Abstract
Purpose of Review
Adverse drug reactions (ADRs) are a significant cause of morbidity and mortality. The electronic health record (EHR) provides an opportunity to monitor ADRs, mainly through the utilization of drug allergy data and pharmacogenomics. This review article explores the current use of the EHR for ADR monitoring and highlights areas that require improvement.
Recent Findings
Recent research has identified several issues with using EHR for ADR monitoring. These include the lack of standardization between EHR systems, specificity in data entry options, incomplete and inaccurate documentation, and alert fatigue. These issues can limit the effectiveness of ADR monitoring and compromise patient safety.
Summary
The EHR has great potential for monitoring ADR but needs significant updates to improve patient safety and optimize care. Future research should concentrate on developing standardized documentation and clinical decision support systems within EHRs. Healthcare professionals should also be educated on the significance of accurate and complete ADR monitoring.

Similar content being viewed by others
Abbreviations
- AAAAI:
-
American Academy of Allergy, Asthma & Immunology
- ADRs:
-
Adverse drug reactions
- CDS:
-
Clinical decision support
- CPIC:
-
Clinical Pharmacogenetics Implementation Consortium
- CPOE:
-
Computerized physician order entry
- DAL:
-
Drug allergy label
- EHR:
-
Electronic health record
- HCP:
-
Healthcare professional
- HLA:
-
Human leukocyte antigen
- HSR:
-
Hypersensitivity reaction
- PharmGKB:
-
Pharmacogenomics Knowledgebase
- PharmVar:
-
Pharmacogene Variation Consortium
- PGx:
-
Pharmacogenomic
- US:
-
United States
- USFDA:
-
United States Food and Drug Association
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Khan DA, et al. Drug allergy: a 2022 practice parameter update. J Allergy Clin Immunol. 2022. https://doi.org/10.1016/j.jaci.2022.08.028.
Pichler WJ. Immune pathomechanism and classification of drug hypersensitivity. Allergy: Eur J Allergy Clin Immunol. Blackwell Publishing Ltd. 2019;74(8):1457–71. https://doi.org/10.1111/all.13765.
Schmid O, Bereznicki B, Peterson GM, Stankovich J, Bereznicki L. Persistence of adverse drug reaction-related hospitalization risk following discharge. Int J Environ Res Public Health. 2022;19(9). https://doi.org/10.3390/ijerph19095585.
Forster AJ, Jennings A, Chow C, Leeder C, van Walraven C. A systematic review to evaluate the accuracy of electronic adverse drug event detection. J Am Med Inform Assoc. 2012;19(1):31–8. https://doi.org/10.1136/amiajnl-2011-000454.
Ball R, Robb M, Anderson SA, Dal Pan G. The FDAs sentinel initiative—a comprehensive approach to medical product surveillance. Clin Pharmacol Ther. 2016;99(3):265–8. Nature Publishing Group. https://doi.org/10.1002/cpt.320.
Kwan JL, et al. Computerised clinical decision support systems and absolute improvements in care: meta-analysis of controlled clinical trials. BMJ. 2020;370. https://doi.org/10.1136/bmj.m3216.
Goss FR, Plasek JM, Lau JJ, Seger DL, Chang FY, Zhou L. An evaluation of a natural language processing tool for identifying and encoding allergy information in emergency department clinical notes. AMIA Annu Symp Proc. 2014;2014:580–8.
Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients a meta-analysis of prospective studies. [Online]. https://jamanetwork.com/.
Iammatteo M, et al. Identifying allergic drug reactions through placebo-controlled graded challenges, J Allergy Clin Immunol. In Pract. 2017;5(3):711-717.e2. https://doi.org/10.1016/j.jaip.2016.09.041.
Iammatteo M, et al. Safety and outcomes of oral graded challenges to amoxicillin without prior skin testing, J Allergy Clin Immunol. In Pract. 2019;7(1):236–43. https://doi.org/10.1016/j.jaip.2018.05.008.
Zhou L, et al. Drug allergies documented in electronic health records of a large healthcare system. Allergy: Eur J Allergy Clin Immunol. 2016;71(9):1305–13. https://doi.org/10.1111/all.12881.
Wang L, et al. A dynamic reaction picklist for improving allergy reaction documentation in the electronic health record. J Am Med Inform Assoc. 2020;27(6):917–23. https://doi.org/10.1093/jamia/ocaa042.
Ho T-B, Le L, Thai DT, Taewijit S. Data-driven approach to detect and predict adverse drug reactions. Curr Pharm Des. 2016;22:3498–526. [Online]. https://www.nlm.nih.gov/bsd/pmresources.html.
