Abstract
Purpose of Review
The study of microRNA in asthma has revealed a vibrant new level of gene regulation underlying asthma pathology. Several miRNAs have been shown to be important in asthma, influencing various biological mechanisms which lead to asthma pathology and symptoms. In addition, miRNAs have been proposed as biomarkers of asthma affection status, asthma severity, and asthma treatment response. We review all recent asthma-miRNA work, while also presenting comprehensive tables of all miRNA results related to asthma.
Recent Findings
We here reviewed 63 recent studies published reporting asthma and miRNA research, and an additional 14 reviews of the same. We summarized the information for both adult and childhood asthma, as well as research on miRNAs in asthma–COPD overlap syndrome (ACOs), and virus-induced asthma exacerbations.
Summary
We attempted to present a comprehensive collection of recently published asthma-associated miRNAs as well as tables of all published asthma-related miRNA results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is one of the most prevalent non-communicable diseases, and it has a significant influence on many people’s quality of life. It affects 23.4 million people in the USA alone (5–10% of the population), including 7 million children [1]. It affects an estimated 300 million people worldwide, with another 100 million predicted to be impacted by 2025 [2]. The World Health Organization (WHO) estimates that 15 million disability-adjusted life-years are lost each year, with 250,000 asthma fatalities reported globally [3]. Asthma is the 16th greatest cause of years lived with disability and the 28th leading source of disease burden, as defined by disability-adjusted life years, globally.
Asthma is a multifaceted condition with a complex etiology involving interactions between genetic susceptibility, host factors, and environmental exposures. Environmental factors may involve exposure to air pollution, pollens, mold, aeroallergens, tobacco smoke, etc., while host factors include obesity, nutrition, infections, allergic sensitization, etc. Genetic factors include asthma susceptibility loci on genes or family history of asthma. Although the precise mechanisms of asthma are unknown, they may include airway inflammation, airway tone control, and airway responsiveness [4]. Asthma has been studied at multiple omics levels, encompassing genomes, metabolomics, epigenomics, and transcriptomics, and therefore is associated with complex cellular and genomic interactions [5, 6]. RNAs have traditionally been regarded to be molecules that solely encode genetic information for protein production, while gene modulation and cell-signaling networks have been thought to be the key regulatory systems in cells. However, following relatively recent breakthroughs in non-coding RNAs, such as the discovery of microRNAs (miRNAs), this paradigm is evolving. miRNAs are 18–22 nucleotides long and stop protein translation by interacting with mRNA [7]. Each miRNA may affect hundreds to thousands of genes and, when taken in aggregate, may lead to a combinatorial increase in regulatory complexity. Even though miRNAs were discovered about 30 years ago, their immense role in the immune system has only begun to be appreciated. miRNAs’ role has been deeply studied in several human diseases including cancer, skin conditions, and several lung disorders, including but not limited to idiopathic pulmonary fibrosis (IPF), cystic fibrosis (CF), chronic obstructive pulmonary disease (COPD), asthma, and pulmonary illness [8, 9]. In asthma, miRNAs regulate multiple pro-inflammatory pathways as well as smooth muscle cell proliferation, driving airway hyperresponsiveness and contributing to the disease’s development [10,11,12,13].
In the year leading up to this review, 63 research articles on asthma and miRNAs were published, with another 14 reviews. Here, we contribute to the previously remarkable collection of work by summarizing the quite remarkable body of work on the impact of miRNAs in asthma. Our purpose is to review the recent contributions to the field of miRNA in asthma; prior work has already been reviewed, and we refer the interested reader to other excellent reviews [10, 13,14,15,16,17,18, 19••, 20, 21, 22••, 23,24,25]. However, we have attempted to provide comprehensive treatment of the entire body of literature in our figures and tables, which we hope will be a useful reference for miRNA researchers doing work in asthma.
Asthma and miRNA
Asthma has a high degree of variability among patients, making it difficult to develop diagnostic and therapeutic tools. Chronic airway inflammation, mucus hyper-secretion, and bronchial hyper-responsiveness, as well as respiratory symptoms such as wheezing, shortness of breath, chest tightness, and cough, are all hallmarks of asthma. Asthma can further be classified into distinct mechanistic pathways or endotypes based on variable clinical presentations or phenotypes [26]. Using induced sputum or peripheral blood cytology to phenotype and endotype asthma can help with treatment responsiveness, identifying pathogenic pathways, and anticipating complications. Moreover, asthma shifts significantly throughout the lifespan. Childhood asthma is characterized by having a high general frequency, a male predominance prior to puberty, frequent remission, and rare fatality. Female preponderance, exceptional remission, and atypical mortality are all characteristics of adult asthma [27]. The longevity of asthma symptoms, medication use, lung function, low socioeconomic status, racial/ethnic minorities, and a neutrophilic phenotype have all been linked to the severity of childhood asthma. Increased IgE, elevated FeNO, eosinophilia, obesity, smoking, and low socioeconomic status have all been linked to adult asthma severity [28]. Despite higher prebronchodilator FEV1/FVC, adult-onset illness is related to more respiratory symptoms and asthma medication use [28]. Adult-onset asthma is less quiescent and appears to be more stable than childhood-onset asthma, with more relapses and fewer remissions. These characteristics reflect the complexity of asthma and the various elements involved in its pathophysiology.
