mental health. Lancet Psychiatry. 2017;4(2):159–70.
Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):953–62.
Boyle SH, Samad Z, Becker RC, Williams R, Kuhn C, Ortel TL, et al. Depressive symptoms and mental stress-induced myocardial ischemia in patients with coronary heart disease. Psychosom Med. 2013;75(9):822–31.
Vaccarino V, Wilmot K, Al Mheid I, Ramadan R, Pimple P, Shah AJ, et al. Sex differences in mental stress-induced myocardial ischemia in patients with coronary heart disease. J Am Heart Assoc. 2016;5(9):e003630.
Vaccarino V, Sullivan S, Hammadah M, Wilmot K, Al Mheid I, Ramadan R, et al. Mental stress-induced-myocardial ischemia in young patients with recent myocardial infarction: sex differences and mechanisms. Circulation. 2018;137(8):794–805.
Sullivan S, Hammadah M, Wilmot K, Ramadan R, Pearce BD, Shah A, et al. Young women with coronary artery disease exhibit higher concentrations of interleukin-6 at baseline and in response to mental stress. J Am Heart Assoc. 2018;7(23):e010329.
van der Meer RE, Maas AH. The role of mental stress in ischaemia with no obstructive coronary artery disease and coronary vasomotor disorders. Eur Cardiol. 2021;16:e37.
Klakk H, Kristensen PL, Andersen LB, Froberg K, Moller NC, Grontved A. Symptoms of depression in young adulthood is associated with unfavorable clinical- and behavioral cardiovascular disease risk factors. Prev Med Rep. 2018;11:209–15.
Arigo D, Ainsworth MC, Pasko K, Brown MM, Travers L. Predictors of change in BMI over 10 years among midlife and older adults: associations with gender, CVD risk status, depressive symptoms, and social support. Soc Sci Med. 2021;279:113995.
Gillespie SL, Anderson CM, Zhao S, Tan Y, Kline D, Brock G, et al. Allostatic load in the association of depressive symptoms with incident coronary heart disease: the Jackson Heart Study. Psychoneuroendocrinology. 2019;109:104369.
Szlejf C, Suemoto CK, Santos IS, Brunoni AR, Nunes MA, Viana MC, et al. Poorer cardiovascular health is associated with psychiatric comorbidity: results from the ELSA-Brasil Study. Int J Cardiol. 2019;274:358–65.
Bousquet-Santos K, Chen R, Kubzansky LD. A sad heart: depression and favorable cardiovascular health in Brazil. Prev Med. 2021;142:106378.
Cramer H, Lauche R, Adams J, Frawley J, Broom A, Sibbritt D. Is depression associated with unhealthy behaviors among middle-aged and older women with hypertension or heart disease? Womens Health Issues. 2020;30(1):35–40.
Allabadi H, Probst-Hensch N, Alkaiyat A, Haj-Yahia S, Schindler C, Kwiatkowski M, et al. Mediators of gender effects on depression among cardiovascular disease patients in Palestine. BMC Psychiatry. 2019;19(1):284.
Xu H, Deng K, Lin Z, Huang Z, Gong X, Tan J, et al. The effects of physical activity and sedentary behavior in the associations between cardiovascular diseases and depression: a four-way decomposition. J Affect Disord. 2020;275:194–201.
Achttien R, van Lieshout J, Wensing M, van der Sanden MN, Staal JB. Symptoms of depression are associated with physical inactivity but not modified by gender or the presence of a cardiovascular disease; a cross-sectional study. BMC Cardiovasc Disord. 2019;19(1):95.
Marzolini S, Colella TJF. Factors that predispose women to greater depressive symptoms: a sex-, age-, and diagnosis-matched cardiac rehabilitation cohort. Can J Cardiol. 2021;37(3):382–90.
Peltier MR, Flores JM, Smith PH, Roberts W, Verplaetse TL, Moore KE, et al. Smoking across the menopausal transition in a 10-year longitudinal sample: the role of sex hormones and depressive symptoms. Nicotine Tob Res. 2020;22(6):872–7.
Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011;378(9799):1297–305.
Goldstein BI, Carnethon MR, Matthews KA, McIntyre RS, Miller GE, Raghuveer G, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(10):965–86.
Mattina GF, Van Lieshout RJ, Steiner M. Inflammation, depression and cardiovascular disease in women: the role of the immune system across critical reproductive events. Ther Adv Cardiovasc Dis. 2019;13:1753944719851950.
Birur B, Amrock EM, Shelton RC, Li L. Sex differences in the peripheral immune system in patients with depression. Front Psychiatry. 2017;8:108.
Mommersteeg PMC, Naude PJW, Bagijn W, Widdershoven J, Westerhuis B, Schoemaker RG. Gender differences in associations of depressive symptoms and anxiety with inflammatory markers in patients with non-obstructive coronary artery disease. J Psychosom Res. 2019;125:109779.
Lawes S, Demakakos P, Steptoe A, Lewis G, Carvalho LA. Combined influence of depressive symptoms and systemic inflammation on all-cause and cardiovascular mortality: evidence for differential effects by gender in the English Longitudinal Study of Ageing. Psychol Med. 2019;49(9):1521–31.
Vaccarino V, Johnson BD, Sheps DS, Reis SE, Kelsey SF, Bittner V, et al. Depression, inflammation, and incident cardiovascular disease in women with suspected coronary ischemia: the National Heart, Lung, and Blood Institute-sponsored WISE study. J Am Coll Cardiol. 2007;50(21):2044–50.
Slavich GM, Sacher J. Stress, sex hormones, inflammation, and major depressive disorder: extending social signal transduction theory of depression to account for sex differences in mood disorders. Psychopharmacology. 2019;236(10):3063–79.