Bailey C, et al. Adverse drug event reporting systems: a systematic review. Br J Clin Pharmacol. Blackwell Publishing Ltd. 2016:17–29. https://doi.org/10.1111/bcp.12944.
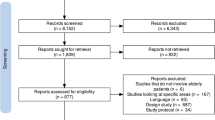
•• Bassir F, Varghese S, Wang L, Chin YP, Zhou L. The use of electronic health records to study drug-induced hypersensitivity reactions from 2000 to 2021: a systematic review. Immunol Allergy Clin. 2022;42(2):453–97. Systematic review of EHR use in drug allergy research from 2000 to 2021 highlights the need to improve clinical documentation and CDS alerting to enhance patient safety.
Pasternak AL, et al. Establishment of a pharmacogenetics service focused on optimizing existing pharmacogenetic testing at a large academic health center. J Pers Med. 2020;10(4):1–10. https://doi.org/10.3390/jpm10040154.
Martin MA, Klein TE, Dong BJ, Pirmohamed M, Haas DW, Kroetz DL. Clinical pharmacogenetics implementation consortium guidelines for HLA-B genotype and abacavir dosing. Clin Pharmacol Ther. 2012;91(4):734–8. https://doi.org/10.1038/clpt.2011.355.
Hershfield MS, et al. Clinical pharmacogenetics implementation consortium guidelines for human leukocyte antigen-b genotype and allopurinol dosing. Clin Pharmacol Ther. 2013;93(2):153–8. https://doi.org/10.1038/clpt.2012.209.
Caudle KE et al. Clinical pharmacogenetics implementation consortium guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing, Clin Pharmacol Ther. 2014;9(5):542–8. Nature Publishing Group. https://doi.org/10.1038/clpt.2014.159.
Slight SP, et al. A cross-sectional observational study of high override rates of drug allergy alerts in inpatient and outpatient settings, and opportunities for improvement. BMJ Qual Saf. 2017;26(3):217–25. https://doi.org/10.1136/bmjqs-2015-004851.
Blumenthal KG, Park MA, Macy EM. Redesigning the allergy module of the electronic health record. Ann Allergy Asthma Immunol. 2016;117(2):126–31. https://doi.org/10.1016/j.anai.2016.05.017.
Goss FR, et al. A value set for documenting adverse reactions in electronic health records. J Am Med Inform Assoc. 2018;25(6):661–9. https://doi.org/10.1093/jamia/ocx139.
Rukasin CRF, Henderlight S, Bosen T, Nelson SD, Phillips EJ. Implications of electronic health record transition on drug allergy labels. J Allergy Clin Immunol. In Pract. 2020;8(2):764–6. https://doi.org/10.1016/j.jaip.2019.07.017.
Alvarez-Arango S, et al. Vancomycin hypersensitivity reactions documented in electronic health records. J Allergy Clin Immunol. In Pract. 2021;9(2):906–12. https://doi.org/10.1016/j.jaip.2020.09.027.
Shah NS, Ridgway JP, Pettit N, Fahrenbach J, Robicsek A. Documenting penicillin allergy: the impact of inconsistency. PLoS One. 11(3). https://doi.org/10.1371/journal.pone.0150514.
Lyons N, Rankin S, Sarangarm P, Washington C, Weiss SJ, Ernst AA. Disparity in patients’ self-reported and charted medication allergy information. South Med J. 2015;108(6):332–6. https://doi.org/10.14423/SMJ.0000000000000301.
Cavallari LH, et al. Institutional profile: University of Florida health personalized medicine program. Pharmacogenomics. 2017;18(5):421–6. https://doi.org/10.2217/pgs-2017-0028.
Hertz DL, et al. Institutional profile of pharmacogenetics within University of Michigan College of Pharmacy. Pharmacogenomics. 2017;18(12). https://doi.org/10.2217/pgs-2017-0107.
Hoffman JM, et al. PG4KDS: a model for the clinical implementation of pre-emptive pharmacogenetics. Am J Med Genet C Semin Med Genet. 2014;166(1):45–55. https://doi.org/10.1002/ajmg.c.31391.
Dunnenberger HM, et al. Implementation of a multidisciplinary pharmacogenomics clinic in a community health system. Am J Health Syst Pharm. 2016;73(23):1956–66. https://doi.org/10.2146/ajhp160072.