A layer of regulation by miRNA adds to the regulatory network governing genetics, epigenetics, protein synthesis, and immune response in asthma. miRNAs are short non-coding RNAs that regulate gene expression by binding to target messenger RNAs and causing mRNA degradation or translational repression [29]. miRNAs can also regulate epigenetic DNA modifications, while also being influenced by epigenetic modifications [20, 30]. miRNAs play broadly different roles based on their location in the organism: (1) extracellular miRNAs are found inside extracellular vesicles such as exosomes, macrovesicles, and apoptotic bodies, which may act as cell-to-cell or system-to-system messengers, and (2) intracellular miRNAs, which govern protein production internal to a cell [31]. Intracellular miRNAs govern a variety of cellular pathways, and because their expression varies by tissue and disease, they have been widely exploited as prognostic and diagnostic biomarkers for a variety of disorders, including viral infections, cancer, cardiovascular disease, and allergic diseases [32, 33]. Extracellular, or circulating miRNAs, have also been investigated as potential biomarkers as they are resistant to degradation and ubiquitination [34].
Childhood Asthma and miRNA
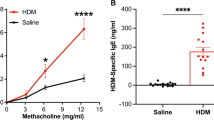
Allergic asthma may start as early as childhood, with up to 50% of adults reporting symptoms as children [35]. The composition of miRNAs in circulation and their potential as asthma biomarkers have been studied [17, 22••]. For instance, changes in miR-196a-2 expression and serum ANXA1 levels may play a role in asthma etiology. Furthermore, ANXA1 and miR-196a-2 could be used as diagnostic biomarkers for asthma and therapeutic targets in the future [36]. Wang et al. showed that deregulated miR-451a-ETS1 axis is a unique molecular mechanism responsible for pediatric asthma pathogenesis [37]. A study with CAMP data showed baseline FEV1/FVC and miR-221-5p were independent predictors of asthma remission by early adulthood [38]. Another study revealed reduced expression of miR-145-5p as a risk factor for early decline of long-term lung function growth leading to adult COPD in children with asthma and additionally increases airway smooth muscle cell proliferation [39]. A study showed that the aberrant expression of immune-related miRNAs (miR-146a and miR-106b) and inflammatory cytokines (IL-5 and IL-13) among asthmatic children led to their probable role in asthma pathogenesis [40]. Cancer-related long non-coding RNAs (lncRNA) were negatively correlated with miR-33a and miR-495 and positively with inflammatory cytokines in asthmatic children [41]. Another study on lncRNA showed that a lncRNA, RMRP, plays a pro-inflammatory and pro-fibrotic effect in pediatric asthma through targeting the miR-206/CCL2 axis [42]. Tiwari et al. investigated the association of circulating miRNAs from asthmatic children with seasonal variation in allergic inflammation and asthma symptoms and found that miR-328-3p and let-7d-3p expression varies seasonally and are significantly associated with seasonal asthma symptoms and seasonal allergies where let-7d-3p plays a potentially protective role and miR-328-3p has a deleterious role in asthmatic children sensitized to mulberry [43]. miR-15a is expressed during human lung development, is influenced by intrauterine smoke exposure, regulates the intrauterine expression of asthma genes, and is associated to asthma severity [44]. A study showed that baicalin regulates the onset of asthma in children by up-regulating miR-103 and modulating the TLR4/NF-B pathway [45]. After demonstrating that many miRNAs are altered in asthma, more research is needed to mechanistically characterize their role(s) in childhood asthma etiology (Table 1, Fig. 1).
Adult Asthma and miRNA
Numerous miRNAs have also been detected in adult asthma studies, which may help in better understanding the disease. One of the studies on RNA samples from eosinophils of individuals with atopic dermatitis, atopy, allergic rhinitis, and asthma identified 18 miRNAs (miR-1276, miR-29B2, miR-3175, miR-33B, miR-4308, miR-4523, miR-4673, miR-4785, miR-590, miR-638, miR-614, miR-142, miR-3064, miR-4434, miR-1304, miR-2355, miR-26A2, and miR-645) differentially expressed in eosinophil samples in cases of atopic dermatitis or asthma, or according to PC20 or IgE levels, compared to healthy samples [11]. According to a meta-analysis, the miR-499 rs3746444 (T > C) polymorphism is associated to asthma susceptibility, while the miR-146a rs2910164 (G > C) polymorphism is protective against asthma susceptibility [46]. A study found that c-kit + cells reduce asthma-related pathologies, likely through modulating miR-126 and miR-133 production [47]. miR-139 can decrease the inflammatory response of Th2 cells by down-regulating the Notch pathway and encouraging bone marrow-derived mesenchymal stem cells into asthmatic lung tissues [48] (Table 2).
Circulating and Exosome-Derived miRNAs
Even outside of the airways, miRNAs have showed promise as asthma predictors. Several studies with plasma samples of asthmatic patients have been undertaken to identify dysregulated miRNAs. A study identified miR-19b-3p and miR-320c significantly dysregulated in moderate asthmatic patients in comparison with control group and showed a positive correlation between the expression level of miR-320c and IL-4 levels [49]. Under the influence of vitamin D treatment, a plasma circulating miRNA, miR-574-5p, was discovered to be related with and predictive of asthma [50]. It has been reported that plasma circulating miR-223 and miR-21 had a diagnosis estimation probability of 83 and 76% in moderate asthmatic patients, respectively, and could be employed as biomarkers or for targeted immunotherapies in asthma [51]. It has been shown that plasma miR-206, IL-4, IL-13, and INF-γ has potential significance for prognosis of asthma-induced pulmonary arterial hypertension [52]. It is intriguing to suggest that plasma miR-122-5p can differentiate different subtypes of asthma, such as neutrophilic versus eosinophilic asthma, given its IPA-predicted role in lymphocyte differentiation and function [53]. Plasma miR-206, IL-4, IL-13, and INF-γ have been found to have potential prognostic value in asthma-induced pulmonary arterial hypertension [52].
