Abstract
Purpose of Review
Occupational rhinitis is an underdiagnosed disease with significant morbidity and implications in the workplace. Multiple factors associated with this disease continue to pose a challenge to investigators. This review aims to summarize recent literature in occupational rhinitis, including classifications, pathogenesis, diagnosis, and treatment, as well as the impact of occupational rhinitis on individuals. Additionally, it identifies areas in need of further research and investigation.
Recent Findings
We highlight current research on the association between occupational rhinitis and occupational asthma and the role of immunotherapy in this disease. Discussion includes the impact of social trends on workers and the wider consequences of occupational rhinitis including decreased work productivity, absenteeism, and socioeconomic burden.
Summary
Occupational rhinitis remains a challenging disease entity due to the numerous potential causative factors, reduced recognition, morbidity in asthma, and therapeutic limitations. Additional research is needed to better identify disease predictors and develop effective management strategies.

Similar content being viewed by others
REFERENCES
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hox V, et al. Occupational upper airway disease: how work affects the nose. Allergy. 2014;69(3):282–91.
Moscato G, Siracusa A. Rhinitis guidelines and implications for occupational rhinitis. Curr Opin Allergy Clin Immunol. 2009;9(2):110–5.
Dykewicz MS, et al. Rhinitis 2020: A practice parameter update. J Allergy Clin Immunol. 2020;146(4):721–67.
Vandenplas O, et al. Impact of Rhinitis on Work Productivity: A Systematic Review. J Allergy Clin Immunol Pract. 2018;6(4):1274-1286 e9.
Siracusa A, Desrosiers M, Marabini A. Epidemiology of occupational rhinitis: prevalence, aetiology and determinants. Clin Exp Allergy. 2000;30(11):1519–34.
Vandenplas O, Hox V, Bernstein D. Occupational Rhinitis. J Allergy Clin Immunol Pract. 2020;8(10):3311–21.
Hellings PW, et al. Non-allergic rhinitis: Position paper of the European Academy of Allergy and Clinical Immunology. Allergy. 2017;72(11):1657–65.
Segboer CL, et al. Quality of life is significantly impaired in nonallergic rhinitis patients. Allergy. 2018;73(5):1094–100.
Avdeeva KS, et al. The prevalence of non-allergic rhinitis phenotypes in the general population: A cross-sectional study. Allergy. 2022;77(7):2163–74.
Maoua M, Rouis H. Occupational Rhinitis and Asthma in the Textile Sector of the Central Region of Tunisia. Int J Respiratory Pulmon Med. 2018;5.
Ameille J, et al. Occupational asthma and occupational rhinitis: the united airways disease model revisited. Occup Environ Med. 2013;70(7):471–5.
Moscato G, et al. Occupational rhinitis affects occupational asthma severity. J Occup Health. 2016;58(3):310–3.
Balogun RA, Siracusa A, Shusterman D. Occupational rhinitis and occupational asthma: Association or progression? Am J Ind Med. 2018;61(4):293–307.
da Paz ER, et al. Airway inflammatory profile among cleaning workers from different workplaces. BMC Pulm Med. 2022;22(1):170.
Sonday Z, Jeebhay M. Occupational rhinitis and asthma due to lentil and split pea allergy in a food-handler 2022. Curr Opin Allergy Clin Immunol. 2022;35:35–43.
Jungewelter S, Airaksinen L, Pesonen M. Occupational rhinitis, asthma, and contact urticaria from IgE-mediated allergy to pork. Am J Ind Med. 2019;62(1):80–4.
Kuske M, et al. Occupational allergy to phytase: case series of eight production workers exposed to animal feed additives. J Dtsch Dermatol Ges. 2020;18(8):859–65.
Chemingui S, et al. RF-417 Occupational Rhinitis and Asthma Caused by Isocyanates. BMJ Publishing Group Ltd. 2021.
