Abstract
Introduction
Air pollution poses a risk for people with Chronic Obstructive Pulmonary Disease (COPD). This study estimated the short-term effect of variations in air pollutant concentrations on exacerbations of COPD (COPD-E) in Bogotá, Colombia.
Methods
We performed an ecological time series study from 2014 to 2021 to evaluate the short-term effect of fine particulate matter (PM2.5), nitrogen dioxide (NO2), and ozone (O3) levels on COPD-E treated in the emergency and hospitalization services. Daily counts of patients with COPD-E discharge diagnoses were obtained from the National Health Information System, and daily measurements of PM2.5, NO2, and O3 concentrations and meteorological data were obtained from air monitoring stations. A Generalized Additive Model was used with Distributed Lag Non-Linear Models to control for confounders.
Results
An increase of 10 μg/m3 in PM2.5 and O3 was associated with increased COPD-E admissions (lagged 0-3 days) with Relative Risk (RR) of 1.04 (95%CI: 1.02 -1.07) and RR:1.03 (95%CI:1.01 – 1.04), respectively. During the rainy season and minimum temperature of the series, for every 10 μg/m3 increase in PM2.5 concentration, COPD-E admissions (lagged 0-3 days) increased with RR 1.03 (95%CI: 1.01-1.06). A higher magnitude of association was observed in men (PM2.5, 1.04 95%CI:1.01 – 1.06 and O3, 1.04 95%CI:1.02 – 1.05, lag 0-7 days) than in women.
Conclusions
A higher air pollution was associated with more COPD-E. These results highlight the importance of actions aimed at improving air quality.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Air Pollution continues to be a global public health and environmental problem (Dominski et al. 2021). It is one of the significant health risk factors, to which 5.15 to 2.35 Years of Life Lost were attributed between 1990 and 2019 worldwide (Abbafati et al. 2020; Bălă et al. 2021). Outdoor air pollution due to 2.5-micron particulate matter (PM2.5) was responsible for 4.14 million deaths (118 Million Years of Life Lost), and O3 was responsible for 365,000 premature deaths (6.21 Million Potential Years of Life Lost). Both air pollutants were responsible for 1 in 9 deaths worldwide in 2019 (Health Effects Institute and Institute for Health Metrics and Evaluation’s Global Burden of Desease project 2020). For the same year, 18% of premature deaths in patients with chronic obstructive pulmonary disease (COPD) were due to air pollution (World Health Organization WHO 2022; Soriano et al. 2020).
Air quality in low- and middle-income countries has deteriorated with accelerating urbanization, the development of fossil-fuel-based economies, disparities in exposure to air pollution, and the use of solid fuels, mainly biomass, for cooking and domestic heating (World Health Organization WHO 2021; Stoner et al. 2021). Similarly, as a result of aging populations and changing lifestyles, the prevalence of chronic non-communicable diseases (NCDs) is increasing in these countries. The burden of morbidity and mortality from NCDs is therefore increased by poor air quality (World Health Organization WHO 2021).
COPD, a pathological disease characterized by airflow obstruction and respiratory symptoms, is characterized by the occurrence of COPD exacerbations (COPD-E), which are episodes of worsening symptoms that require additional treatment and adversely affect the prognosis and mortality of the disease (Gold Science Committee 2023; Celli et al. 2021; Soler-Cataluña and Lopez-Campos 2022). Causes of COPD-E are diverse and include bacterial and viral infections, exposure to tobacco and biomass smoke, poor adherence to treatment, other concomitant diseases, and COPD-E's history and severity (Gold Science Committee 2023; Lee et al. 2019).
Although there is no conclusive causal relationship, emerging evidence suggests that exposure to air pollution may also adversely affect COPD (Yan et al. 2019; Li et al. 2016). Increasing evidence links short-term air pollution with hospital admissions and emergency department visits for COPD-E (Yan et al. 2019; Hoffmann et al. 2022; Jin et al. 2022; Ross et al. 2023; Liu et al. 2022; Du et al. 2021; Tang et al. 2021; Dong et al. 2023; Ting et al. 2021). However, most epidemiological studies have been conducted in North America, Asia, and Europe, and there is little information on its association in Latin American countries, where it is recognized that the concentrations of air pollutants are generally higher than in North America and Europe. It is not possible to fully and accurately extrapolate the short-term effects of air pollution on COPD patients in Colombia from estimates of effects in high-income countries, given the heterogeneity in the levels and components of air pollutants (Health Effects Institute and Institute for Health Metrics and Evaluation’s Global Burden of Desease project 2020).