Recently, miRNAs were utilized to identify asthma subgroups in serum; investigations reported that miR‐28‐3p, miR‐16‐2‐3p, miR‐210‐3p, miR-185, miR-125b, miR-338-3p, and miR-125b were associated with severe asthma [54,55,56]. Another study found that miR-3934 levels in PBMCs and serum can distinguish asthma patients from controls, particularly severe asthma patients, and that miR-3934 levels in PBMCs were negatively correlated with serum levels of IL-6, IL-8, and IL-33 in asthma patients, respectively [57]. Several biomarker studies have been undertaken to identify extracellular vesicle-derived miRNAs from bronchoalveolar lavage (BAL) as well as cell-specific miRNAs that are dysregulated in asthma. By comparing serum expression levels in asthmatic patients to those in healthy controls and associating their levels with serum IL-4, one study found that miR-21 and miR-155 are promising non-invasive biomarkers in the diagnosis of eosinophilic asthma and its response to therapy [58]. Another study identified miR-1246, miR-5100, and miR-338-3p as biomarkers for predicting the response to the biological drug benralizumab [59]. One study evaluated the effect of aging on serum miRNA expression in asthmatics and found that serum miRNA (miR-146a, miR-126a, miR-106a, and miR-19b) expression correlates with clinical characteristics of asthma and systemic inflammation in an age-dependent manner, implying that miRNA may contribute to asthma pathogenesis differently in elderly and non-elderly patients [60].
Recent in-depth investigations have revealed possible links between miRNA gene targets and asthma pathology, implying that numerous signaling systems could be involved. It is reported that miR-20a-5p targets ATG7-regulated cell death, fibrosis, and inflammation in an ovalbumin (OVA)–induced mouse model of allergic asthma [61]. Another study found that the miR-106b-5p/E2F1/SIX1 signaling pathway could be used to develop asthma therapies [62]. It has been reported that borneol reduces asthma symptoms by inhibiting CD4+ T-cell proliferation by down-regulating miR-26a and miR-142-3p [63]. In asthma, up-regulation of miR-92a in the serum leads to the blocking of goblet cell metaplasia by targeting MUC5AC [64]. Still, there is a need to study more miRNA and its target genes for better understanding the asthma pathogenesis.
The exosome plays an important role in chronic asthma. The DDAH1/Wnt/-catenin signaling pathway enhances oxidative stress and inflammatory responses in asthmatic mice via miR-21 secreted by mast cell–derived extracellular vesicles [65]. miR-21-5p in macrophage-derived exosomes targets Smad7 in airway epithelial cells to promote epithelial mesenchymal transition [66]. Exosomes generated from M2 macrophages carry miR-370, which slows asthma progression by inhibiting FGF1 production and the MAPK/STAT1 signaling pathway [67].
Thus, circulating miRNAs have showed potential as non-invasive biomarkers and asthma etiology predictors.
Asthmatic Airways and Airway Remodeling
Asthma has been associated to airway remodeling, which is a change in the fundamental architecture of the airway walls. These structural changes are characterized by epithelial goblet cell hyperplasia and metaplasia, an increase in bronchial smooth muscles and new blood vessels, and interstitial collagen deposition that extends beyond the thickened lamina reticularis to involve the entire inner airway wall in proportion to disease severity [68]. Several studies were conducted to examine the expression and role of miRNA in airway remodeling. One of the studies showed a role for miR-620 in promoting TGF-β1-induced proliferation of airway smooth muscle cell through controlling PTEN/AKT signaling pathway [69]. The investigators reconstructed circular-RNA-miRNA-mRNA regulatory network using miRNA and mRNA expression data of bronchial brushing samples from asthma patients and healthy patients. Downstream analysis identified the top 10 epithelial RNAs: hsa_circ_0001585, hsa_circ_0078031, hsa_circ_0000552, miR-30a-3p, miR-30d-3p, KIT, CD69, ADRA2A, BPIFA1, and GGH, demonstrating the utility of the epithelial circRNA-miRNA-mRNA network in understanding the pathogenesis of asthma [70]. miR-21 dysregulation in the circulation and airways has been widely observed in allergic asthma and extensively investigated in humans and mice [71, 72]. According to studies, in an ovalbumin-induced allergic asthma mice model, miR-21 inhibition suppresses alveolar M2 macrophages [71], and in human bronchial smooth muscle cells, the miR-21-transforming growth factor 1-Smad7 axis controls the pathogenesis of ovalbumin-induced chronic asthma [72]. According to a study, TUG1 reinforces HMGB1 expression by sequestering miR-181b, which activates the NF-B signaling pathway and promotes airway remodeling in asthmatic mice [73]. An in vitro investigation showed that miR-30b-5p targets phosphatase and tensin homolog deleted on chromosome ten (PTEN) and stimulates the proliferation and migration of human airway smooth muscle cells triggered by platelet-derived growth factor [74]. According to a study, reduced A-to-I editing of miR-200b-3p position 5 in lower airway cells from moderate-to-severe asthmatic individuals may lead to overexpression of SOCS1 and defective cytokine signaling [75]. Interlukin-13-dependent RhoA protein expression is negatively controlled by miR-140-3p in ASMs, according to a study, and the RhoA/Rho-kinase pathway has been suggested as a new target for the therapy of AHR in asthma [76, 77]. miR-149 inhibits TGF-1-induced airway smooth muscle cell proliferation and migration via targeting TRPM7 and altering the downstream MAPK signal pathway [78]. miR-135a reduces asthmatic mice’s airway inflammatory response through modulating the JAK/STAT signaling pathway [79]. Pulmonary macrophage polarization and asthma airway remodeling are regulated by miR-142-5p and miR-130a-3p [80]. By regulating the transforming growth factor-Smad7 pathway, miR-21 inhibition reduces airway inflammation and remodeling [72]. In nicotine-induced airway remodeling, miR-98 suppresses nerve growth factor expression [81].