Hollund BE, et al. Prevalence of airway symptoms among hairdressers in Bergen. Norway Occup Environ Med. 2001;58(12):780–5.
Macan J, et al. Respiratory toxicity of persulphate salts and their adverse effects on airways in hairdressers: a systematic review. Int Arch Occup Environ Health. 2022;95(8):1679–702.
Foss-Skiftesvik MH, et al. High occurrence of rhinitis symptoms in hairdressing apprentices. Int Forum Allergy Rhinol. 2017;7(1):43–9.
• Haltia T, et al. Occupational asthma, rhinitis, and contact urticaria from indigo (Indigofera tinctoria) hair dye. J Allergy Clin Immunol Pract. 2021;9(9):3500-3502. Describes sensatization to organic products amongst hairdressers.
Villalobos V, et al. Occupational Asthma and Rhinitis due to Yellow and Red Henna in a Hairdresser. J Investig Allergol Clin Immunol. 2020;30(2):133–4.
Pyana Kitenge J, et al. Occupational rhinitis and asthma in bakers: a cross-sectional study in the former Katanga province of DR Congo. International Archives of Occupational and Environmental Health. 2022;95(1):293–301.
•• Olivieri M, et al. Exposure to additives or multigrain flour is associated with high risk of work-related allergic symptoms among bakers. Occup Environ Med. 2021;78(2):112-116. Describes the complexity of baker's rhinitis and asthma and the effect of different flour components in symptoms.
• Jungewelter S, Suomela S, Airaksinen L. Occupational IgE-mediated psyllium allergy in contemporary gluten-free and vegan baking: A case of allergic rhinitis. Am J Ind Med. 2021;64(5):431-434. Highlights the effect of social trends in the recognition of new agents leading to occupational rhinitis.
• Jungewelter S, Airaksinen L, Pesonen M. Occupational buckwheat allergy as a cause of allergic rhinitis, asthma, contact urticaria and anaphylaxis-An emerging problem in food-handling occupations? Am J Ind Med. 2020;63(11):1047-1053. Presents the case of workers becoming sensitized to buckwheat when used as a gluten free-alternative in the workplace.
Bachert C. Persistent rhinitis - allergic or nonallergic? Allergy. 2004;59 Suppl 76:11-5; discussion 15.
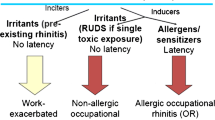
Kotz S, et al. Occupational rhinitis Allergol Select. 2021;5:51–6.
Brooks SM, Weiss MA, Bernstein IL. Reactive airways dysfunction syndrome (RADS). Persistent asthma syndrome after high level irritant exposures. Chest. 1985;88(3):376-84.
Meggs WJ, et al. Nasal pathology and ultrastructure in patients with chronic airway inflammation (RADS and RUDS) following an irritant exposure. J Toxicol Clin Toxicol. 1996;34(4):383–96.
Lemiere C, et al. Irritant-Induced Asthma. J Allergy Clin Immunol Pract. 2022;10(11):2799–806.
Vandenplas O, et al. EAACI position paper: irritant-induced asthma. Allergy. 2014;69(9):1141–53.
Ogi K, et al. Trimellitic anhydride facilitates transepithelial permeability disrupting tight junctions in sinonasal epithelial cells. Toxicol Lett. 2021;353:27–33.
•• Nakonechna A, Matthews D, Sargur R. Occupational asthma, rhinitis, contact dermatitis, and severe milk allergy caused by primary occupational exposure to casein. Ann Allergy Asthma Immunol. 2019;123(2):224-225. Presents a rare case of occupational asthma, rhinitis, urticaria, and severe milk allergy in a laboratory worker sensitized to casein after working with culture media powder containing casein.
Sibanda E, Makaza N. Health effects of diesel engine exhaust emissions exposure (DEEE) can mimic allergic asthma and rhinitis. Allergy Asthma Clin Immunol. 2019;15:31.