A previous study in Colombia by Morantes and Fajardo showed that high concentrations of PM2.5 and PM10 with a lag time of 48 hours in hospitalized patients were associated with increased sputum volume (OR: 4. 74; 95%CI: 1.02-21.90), purulence (OR: 6.58; 95%CI: 2.51-17.20), pleuritic pain (OR: 3.62; 95%CI: 1.27-10.37), use of antibiotics (OR: 2.87; 95%CI: 1.17-7.07) and corticosteroids (OR: 2.62; 95%CI: 1.07-6.44) (Morantes-Caballero and Fajardo Rodriguez 2019). However, this study was only an assessment of COPD symptoms. Therefore, it is essential to approach the question from the perspective of healthcare utilization and more severe clinical outcomes, as assessing emergency department admissions and hospitalizations for COPD is relevant.
As seen in the GOLD 2022 definition of COPD (Gold Science Committee 2022) there is a paradigm shift in the taxonomy of COPD, as it is now recognized that it may be caused by non-infectious risk factors, such as poor outdoor or indoor air quality (Roque et al. 2023; Stolz et al. 2022), that may play a clinically relevant role for the disease. Documentation and understanding of the relationship between COPD-E and pollutant levels is crucial because it may increase COPD patients' survival and quality of life and reduce healthcare costs and disease burden. In addition, reducing exacerbations is one of the most essential treatment targets in COPD from a clinical and economic perspective (Gold Science Committee 2023; Hoogendoorn et al. 2017)
Bogotá is a megacity in Latin America that has experienced high levels of air pollution during the last decades. However, there is little information on the relationship between outdoor air pollution and COPD-E and its behavior among the inhabitants of this high-altitude city. This study aimed to determine the short-term effect of variations in air pollutants on COPD-E between 2014 and 2021 in Bogotá, Colombia, hypothesizing that at least one pollutant is associated with emergency care and hospitalizations for COPD-E.
Methods
Study design and location
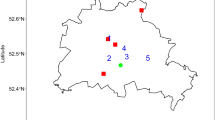
A retrospective ecological time series study was conducted between 1 January 2014 and 31 December 2021 in Bogotá, Colombia. The city is located in the central zone between 4°35'56"north latitude and 74°04'51" east longitude, with an altitude of 2,582 m asl, classified as high altitude (≥2,500 m) (Figure S1).
Data sources
Health Data
Daily counts were obtained from emergency and hospital admissions with a primary discharge diagnosis of COPD-E (ICD-10 J44.1, J440). Daily counts were also obtained from visits for other acute lower respiratory tract infections (ICD-10 J20-J22) and other acute upper respiratory tract infections (ICD-10 J30-J39). Data were obtained from the Social Protection Information System (Sistema de Information de la Protection Social - SISPRO) in the Individual Service Delivery Records (Registers Individuals de Prestation de Services - RIPS) module of the Ministry of Health and Social Protection (Ministerio de Salud y Protección Social) (Ministerio de Salud y ProtecciónSocial 2022). Daily counts of confirmed COVID-19 cases were obtained from the public database available on the National Health Institute website (Instituto Nacional de Salud - INS).
Pollutants and meteorological data
Hourly data on the city's daily concentrations of PM2.5, NO2, and O3, as well as meteorological variables, were obtained from the Bogotá Air Quality Monitoring Network (Red de Monitoreo de Calidad de Aire de Bogotá - RMCAB). This network consists of 20 air quality monitoring stations (Figure S1). The District Environment Office (Secretaría Distrital del Ambiente) provided data for the period studied. The 24-hour average was calculated for PM2.5 and NO2, and the maximum of the 8-hour moving average for O3. Estimates were obtained from temporal representativeness greater than or equal to 75% of the hourly record for each pollutant.
The study was approved by the Ethics Committee of the National School of Public Health of the University of Antioquia (Comité de Ética de la Facultad Nacional de Salud Pública de la Universidad de Antioquia) (CEI- 21030002-00162). Informed consent was waived according to international standards (CIOMS, OMS 2017).