PRMT1 was found to be a coactivator for STAT1 or RUNX1, which is required for the transcription of pri-let-7i and pri-miR-423 in epithelial cells and could be linked to asthmatic epithelial dysfunction [82]. By targeting miR-143-3p via HMGB1, OIP5AS1 increased Der p1-induced inflammation and apoptosis in BEAS2B cells [83]. TNF receptor-associated factor 6 is targeted by miR-146a-5p, which reduces the inflammatory response and damage of airway epithelial cells [84]. The CD39–extracellular ATP axis, which represents a potentially unique therapeutic target in type 2–high asthma, is targeted by epithelial miR-206, which up-regulates airway IL-25 and TSLP expression [85]. A study discovered that miR-141-3p governs pathological airway mucus production, and in T2-high asthma, miR-141-3p and/or its mRNA targets could be useful therapeutic targets [86]. Airway smooth muscle cell (ASMC) regulation is strongly influenced by epigenetic processes. By modulating miR-149, the lncRNA PVT1 exacerbates asthmatic inflammation and cell-barrier damage [87]. The PVT1-miR-15a-5p/miR-29c-3p-PI3K-Akt-mTOR lncRNA axis has been associated with the development of ozone-induced asthma by stimulating ASMC proliferation and a Th1/Th2 imbalance [88]. Furthermore, another study showed that lncRNA TUG1 facilitates Th2 cell differentiation on macrophages by targeting the miR-29c/B7-H3 axis [89]. The increase of CD38 protein in ASMC of asthmatic patients may be caused by the down-regulation of miR-140-3p produced by IL-13 [76]. Another study found that the miR-375/Krüppel-like factor 4 (KLF4) axis contributes to IL-13-induced inflammatory cytokine and mucus production in nasal epithelial cells (NECs) via circARRDC3 [90] (Table 3).
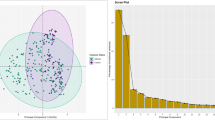
Together, emerging data indicate that the miRNAs play a crucial role in asthmatic airways and airway remodeling, performing an integral role in post-transcriptional regulation within the complex biological network (Tables 2 and 3; Fig. 2).
Asthma–COPD Overlap Syndrome
Recently, several studies were conducted to identify miRNAs as biomarkers for distinguishing patients with ACOS (asthma–COPD overlap syndrome) from patients with COPD or asthma. Hirai et al. proposed miR-15b-5p as a potential marker for identifying patients with ACOS. When miR-15b-5p, serum periostin, and YKL-40 were combined, it can improve diagnosis accuracy for ACOS (AUROC, 0.80) [91]. Another study depicted free-circulating miR-19b-3p, miR-125b-5p, and miR-320c in the blood plasma as three potential biomarkers for the diagnosis of COPD, bronchial asthma, and ACOS [92]. The collected literature reflects potential use of miRNAs as a tool for distinguishing these three very similar diseases: COPD, asthma, and ACOS.
miRNA and Virus-Induced Exacerbations in Asthma
Human respiratory virus (RV), human respiratory syncytial virus (RSV), and influenza viruses are all common viruses that attack the respiratory system. These viruses are known to induce illness and exacerbations in asthmatics [93]. The study found that suppressing STIM1 alleviated influenza A virus (IAV)–induced lung epithelial cell inflammation by inactivating NLRP3 (NLR Family Pyrin Domain Containing 3) and the inflammasome and increasing miR-223 expression. These findings may aid researchers to better understand the mechanism of influenza A virus (IAV)–induced lung injury and aid in IAV infection treatment [94]. The induction of MUC5AC synthesis by reduced miR-34b/c-5p was partly mediated by activation of c-Jun in RSV-infected HBECs. These findings shed light on the mechanism of mucus obstruction following RSV infection and point to potential therapeutic targets for RSV infection and airway obstruction [95]. In vivo, miR-122 enhances RV-induced asthma by suppressing its target SOCS1 [96]. In addition, influenza virus induces miR-146a. By directly targeting the tumor necrosis factor receptor association factor 6 (TRAF6), infection and down-regulation of miR-146a have been demonstrated to decrease influenza A virus multiplication by increasing IFN type 1 responses [97]. These findings point to miRNA modulation of immune responses to respiratory viruses (Fig. 3), and it is tempting to believe that miRNAs that alter virus replication play a key role in asthma exacerbations caused by viruses (Table 4).
Conclusion
It is difficult to accurately compare childhood and adult-onset asthma due to existing gaps in the literature and we acknowledge this limitation. In addition, because some findings are reported more in adults, this does not necessarily mean they are more prevalent, but rather a possible manifestation of publication bias. In this review, we tried to group the miRNAs from recent publications broadly into adult and childhood asthma and further sub-categorized into exosome derived, plasma/serum, ACOs, and role of miRNA in virus-induced exacerbations in asthma.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Tarlo SM, Balmes J, Balkissoon R, Beach J, Beckett W, Bernstein D, et al. Diagnosis and management of work-related asthma: American College of Chest Physicians Consensus Statement. Chest. 2008;134(3 Suppl):1S-41S.
GAN. The Global Asthma Report. Vol. 9, Policy Studies. Auckland, New Zealand; 2018.
Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald JM, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008;31(1):143–78.
Eder W, Ege MJ, von Mutius E. The asthma epidemic. N Engl J Med. 2006;355(21):2226–35.
Ivanova O, Richards LB, Vijverberg SJ, Neerincx AH, Sinha A, Sterk PJ, et al. What did we learn from multiple omics studies in asthma? Allergy [Internet]. 2019;74(11):2129–45. Available from: https://doi.org/10.1111/all.13833.
Gautam Y, Johansson E, Mersha TB. Multi-Omics Profiling Approach to Asthma: An Evolving Paradigm. J Pers Med. 2022 Jan 7;12(1):66. https://doi.org/10.3390/jpm12010066.
Kim VN, Han J, Siomi MC. Biogenesis of small RNAs in animals. Nat Rev Mol Cell Biol. 2009;10(2):126–39.