Penninx BW. Depression and cardiovascular disease: epidemiological evidence on their linking mechanisms. Neurosci Biobehav Rev. 2017;74(Pt B):277–86.
Garcia RG, Mareckova K, Holsen LM, Cohen JE, Whitfield-Gabrieli S, Napadow V, et al. Impact of sex and depressed mood on the central regulation of cardiac autonomic function. Neuropsychopharmacology. 2020;45(8):1280–8.
Tobaldini E, Carandina A, Toschi-Dias E, Erba L, Furlan L, Sgoifo A, et al. Depression and cardiovascular autonomic control: a matter of vagus and sex paradox. Neurosci Biobehav Rev. 2020;116:154–61.
Schulman-Marcus J, Shah T, Swaminathan RV, Feldman DN, Wong SC, Singh HS, et al. Comparison of recent trends in patients with and without major depression and acute ST-elevation myocardial infarction. Am J Cardiol. 2016;118(6):779–84.
Fleetwood K, Wild SH, Smith DJ, Mercer SW, Licence K, Sudlow CLM, et al. Severe mental illness and mortality and coronary revascularisation following a myocardial infarction: a retrospective cohort study. BMC Med. 2021;19(1):67.
Mohamed MO, Rashid M, Farooq S, Siddiqui N, Parwani P, Shiers D, et al. Acute myocardial infarction in severe mental illness: prevalence, clinical outcomes, and process of care in U.S. hospitalizations. Can J Cardiol. 2019;35(7):821–30.
Zambrano J, Celano CM, Januzzi JL, Massey CN, Chung WJ, Millstein RA, et al. Psychiatric and psychological interventions for depression in patients with heart disease: a scoping review. J Am Heart Assoc. 2020;9(22):e018686.
Reavell J, Hopkinson M, Clarkesmith D, Lane DA. Effectiveness of cognitive behavioral therapy for depression and anxiety in patients with cardiovascular disease: a systematic review and meta-analysis. Psychosom Med. 2018;80(8):742–53.
Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA. 2003;289(23):3106–16.
Davidson KW, Bigger JT, Burg MM, Carney RM, Chaplin WF, Czajkowski S, et al. Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: CODIACS vanguard randomized controlled trial. JAMA Intern Med. 2013;173(11):997–1004.
Jee YH, Chang H, Jung KJ, Jee SH. Cohort study on the effects of depression on atherosclerotic cardiovascular disease risk in Korea. BMJ Open. 2019;9(6):e026913.
Herrmann-Lingen C, Beutel ME, Bosbach A, Deter HC, Fritzsche K, Hellmich M, et al. A stepwise psychotherapy intervention for reducing risk in coronary artery disease (SPIRR-CAD): results of an observer-blinded, multicenter, randomized trial in depressed patients with coronary artery disease. Psychosom Med. 2016;78(6):704–15.
Deter HC, Weber C, Herrmann-Lingen C, Albus C, Juenger J, Ladwig KH, et al. Gender differences in psychosocial outcomes of psychotherapy trial in patients with depression and coronary artery disease. J Psychosom Res. 2018;113:89–99.
Norlund F, Wallin E, Olsson EMG, Wallert J, Burell G, von Essen L, et al. Internet-based cognitive behavioral therapy for symptoms of depression and anxiety among patients with a recent myocardial infarction: the U-CARE heart randomized controlled trial. J Med Internet Res. 2018;20(3):e88.
Hankivsky O. Women’s health, men’s health, and gender and health: implications of intersectionality. Soc Sci Med. 2012;74(11):1712–20.
Bowleg L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–73.
Vaughan AS, Quick H, Schieb L, Kramer MR, Taylor HA, Casper M. Changing rate orders of race-gender heart disease death rates: an exploration of county-level race-gender disparities. SSM Popul Health. 2019;7:100334.
Schneiderman N, Saab PG, Catellier DJ, Powell LH, DeBusk RF, Williams RB, et al. Psychosocial treatment within sex by ethnicity subgroups in the Enhancing Recovery in Coronary Heart Disease clinical trial. Psychosom Med. 2004;66(4):475–83.
Smolderen KG, Brush A, Dreyer RP. Psychosocial factors and recovery after acute myocardial infarction in younger women. Curr Cardiol Rep. 2019;21(6):50.
Funding
This work was supported by funds from the National Institutes of Health (R01 HL114924). The NIH had no role in the design and conduct of the study, including the collection, management, analysis, interpretation of the data, preparation, review or approval of the manuscript, and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Drs. DR and NM had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: DR, NM; acquisition of data: DR, AS, JU; analysis and interpretation of data: DR, AS; drafting of the manuscript: DR, NM; critical revision of manuscript for important intellectual content: RL, JU, TC, CM, KGS, NM; statistical analysis: N/A; obtained funding: NM; study supervision: NM.
Corresponding author
Ethics declarations
Competing Interests
Dr. Smolderen reports grants from Merck, Shockwave, Cardinal Health, and Johnson & Johnson, and personal fees from Optum, Cook Medical, and Abbott, outside the submitted work. Dr. Cornelius reports grants from NIH/NCATS (KL2 TR001874), during the conduct of the study (the content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH); and other from Transcendent Endeavors, LLC, outside the submitted work. The other authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Women and Ischemic Heart Disease
Supplementary Information
ESM 1
(DOCX 12.7 KB)
Rights and permissions
About this article
Cite this article
Rome, D., Sales, A., Leeds, R. et al. A Narrative Review of the Association Between Depression and Heart Disease Among Women: Prevalence, Mechanisms of Action, and Treatment. Curr Atheroscler Rep 24, 709–720 (2022). https://doi.org/10.1007/s11883-022-01048-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-022-01048-0