Statistical analysis
The trend, seasonality, pollutant variation, and the Spearman correlation between pollutants, meteorological variables, and daily counts of COPD-E patients were described. Time series regression analysis was performed to evaluate the relationship between daily counts of people treated for COPD-E and daily average concentrations for each pollutant, adjusted for meteorological variables, dry and rainy weather periods, holidays, COVID-19 cases, days of mandatory isolation, and daily counts of people treated for upper and lower respiratory tract infections. Generalized Additive Models (GAMs) with quasi-Poisson distribution and non-linear distributed lag were used (Gasparrini and Armstrong 2011a; Gasparrini and Armstrong 2011b). In this case, the effect of pollutants was assumed to be linear, while the relationship with meteorological variables was modeled by a natural cubic spline with 5 degrees of freedom. The time series model was built assuming an over disperse Poisson distribution, including a time function with 4 degrees of freedom (df)/year (to correct for seasonality and long-term trend) and day of week as a factor. Sensitivity analyses were performed by varying the degrees of freedom between 4 and 8. To assess the lagged effect of pollutant variations on COPED-E (Li et al. 2022) we developed models with different lagged structures including lagged effects up to 15 days (lag 0-3, lag 0-7 and lag 0-15). We used the following model specification:
Where Yt represents the number of people with COPD-E on day t, "intercept" is the intercept of the model; "CB (crossbasis) air pollutant" is a two-dimensional spatial function in which the relationships of COPD-E concentrations and COPD-E lag are combined, assuming a linear and polynomial function, respectively. Meteorological variables of ns (temperature), ns (precipitation), ns (humidity), and ns (solar radiation) were included as covariates in the multivariate model with natural cubic smoothing functions (natural splines-ns) to control for non-linear confounding effects of the trends of the meteorological variables included in the model with 5 degrees of freedom. The smoothing allows maximum likelihood estimation.
In order to control for short-term weekly variations and seasonal trends, the day of the week ("Dow") and public holiday ("Holiday"). Other covariates considered in the model were COVID-19 cases, and other lower (ICD10- J20-J22) and upper (ICD10- J30-J39) respiratory tract infections.
Seasonal patterns were assessed using Dickey-Fuller, Kwiatkowski-Phillips-Schmidt-Shin (KPSS) tests and trends using a simple linear regression model and the KPSS test for trend. Autocorrelation was calculated for 15-day lags. A stratified analysis was performed for seasonality, temperature extremes (minimum and maximum daily temperature), and sex. Quasi Akaike's Information Criterion (QAIC) and Root Mean Squared Error (RMSE), R2, minimization of autocorrelation, and evaluation of residuals were used to select the best model, to identify deviations from model assumptions, and to generate a priori hypotheses based on the epidemiological literature. Results are presented as a relative risk of daily COPD-E per an increase of 10 μg/m3 PM2.5, NO2, and O3. Statistical tests were two-sided, and 95% confidence intervals were calculated for each estimated effect. R software version 4.3.1 (The R Foundation for Statistical Computing 2023) with the DLNM library (Gasparrini 2021) was used for statistical analyses.
Results
Air quality and admission to emergency and inpatient departments for COPD
Over the eight years (2,922 days), the daily average concentration of PM2.5 decreased by 43.15% (from 21.76 μg/m3 in 2014 to 15.20 μg/m3 in 2021), the concentration of NO2 decreased by 10.87% (from 31. 80 μg/m3 in 2014 to 28.68 μg/m3 in 2021), while the maximum 8 h moving average concentration of O3 increased by 12.77% (from 36.32 μg/m3 in 2014 to 41.64 μg/m3 in 2021) (Table 1). The daily pollutant averages were 18.43 ± 8.1 μg/m3 for PM2.5, 31.35 ± 10.1 μg/m3 for NO2, and 36.56 ± 15.27 μg/m3 for O3. The annual average concentrations of PM2.5 did not reach the annual intermediate objective of the World Health Organization (WHO 2005) guideline in force during the study period (10 μg/m3 for PM2.5), but they did for NO2 and O3. However, they did not reach the limit values set by the WHO for 2021 (5 μg/m3 for PM2.5, 10 μg/m3 for NO2 and O3 of 100 μg/m3). Meteorological variables showed variations, especially temperature and solar radiation, with means and standard deviations of 14.87 ± 0.77 °C and 178.33 ± 49.01 Wm2, respectively, over the period.
The correlation variables of the series showed seasonal behavior. The mean and variance of the time series were constant, and the Dickey-Fuller test (p-value=0.010) indicated rejection of the null hypothesis of non-stationarity. Therefore, a non-linear distributed lag model with a Poisson link (quasi-poisson) was constructed to model the COPD-E counts. The presence of increasing (O3) and decreasing (PM2.5 and NO2) trends in the behavior of the pollutants was confirmed (Figure S2, S3, and S4). The PM2.5, NO2, and O3 series showed a more pronounced seasonality than the meteorological variable series. The autocorrelation or serial correlation was positive for all three pollutants, and the risk estimates were higher for the lags in the first seven days (Figure S5).