Varghese M, Glaum MC, Lockey RF. Drug-induced rhinitis. Clin Exp Allergy. 2010;40(3):381–4.
Lee WH, et al. Effects of cigarette smoking on rhinologic diseases: Korean National Health and Nutrition Examination Survey 2008–2011. Int Forum Allergy Rhinol. 2015;5(10):937–43.
Hisinger-Molkanen H, et al. Smoking, environmental tobacco smoke and occupational irritants increase the risk of chronic rhinitis. World Allergy Organ J. 2018;11(1):6.
Konno S, et al. The prevalence of rhinitis and its association with smoking and obesity in a nationwide survey of Japanese adults. Allergy. 2012;67(5):653–60.
Wang S, et al. Smoking behavior might affect allergic rhinitis and vasomotor rhinitis differently: A mendelian randomization appraisal. World Allergy Organ J. 2022;15(2): 100630.
Lucas D, et al. Occupational asthma, rhinitis and contact urticaria in a salmon-processing worker. Int Marit Health. 2022;73(3):112–4.
Romita P, et al. Occupational allergic rhinitis and contact urticaria caused by Gum Arabic in a candy factory worker. Contact Dermatitis. 2018;78(6):427–8.
Sokol KC, Hamilos DL. Occupational Rhinitis. In: Bernstein JA, editor. Rhinitis and Related Upper Respiratory Conditions: A Clinical Guide. Cham: Springer International Publishing; 2018. p. 59–66.
• Touati N, et al. An Unusual Case of Occupational Rhinitis. J Investig Allergol Clin Immunol. 2020;30(3):207-208. Describes the use of patch testing in conjunction with SPT in the assessment of OR with suspected underlying T-cell mediated hypersensitivity reactions.
Cantone E, Detoraki A, De Corso E. Local Allergic Rhinitis: A Different Rhinitis Endotype? Literature Overview. Appl Sci. 2022;12. https://doi.org/10.3390/app122111141.
•• Ronsmans S, et al. Diagnostic approach to occupational rhinitis: the role of nasal provocation tests. Curr Opin Allergy Clin Immunol. 2020;20(2):122-130. Describes the role of NPTs in ocuppational rhinitis and considerations to keep in mind when using HMW and LMW agents that are not standardized.
Hellgren J, Karlsson G, Toren K. The dilemma of occupational rhinitis: management options. Am J Respir Med. 2003;2(4):333–41.
Wagoner WW, et al. Treatment of Maize-Based Occupational Rhinitis By Phleum Pretense Subcutaneous Immunotherapy. J Allergy Clin Immunol. 2017;139(2, Supplement):AB152.
•• Dubini M, et al. Occupational asthma and rhinitis due to wheat flour: sublingual specific immunotherapy treatment. Med Lav. 2020;111(3):203-209. Highlights the use of SLIT in the management of baker's rhinitis and asthma.
Maoua M, et al. Quality of Life and Work Productivity Impairment of Patients with Allergic Occupational Rhinitis. Tanaffos. 2019;18(1):58–65.
•• Vandenplas O, et al. The Impact of Work-Related Rhinitis on Quality of Life and Work Productivity: A General Workforce-Based Survey. J Allergy Clin Immunol Pract. 2020;8(5):1583-1591 e5. Presents evidence showing that WRR has a significant impact on QoL and work productivity.
Funding
JAP receives funding from National Institute for Occupational Safety and Health (R01:OH012045), Department of Defense (PR200793) and Central States Center of Agricultural Safety and Health (CS-CASH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
JAP has received research regents (no monies) from AstraZeneca and is clinical site recruiter for asthma and sinus disease studies for GlaxoSmithKline, AstraZeneca, and Regeneron Pharmaceuticals.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zamora-Sifuentes, J., Poole, J.A. Occupational Rhinitis: An Update. Curr Allergy Asthma Rep 23, 579–587 (2023). https://doi.org/10.1007/s11882-023-01103-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-023-01103-z