Hoefel G, Tay H, Foster P. MicroRNAs in lung diseases. Chest. 2019 Nov;156(5):991–1000. https://doi.org/10.1016/j.chest.2019.06.008. Epub 2019 Jun 27.
Ardekani AM, Naeini MM. The role of MicroRNAs in human diseases. Avicenna J Med Biotechnol. 2010;2(4):161–79.
Cañas JA, Rodrigo-Muñoz JM, Gil-Martínez M, Sastre B, del Pozo V. Exosomes: a key piece in asthmatic inflammation. Int J Mol Sci. 2021;22(2):963.
Bélanger É, Madore A-M, Boucher-Lafleur A-M, Simon M-M, Kwan T, Pastinen T, et al. Eosinophil microRNAs play a regulatory role in allergic diseases included in the atopic march. Int J Mol Sci. 2020;21(23):9011.
Tan BWQ, Sim WL, Cheong JK, Kuan WS, Tran T, Lim HF. MicroRNAs in chronic airway diseases: clinical correlation and translational applications. Pharmacol Res. 2020;160:105045.
Usman K, Hsieh A, Hackett T-L. The role of miRNAs in extracellular matrix repair and chronic fibrotic lung diseases. Cells. 2021;10(7):1706.
Adcock IM, Mumby S. MicroRNAs in human disease: commentary. Iran J Allergy Asthma Immunol. 2021;20(3):259–62.
Alashkar Alhamwe B, Potaczek DP, Miethe S, Alhamdan F, Hintz L, Magomedov A, et al. Extracellular vesicles and asthma-more than just a co-existence. Int J Mol Sci. 2021;22(9):4984.
Cañas JA, Rodrigo-Muñoz JM, Sastre B, Gil-Martinez M, Redondo N, Del Pozo V. MicroRNAs as potential regulators of immune response networks in asthma and chronic obstructive pulmonary disease. Front Immunol. 2020;11:608666.
Paul S, Ruiz-Manriquez LM, Ledesma-Pacheco SJ, Benavides-Aguilar JA, Torres-Copado A, Morales-Rodríguez JI, et al. Roles of microRNAs in chronic pediatric diseases and their use as potential biomarkers: a review. Arch Biochem Biophys. 2021;699:108763.
Akbari Dilmaghnai N, Shoorei H, Sharifi G, Mohaqiq M, Majidpoor J, Dinger ME, et al. Non-coding RNAs modulate function of extracellular matrix proteins. Biomed Pharmacother. 2021;136:111240.
•• Calvén J, Ax E, Rådinger M. The airway epithelium–a central player in asthma pathogenesis. Int J Mol Sci. 2020;21(23):8907. Describes the miRNAs associated with virus induced asthma and role of airway epithelium.
Benincasa G, DeMeo DL, Glass K, Silverman EK, Napoli C. Epigenetics and pulmonary diseases in the horizon of precision medicine: a review. Eur Respir J. 2021;57(6):2003406.
Shastri MD, Chong WC, Dua K, Peterson GM, Patel RP, Mahmood MQ, et al. Emerging concepts and directed therapeutics for the management of asthma: regulating the regulators. Inflammopharmacology. 2021;29(1):15–33.
•• Weidner J, Bartel S, Kılıç A, Zissler UM, Renz H, Schwarze J, et al. Spotlight on microRNAs in allergy and asthma. Allergy. 2021;76(6):1661–78. COMMENT: A good collection of miRNAs associated with Asthma.
Alashkar Alhamwe B, Miethe S, von Strandmann E, Potaczek DP, Garn H. Epigenetic regulation of airway epithelium immune functions in asthma. Front Immunol. 2020;11:1747.
Ghafouri-Fard S, Shoorei H, Taheri M, Sanak M. Emerging role of non-coding RNAs in allergic disorders. Biomed Pharmacother. 2020;130:110615.
Casciaro M, Di Salvo E, Pioggia G, Gangemi S. Microbiota and microRNAs in lung diseases: mutual influence and role insights. Eur Rev Med Pharmacol Sci. 2020;24(24):13000–8.
Kuruvilla ME, Lee FE-H, Lee GB. Understanding asthma phenotypes, endotypes, and mechanisms of disease. Clin Rev Allergy Immunol. 2019;56(2):219–33.
Trivedi M, Denton E. Asthma in children and adults—what are the differences and what can they tell us about asthma? Front Pediatr. 2019 Jun 25;7:256. https://doi.org/10.3389/fped.2019.00256.
Sood A, Qualls C, Schuyler M, Arynchyn A, Alvarado JH, Smith LJ, et al. Adult-onset asthma becomes the dominant phenotype among women by age 40 years. The longitudinal CARDIA study. Ann Am Thorac Soc. 2013 Jun;10(3):188–97. https://doi.org/10.1513/AnnalsATS.201212-115OC.
O’Brien J, Hayder H, Zayed Y, Peng C. Overview of MicroRNA biogenesis, mechanisms of actions, and circulation. Front Endocrinol (Lausanne) [Internet]. 2018;9. Available from: https://doi.org/10.3389/fendo.2018.00402.
Liu X, Chen X, Yu X, Tao Y, Bode AM, Dong Z, et al. Regulation of microRNAs by epigenetics and their interplay involved in cancer. J Exp Clin Cancer Res [Internet]. 2013;32(1):96. Available from: https://doi.org/10.1186/1756-9966-32-96.
Rodrigo-Muñoz JM, Cañas JA, Sastre B, Rego N, Greif G, Rial M, et al. Asthma diagnosis using integrated analysis of eosinophil microRNAs. Allergy. 2019;74(3):507–17.
Taka S, Tzani-Tzanopoulou P, Wanstall H, Papadopoulos NG. MicroRNAs in asthma and respiratory infections: identifying common pathways. Allergy Asthma Immunol Res. 2020;12(1):4–23.