In total, 37,968 people over 40 years of age were discharged from the emergency and hospitalization services with a diagnosis of COPD-E out of 46,373 admissions during the same period, for a ratio of 1.22 admissions to cases, with a maximum of 48 days in 2019 and a minimum of 20 in 2021. Although a decreasing trend was observed, this series showed three peaks (2014, 2018, and 2019) throughout the period analyzed. For 2014, the daily mean was 16.85 ± 6.10, of which 52.92% were female and 47.04% were male (Table 1).
The most positive and highest Spearman correlations were found between PM2.5 and NO2 (0.65); relative humidity and precipitation (0.57); O3 and maximum temperature (0.51) and PM2.5 and O3 (0.44); a positive correlation was found between COPD-E and PM2.5, NO2 and maximum temperature concentrations (0.12, 0.20, 0.09 respectively) and inverse correlation with pollutant O3 (-0.03) (Fig. 1).
Spearman correlation between criteria pollutants, meteorological variables, and patients admitted to the emergency and hospitalization services in Bogotá D.C. - Colombia, 2014 - 2021. NO2S: Nitrogen Dioxide in μg/m3. PM25S: Particulate matter in 2.5 μg/m3. TEMPS: Period mean temperature. RGLS: Solar radiation. PRECS: Precipitation. HRS: Relative humidity. Ozone: Ozone in μg/m3. pepocurghosp: Patients admitted to the emergency and hospitalization services. tempmin: Period average of minimum temperature. tempmax: Period average for maximum temperature
Association of air pollutants and admission to the emergency department and hospital for COPD-E
Figure 2 shows the Relative Risk (RR) and 95% confidence intervals (95%CI) for COPD-E for 10 μg/m3 increments of PM2.5 and O3 with lags from 0 to 15 days. The effects of the pollutants decreased after the seventh day and then increased after 14 days. The O3 effect was more significant on the same day than PM2.5, which was more significant at the 3-day lag. The effect of NO2 was null in the first three days and decreased from the fourth to the thirteenth day, showing an inverse proportionality with the occurrence of COPD-E (Fig. 2) (Figure S5). The effects of PM2.5 and O3 on COPD-E were significant, especially during the first three days of the lag.
A statistically significant association was observed for the effect of pollutants on the number of patients admitted to the emergency and hospitalization services with a diagnosis of COPD-E. The RR of COPD-E for each increment of 10μg/m3 were 1,04 (95%CI:1,02 - 1,07) for PM2.5 and 1,03 (95%CI:1,02 - 1,05) for O3 in the 0–3-day lag (Table 2) for the entire time series. The same behavior is shown for the lag 0-7 days for PM2.5 (RR=1.04; 95%CI:1.01 - 1.06) and O3 (RR=1.04; 95%CI: 1.02 - 1,05) and 0 - 15 days for PM2.5 (RR=1.03; 95%CI: 1.01 - 1.06) and O3 (RR=1.04; 95%CI: 1.02 - 1.04) (Table 2). All pollutants except NO2 show a statistically significant risk-increasing effect on admissions for COPD-E (Table 2).
In the stratified analysis by sex, the RRs for PM2.5 and O3 at lag 0-3 were higher in men than in women, with a difference of 15,0% and 3.0% for PM2.5 and O3, respectively. The increased risk of COPD-E was statistically significant in men (RR=1.04; 95%CI:1.01- 1.06) but not in women (RR=0.92; 95%CI:0.89- 0.94) Stratified analysis by season showed no statistically significant associations were found during the rainy season for any of the three air pollutants. However, when minimum rather than mean temperature was included in these models, a statistically significant association was found for PM2.5 (RR=1.03; 95%CI: 1.01 - 1.06) in the 0–3-day lag (Table 2).
According to the sensitivity analyses, the effect estimates changed little when the degrees of freedom were changed (Supplementary Table S1).
Table 3 shows the models that recorded the smallest values in the QAIC were the stratification of rainy season and minimum temperature (12,732.43), rainy season (12,765.13) and minimum temperature (19,262.25) for the average PM2.5, this same behavior of the variables that constituted the O3 models.