Dolan ME, Maitland ML, O’Donnell PH, Nakamura Y, Cox NJ, Ratain MJ. Institutional profile: University of Chicago Center for Personalized Therapeutics: research, education and implementation science. Pharmacogenomics. 2013;14(12):1383–7. https://doi.org/10.2217/pgs.13.134.
Johansen Taber KA, Dickinson BD. Pharmacogenomic knowledge gaps and educational resource needs among physicians in selected specialties. Pharmacogenomics Pers Med. 2014;7(1):145–62. https://doi.org/10.2147/PGPM.S63715.
Beitelshees AL, et al. Evaluating the extent of reusability of CYP2C19 genotype data among patients genotyped for antiplatelet therapy selection. Genet Med. 2020;22(11):1898–902. https://doi.org/10.1038/s41436-020-0894-2.
Caudle KE, Keeling NJ, Klein TE, Whirl-Carrillo M, Pratt VM, Hoffman JM. Standardization can accelerate the adoption of pharmacogenomics: current status and the path forward. Pharmacogenomics. Future Medicine Ltd. 2018;19(10):847–60. https://doi.org/10.2217/pgs-2018-0028.
Shakib S, Caughey GE, Fok JS, Smith B. Adverse drug reaction classification by health professionals: appropriate discrimination between allergy and intolerance? Clin Transl Allergy. 2019;9(1). https://doi.org/10.1186/s13601-019-0259-6.
Blumenthal KG, Ryan EE, Li Y, Lee H, Kuhlen JL, Shenoy ES. The impact of a reported penicillin allergy on surgical site infection risk. Clin Infect Dis. 2018;66(3):329–36.
Inglis JM, Caughey GE, Smith W, Shakib S. Documentation of penicillin adverse drug reactions in electronic health records: inconsistent use of allergy and intolerance labels. Intern Med J. 2017;47(11):1292–7. https://doi.org/10.1111/imj.13558.
Gerace KS, Phillips E. Penicillin allergy label persists despite negative testing. J Allergy Clin Immunol Pract. 2015;3:815–6.
Ramsey A, Macy E, Chiriac AM, Blumenthal KG. Drug allergy labels lost in translation: from patient to charts and backwards, J Allergy Clin Immunol. In Pract. 2021;9(8):3015–20. https://doi.org/10.1016/j.jaip.2021.02.005.
• Phadke NA, et al. Allergy safety events in health care: development and application of a classification schema based on retrospective review, J Allergy Clin Immunol. In Pract. 2022;10(7):1844–55.e3. https://doi.org/10.1016/j.jaip.2022.03.026. Classification schema based on a retrospective review to identify failures that can cause allergy-related safety events. Findings suggest that using such a schema can help improve allergy safety practices by identifying areas for improvement.
Guyer AC, et al. Allergy electronic health record documentation: a 2022 work group report of the AAAAI adverse reactions to drugs, biologicals, and latex committee. J Allergy Clin Immunol. In Pract. 2022;10(11):2854–67. https://doi.org/10.1016/j.jaip.2022.08.020.
Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–203. https://doi.org/10.1001/jama.293.10.1197.
Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006;13(5):547–56. https://doi.org/10.1197/jamia.M2042.
Topaz M, et al. Rising drug allergy alert overrides in electronic health records: an observational retrospective study of a decade of experience. J Am Med Inform Assoc. 2016;23(3):601–8. https://doi.org/10.1093/jamia/ocv143.
Joyner LM, Alicea LA, Goldman JL, Suppes SL, Tillman EM. Methods for detecting pediatric adverse drug reactions from the electronic medical record. J Clin Pharmacol. 2021;61(11):1479–84. https://doi.org/10.1002/jcph.1916.
• Wang L, Park H, Vallamkonda S, Seger DL, Blackley SV, Garabedian PM, Goss F, Blumenthal KG, Bates DW, Murphy S, Zhou L. Dynamic reaction picklist for improving allergy reaction documentation: a usability study. Int J Med Informatics. 2023;1(170):104939. The novel dynamic reaction picklist is a promising solution to improve drug allergy documentation in EHRs by reducing the use of free-text entries and decreasing the time required for documentation. This new approach can potentially address some of the challenges associated with drug allergy documentation in EHRs.
Goss FR, et al. Evaluating standard terminologies for encoding allergy information. J Am Med Inform Assoc. 2013;20(5):969–79. https://doi.org/10.1136/amiajnl-2012-000816.