Wang J, Chen J, Sen S. MicroRNA as biomarkers and diagnostics. J Cell Physiol. 2016;231(1):25–30.
Mori MA, Ludwig RG, Garcia-Martin R, Brandão BB, Kahn CR. Extracellular miRNAs: from biomarkers to mediators of physiology and disease. Cell Metab [Internet]. 2019/08/22. 2019;30(4):656–73. Available from: https://pubmed.ncbi.nlm.nih.gov/31447320.
Simpson CR, Sheikh A. Trends in the epidemiology of asthma in England: a national study of 333,294 patients. J R Soc Med. 2010 Mar;103(3):98–106. https://doi.org/10.1258/jrsm.2009.090348.
Ibrahim AA, Ramadan A, Wahby AA, Draz IH, El Baroudy NR, Abdel Hamid TA. Evaluation of miR-196a2 expression and Annexin A1 level in children with bronchial asthmaEvaluation of miR-196a2 expression and Annexin A1 level in children. Allergol Immunopathol (Madr). 2020;48(5):458–64.
Wang T, Zhou Q, Shang Y. Downregulation of miRNA-451a promotes the differentiation of CD4+ T cells towards Th2 cells by upregulating ETS1 in childhood asthma. J Innate Immun. 2021;13(1):38–48.
Wang AL, Li J, Kho AT, McGeachie MJ, Tantisira KG. Enhancing the prediction of childhood asthma remission: integrating clinical factors with microRNAs. J Allergy Clin Immunol. 2021;147(3):1093-1095.e1.
Tiwari A, Li J, Kho AT, Sun M, Lu Q, Weiss ST, et al. COPD-associated miR-145-5p is downregulated in early-decline FEV1 trajectories in childhood asthma. J Allergy Clin Immunol. 2021;147(6):2181–90.
Elnady HG, Sherif LS, Kholoussi NM, Ali Azzam M, Foda AR, Helwa I, et al. Aberrant expression of immune-related MicroRNAs in pediatric patients with asthma. Int J Mol Cell Med. 2020;9(4):246–55.
Li W, Wang X, Sun S, An H. Long non-coding RNA colorectal neoplasia differentially expressed correlates negatively with miR-33a and miR-495 and positively with inflammatory cytokines in asthmatic children. Clin Respir J. 2021;15(11):1175–84.
Yin H, Liu MH, Gao F, Shang HM. Pro-inflammatory and pro-fibrotic role of long non-coding RNA RMRP in pediatric asthma through targeting microRNA-206/CCL2 axis. J Biol Regul Homeost Agents. 2021;35(1):71–83.
Tiwari A, Wang AL, Li J, Lutz SM, Kho AT, Weiss ST, et al. Seasonal variation in miR-328-3p and let-7d-3p are associated with seasonal allergies and asthma symptoms in children. Allergy Asthma Immunol Res. 2021;13(4):576–88.
Sharma S, Kho AT, Chhabra D, Haley K, Vyhlidal C, Gaedigk R, et al. Effect of intrauterine smoke exposure on microRNA-15a expression in human lung development and subsequent asthma risk. Healthc. 2020;8(4):536.
Zhai C, Wang D. Baicalin regulates the development of pediatric asthma via upregulating microRNA-103 and mediating the TLR4/NF-κB pathway. J Recept Signal Transduct Res. 2021;1–11.
Dong J, Sun D, Lu F. Association of two polymorphisms of miRNA-146a rs2910164 (G > C) and miRNA-499 rs3746444 (T > C) with asthma: a meta-analysis. J Asthma. 2021;58(8):995–1002.
Rahbarghazi R, Keyhanmanesh R, Rezaie J, Mirershadi F, Heiran H, Saghaei Bagheri H, et al. c-kit+ cells offer hopes in ameliorating asthmatic pathologies via regulation of miRNA-133 and miRNA-126. Iran J Basic Med Sci. 2021;24(3):369–76.
Wang K, Zhu H, Yang L, Xu Q, Ren F. miR-139 promotes homing of bone marrow mesenchymal stem cells (BMSCs) to lung tissues of asthmatic rats to inhibit inflammatory response of Th2 cells by down-regulating Notch1/Hes1 pathway. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2021;37(2):97–104.
Aripova A, Akparova A, Bersimbaev R. Moderate bronchial asthma. MicroRNA. 2020;9(5):373–7.
Li J, Tiwari A, Mirzakhani H, Wang AL, Kho AT, McGeachie MJ, et al. Circulating MicroRNA: incident asthma prediction and vitamin D effect modification. J Pers Med. 2021;11(4):307.
Rostami Hir S, Alizadeh Z, Mazinani M, Mahlooji Rad M, Fazlollahi MR, Kazemnejad A, et al. Exosomal MicroRNAs as biomarkers in allergic asthma. Iran J Allergy Asthma Immunol. 2021;20(2):160–8.
Li S, Ma X, Xie J, Yan X, Sun W. MicroRNA-206, IL-4, IL-13, and INF-γ levels in lung tissue and plasma are increased by the stimulation of particulate matter with a diameter of ≤2.5μm, and are associated with the poor prognosis of asthma induced pulmonary arterial hypert. Clin Exp Hypertens. 2021;43(2):181–8.
Bahmer T, Krauss-Etschmann S, Buschmann D, Behrends J, Watz H, Kirsten A-M, et al. RNA-seq-based profiling of extracellular vesicles in plasma reveals a potential role of miR-122-5p in asthma. Allergy. 2021;76(1):366–71.
Kyyaly MA, Sanchez-Elsner T, He P, Sones CL, Arshad SH, Kurukulaaratchy RJ. Circulating miRNAs-A potential tool to identify severe asthma risk? Clin Transl Allergy. 2021;11(4):e12040.
Atashbasteh M, Mortaz E, Mahdaviani SA, Jamaati H, Allameh A. Expression levels of plasma exosomal miR-124, miR-125b, miR-133b, miR-130a and miR-125b-1-3p in severe asthma patients and normal individuals with emphasis on inflammatory factors. Allergy Asthma Clin Immunol. 2021;17(1):51.
Rial MJ, Cañas JA, Rodrigo-Muñoz JM, Valverde-Monge M, Sastre B, Sastre J, et al. Changes in serum MicroRNAs after anti-IL-5 biological treatment of severe asthma. Int J Mol Sci. 2021;22(7):3558.
Wang W, Wang J, Chen H, Zhang X, Han K. Downregulation of miR-3934 in peripheral blood mononuclear cells of asthmatic patients and its potential diagnostic value. Biomed Res Int. 2021;2021:8888280.
ElKashef SMMAE, Ahmad SEA, Soliman YMA, Mostafa MS. Role of microRNA-21 and microRNA-155 as biomarkers for bronchial asthma. Innate Immun. 2021;27(1):61–9.
Cañas JA, Valverde-Monge M, Rodrigo-Muñoz JM, Sastre B, Gil-Martínez M, García-Latorre R, et al. Serum microRNAs as tool to predict early response to benralizumab in severe eosinophilic asthma. J Pers Med. 2021;11(2):76.
Wardzyńska A, Pawełczyk M, Rywaniak J, Makowska J, Jamroz-Brzeska J, Kowalski ML. Circulating miRNA expression in asthmatics is age-related and associated with clinical asthma parameters, respiratory function and systemic inflammation. Respir Res. 2021;22(1):177.
Yu Y, Men S, Zhang Y. miR-20a-5p ameliorates ovalbumin (OVA)-induced mouse model of allergic asthma through targeting ATG7-regulated cell death, fibrosis and inflammation. Int Immunopharmacol. 2021;95:107342.
Liu S, Chen X, Zhang S, Wang X, Du X, Chen J, et al. miR-106b-5p targeting SIX1 inhibits TGF-β1-induced pulmonary fibrosis and epithelial-mesenchymal transition in asthma through regulation of E2F1. Int J Mol Med. 2021;47(3):1.
Wang J-Y, Dong X, Yu Z, Ge L, Lu L, Ding L, et al. Borneol inhibits CD4 + T cells proliferation by down-regulating miR-26a and miR-142-3p to attenuate asthma. Int Immunopharmacol. 2021;90:107223.
Dai J, Ma B, Wen X, Yang Z, Yue Y. Upregulation of miR-92a contributes to blocking goblet cell metaplasia by targeting MUC5AC in asthma. J Recept Signal Transduct Res. 2020;40(6):613–9.
Zou Y, Zhou Q, Zhang Y. MicroRNA-21 released from mast cells-derived extracellular vesicles drives asthma in mice by potentiating airway inflammation and oxidative stress. Am J Transl Res. 2021;13(7):7475–91.
Li X, Yang N, Cheng Q, Zhang H, Liu F, Shang Y. MiR-21-5p in macrophage-derived exosomes targets Smad7 to promote epithelial mesenchymal transition of airway epithelial cells. J Asthma Allergy. 2021;14:513–24.
Li C, Deng C, Zhou T, Hu J, Dai B, Yi F, et al. MicroRNA-370 carried by M2 macrophage-derived exosomes alleviates asthma progression through inhibiting the FGF1/MAPK/STAT1 axis. Int J Biol Sci. 2021;17(7):1795–807.
Hough KP, Curtiss ML, Blain TJ, Liu R-M, Trevor J, Deshane JS, et al. Airway remodeling in asthma. Front Med [Internet]. 2020;7. Available from: https://doi.org/10.3389/fmed.2020.00191.
Chen H, Guo S-X, Zhang S, Li X-D, Wang H, Li X-W. MiRNA-620 promotes TGF-β1-induced proliferation of airway smooth muscle cell through controlling PTEN/AKT signaling pathway. Kaohsiung J Med Sci. 2020;36(11):869–77.
Chen D, Wu W, Yi L, Feng Y, Chang C, Chen S, et al. A potential circRNA-miRNA-mRNA regulatory network in asthmatic airway epithelial cells identified by integrated analysis of microarray datasets. Front Mol Biosci. 2021;8:703307.
Lee HY, Hur J, Kang JY, Rhee CK, Lee SY. MicroRNA-21 inhibition suppresses alveolar M2 macrophages in an ovalbumin-induced allergic asthma mice model. Allergy Asthma Immunol Res. 2021;13(2):312–29.
Hur J, Rhee CK, Lee SY, Kim YK, Kang JY. MicroRNA-21 inhibition attenuates airway inflammation and remodelling by modulating the transforming growth factor β-Smad7 pathway. Korean J Intern Med. 2021;36(3):706–20.
Huang W, Yu C, Liang S, Wu H, Zhou Z, Liu A, et al. Long non-coding RNA TUG1 promotes airway remodeling and mucus production in asthmatic mice through the microRNA-181b/HMGB1 axis. Int Immunopharmacol. 2021;94:107488.
Wang W, Guo J, Wang Y. MicroRNA-30b-5p promotes the proliferation and migration of human airway smooth muscle cells induced by platelet-derived growth factor by targeting phosphatase and tensin homolog deleted on chromosome ten. Bioengineered. 2021;12(1):3662–73.
Magnaye KM, Naughton KA, Huffman J, Hogarth DK, Naureckas ET, White SR, et al. A-to-I editing of miR-200b-3p in airway cells is associated with moderate-to-severe asthma. Eur Respir J. 2021;58(1):2003862.