Siegersma KR, Evers M, Bots SH, Groepenhoff F, Appelman Y, Hofstra L, Tulevski II, Somsen GA, den Ruijter HM, Spruit M, Onland-Moret NC. Development of a pipeline for adverse drug reaction identification in clinical notes: word embedding models and string matching. JMIR Med Inform. 2022;10(1):e31063. https://doi.org/10.2196/31063. PMID: 35076407; PMCID: PMC8826143.
Hicks JK, Dunnenberger HM, Gumpper KF, Haidar CE, Hoffman JM. Integrating pharmacogenomics into electronic health records with clinical decision support. Am J Health Syst Pharm. 2016;73(23):1967–76. https://doi.org/10.2146/ajhp160030.
Hoffman JM, et al. Developing knowledge resources to support precision medicine: principles from the Clinical Pharmacogenetics Implementation Consortium (CPIC). J Am Med Inform Assoc. 2016;23(4):796–801. https://doi.org/10.1093/jamia/ocw027.
Gage BF, Eby C, Johnson JA, Deych E, Rieder MJ, Ridker PM, Milligan PE, Grice G, Lenzini P, Rettie AE, Aquilante CL, Grosso L, Marsh S, Langaee T, Farnett LE, Voora D, Veenstra DL, Glynn RJ, Barrett A, McLeod HL. Use of pharmacogenetic and clinical factors to predict the therapeutic dose of warfarin. Clin Pharmacol Ther. 2008;84(3):326–31. https://doi.org/10.1038/clpt.2008.10. Epub 2008 Feb 27. Erratum in: Clin Pharmacol Ther. 84(3):430. PMID: 18305455; PMCID: PMC2683977.
Obeng AO, Kaszemacher T, Abul-Husn NS, Gottesman O, Vega A, Waite E, Myers K, Cho J, Bottinger EP, Ellis SB, Scott SA. Implementing algorithm-guided warfarin dosing in an ethnically diverse patient population using electronic health records and preemptive CYP2C9 and VKORC1 genetic testing. Clin Pharmacol Ther. 2016;100(5):427–30. https://doi.org/10.1002/cpt.425. Epub 2016 Aug 18. PMID: 27393744; PMCID: PMC5638436.
Van Driest SL, et al. Clinically actionable genotypes among 10,000 patients with preemptive pharmacogenomic testing. Clin Pharmacol Ther. 2014;95(4):423–31. https://doi.org/10.1038/clpt.2013.229.
Figueiras A, Herdeiro MT, Polonia J, Gestal-Otero JJ. An educational intervention to improve physician reporting of adverse drug reactions: a cluster-randomized controlled trial. JAMA. 2006;296(9):1086–93. https://doi.org/10.1001/jama.296.9.1086.
Tabali M, Jeschke E, Bockelbrink A, et al. Educational intervention to improve physician reporting of adverse drug reactions (ADRs) in a primary care setting in complementary and alternative medicine. BMC Public Health. 2009;9:274. https://doi.org/10.1186/1471-2458-9-274.
Phillips EJ, Sukasem C, Whirl-Carrillo M, Müller DJ, Dunnenberger HM, ChantratitaGoldspiel B, Chen YT, Carleton BC, George AL Jr, Mushiroda T, Klein T, Gammal RS, Pirmohamed M. Clinical pharmacogenetics implementation consortium guideline for HLA genotype and use of carbamazepine and oxcarbazepine: 2017 update. Clin Pharmacol Ther. 2018;103(4):574–81. https://doi.org/10.1002/cpt.1004.
Caudle KE, Rettie AE, Whirl-Carrillo M, Smith LH, Mintzer S, Lee MT, Klein TE, Callaghan JT; Clinical Pharmacogenetics Implementation Consortium. Clinical pharmacogenetics implementation consortium guidelines for CYP2C9 and HLA-B genotypes and phenytoin dosing. Clin Pharmacol Ther. 2014 Nov;96(5):542–8. https://doi.org/10.1038/clpt.2014.159.
Fan WL, Shiao MS, Hui RC, Su SC, Wang CW, Chang YC, Chung WH. HLA association with drug-induced adverse reactions. J Immunol Res. 2017.
Table of Pharmacogenetic Associations. https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations#about.
Acknowledgements
Dr. Alvarez-Arango receives support from the NIH-NCATS (KL2TR003099).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muzaffar, A.F., Abdul-Massih, S., Stevenson, J.M. et al. Use of the Electronic Health Record for Monitoring Adverse Drug Reactions. Curr Allergy Asthma Rep 23, 417–426 (2023). https://doi.org/10.1007/s11882-023-01087-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11882-023-01087-w