Chiba Y, Ando Y, Kato Y, Hanazaki M, Sakai H. Down-regulation of miR-140–3p is a cause of the interlukin-13-induced up-regulation of RhoA protein in bronchial smooth muscle cells. Small GTPases. 2021;1–6.
Chiba Y, Ando Y, Fujii S, Miyakawa Y, Suto W, Kamei J, et al. Downregulation of miR-140-3p is a cause of upregulation of RhoA protein in bronchial smooth muscle of murine experimental asthma. Am J Respir Cell Mol Biol. 2021;64(1):138–40.
Zhu Z, Zhang L, Jiang T, Qian Y, Sun Y, Zhang Q. MiR-149 attenuates the proliferation and migration of TGF-β1-induced airway smooth muscle cells by targeting TRPM7 and affecting downstream MAPK signal pathway. Acta Biochim Pol. 2020;67(4):453–60.
Huang X-P, Qin C-Y, Gao Y-M. miR-135a inhibits airway inflammatory response in asthmatic mice via regulating JAK/STAT signaling pathway. Braz J Med Biol Res. 2021;54(3):e10023.
Shi J, Chen M, Ouyang L, Wang Q, Guo Y, Huang L, et al. miR-142-5p and miR-130a-3p regulate pulmonary macrophage polarization and asthma airway remodeling. Immunol Cell Biol. 2020;98(9):715–25.
Wongtrakool C, Ko J, Jang AJ, Grooms K, Chang S, Sylber C, et al. MicroRNA-98 reduces nerve growth factor expression in nicotine-induced airway remodeling. J Biol Chem. 2020;295(52):18051–64.
Zhai W, Sun H, Li Z, Li L, Jin A, Li Y, et al. PRMT1 modulates processing of asthma-related primary MicroRNAs (pri-miRNAs) into mature miRNAs in lung epithelial cells. J Immunol. 2021;206(1):11–22.
Cai X-J, Huang L-H, Zhu Y-K, Huang Y-J. LncRNA OIP5-AS1 aggravates house dust mite-induced inflammatory responses in human bronchial epithelial cells via the miR-143-3p/HMGB1 axis. Mol Med Rep. 2020;22(6):4509–18.
Yan F, Wufuer D, Ding J, Wang J. MicroRNA miR-146a-5p inhibits the inflammatory response and injury of airway epithelial cells via targeting TNF receptor-associated factor 6. Bioengineered. 2021;12(1):1916–26.
Zhang K, Feng Y, Liang Y, Wu W, Chang C, Chen D, et al. Epithelial miR-206 targets CD39/extracellular ATP to upregulate airway IL-25 and TSLP in type 2-high asthma. JCI Insight. 2021;6(11).
Siddiqui S, Johansson K, Joo A, Bonser LR, Koh KD, Le Tonqueze O, et al. Epithelial miR-141 regulates IL-13-induced airway mucus production. JCI Insight. 2021;6(5).
Ma L, Zhang Q, Hao J, Wang J, Wang C. LncRNA PVT1 exacerbates the inflammation and cell-barrier injury during asthma by regulating miR-149. J Biochem Mol Toxicol. 2020;34(11):e22563.
Wei Y, Han B, Dai W, Guo S, Zhang C, Zhao L, et al. Exposure to ozone impacted Th1/Th2 imbalance of CD4+ T cells and apoptosis of ASMCs underlying asthmatic progression by activating lncRNA PVT1-miR-15a-5p/miR-29c-3p signaling. Aging (Albany NY). 2020;12(24):25229–55.
Sun H, Wang T, Zhang W, Dong H, Gu W, Huang L, et al. LncRNATUG1 facilitates Th2 cell differentiation by targeting the miR-29c/B7-H3 axis on macrophages. Front Immunol. 2021;12:631450.
Wang T, Wang P, Chen D, Xu Z, Yang L. circARRDC3 contributes to interleukin-13-induced inflammatory cytokine and mucus production in nasal epithelial cells via the miR-375/KLF4 axis. Mol Med Rep. 2021;23(2):1.
Hirai K, Shirai T, Shimoshikiryo T, Ueda M, Gon Y, Maruoka S, et al. Circulating microRNA-15b-5p as a biomarker for asthma-COPD overlap. Allergy. 2021;76(3):766–74.
Bersimbaev R, Aripova A, Bulgakova O, Kussainova A, Akparova A, Izzotti A. The plasma levels of hsa-miR-19b-3p, hsa-miR-125b-5p, and hsamiR- 320c in patients with asthma, COPD and Asthma-COPD Overlap Syndrome (ACOS). MicroRNA. 2021;10(2):130–8.
Jartti T, Bønnelykke K, Elenius V, Feleszko W. Role of viruses in asthma. Semin Immunopathol. 2020;42(1):61–74.
Liu C-C, Miao Y, Chen R-L, Zhang Y-Q, Wu H, Yang S-M, et al. STIM1 mediates IAV-induced inflammation of lung epithelial cells by regulating NLRP3 and inflammasome activation via targeting miR-223. Life Sci. 2021;266:118845.
Du X, Yang Y, Xiao G, Yang M, Yuan L, Qin L, et al. Respiratory syncytial virus infection-induced mucus secretion by down-regulation of miR-34b/c-5p expression in airway epithelial cells. J Cell Mol Med. 2020;24(21):12694–705.
Collison AM, Sokulsky LA, Kepreotes E, de Siqueira A, Morten M, Edwards MR, et al. miR-122 promotes virus-induced lung disease by targeting SOCS1. JCI Insight. 2021;6(7).
Laanesoo A, Urgard E, Periyasamy K, Laan M, Bochkov YA, Aab A, et al. Dual role of the miR-146 family in rhinovirus-induced airway inflammation and allergic asthma exacerbation. Clin Transl Med. 2021;11(6):e427.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rinku Sharma, Anshul Tiwari, and Michael J. McGeachie declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Asthma
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.