Discussion
Our results show a significant association between daily ambient air pollutant concentrations (PM2.5 and O3) and the number of emergency room visits or hospitalizations for COPD-E, mainly in the 0–3-day lag, in Bogotá. There was no evidence of an increased risk of COPD-E with increasing NO2 concentrations. The magnitude of the associations of COPD-E with PM2.5 and O3 was higher in men during the rainy season and when the increase in pollutants occurred in seasons with lower temperatures.
In this study, we estimate that for each 10 μg/m3 increase in PM2.5, a 4% (95%CI: 2% -7%) increase in emergency department admissions and hospitalizations occurred with a lag of 0 to 3 days. Our findings are consistent in the magnitude and direction with results reported for other cities (Jin et al. 2022; Dong et al. 2023; Zhang et al. 2018; Santus et al. 2012; Lin et al. 2020; Devries et al. 2017; Kloog et al. 2014; Ko et al. 2007; Xie et al. 2019). Other studies found no significant associations between PM2.5 and hospital admissions for COPD (Hoffmann et al. 2022; Belleudi et al. 2010; Slaughter et al. 2005; Stieb et al. 2009).
Our results also showed that a 10 ug/m3 O3 increase was associated with a 3% (95%CI: 1%-4%) increase in emergency department visits and hospital admissions for COPD-E with a lag of 0-3 days. Other studies have demonstrated this association, such as (Hoffmann et al. 2022), who showed an increased RR of 1.030 per 10 μg/m3 increase in O3 for hospitalization on the day of exposure (95% CI: 1.005 - 1.056). However, no significant association of O3 with the onset of COPD-E was found (Dong et al. 2023).
In contrast to the findings with PM2.5 and O3, our results showed no increased risk with NO2 and COPD-E (RR: 0.99; 95%CI: 0.97 – 1,01 per 10 μg/m3) for the lags evaluated. This association has been shown in other studies (Hoffmann et al. 2022; Dong et al. 2023; Devries et al. 2017; Peel et al. 2005; Li et al. 2016; Huh et al. 2022; Saki et al. 2020). A possible reason for the observed differences in exposure effect estimates could be chance or an unidentified bias (DeVries et al. 2016). The measured pollutants may be surrogates for another source of air pollution in the city, and the findings may be an artifact of measurement error at low concentrations. It could also be explained because the effect of NO2 may have a higher threshold, and short-term exposures are not apparent. Another possible reason is that NO2, being a gaseous traffic pollutant, can rapidly decrease its effect from the source and the monitoring station.
Our results also showed that in subgroup analyses by sex, a greater effect with statistical significance was observed in men than in women, consistent with previous studies (Liang et al. 2019; Szyszkowicz et al. 2018). The sex difference may be due to lifestyle factors (tobacco and alcohol intake, exercise and diet, occupational exposure outside the home) (Xie et al. 2019) and immune or hormonal responses.
At the same time, we found novel evidence that solar radiation, precipitation, relative humidity, and temperature influence COPD exacerbations. In contrast to most studies, these variables have been little investigated and considered in previous epidemiologic studies of short-term effects (Huh et al. 2022; Ferrari et al. 2012)
We found that the effects of PM2.5 on emergency department visits and hospitalizations for COPD-E were significant in the rainy season and at minimum temperature, with a range of 0-3 and 0-15 for PM2.5 increasing by 3% (95%CI: 1%-6%) for 10 μg/m3. The variation in the effects of PM2.5 and O3 according to the season could be explained by the fact that it coincides with the increased circulation of seasonal influenza virus (Sooryanarain and Elankumaran 2015) and that cold temperatures cause bronchoconstriction, increase the concentration of granulocytes and macrophages in the lower respiratory tract, reduce mucociliary clearance (D’Amato et al. 2015) and induce degranulation of mast cells in the respiratory tract (Proud et al. 1992), with COPD patients being more prone to COPD-E.
These findings are consistent with those documented by Liu et al. 2017 (Hwang et al. 2017), for every 10 μg/m3 increase in that of PM2.5 during the cold season increased hospitalizations for COPD-E, with an RR of 1.02 (95% CI:1.007-1.040, lag 0-1 day). Lam et al. showed a short-term association between COPD-E hospitalization at a cold temperature of 20°C with RR:1.50 (95% CI:1.34-1.68) and the lagged effects of cold temperature were up to 0-20 days (Lam et al. 2018). Therefore, during the rainy and cold seasons, the effects of PM2.5 and O3 on COPD-E hospitalizations and emergencies should be monitored. Studies should also be conducted to elucidate the underlying mechanisms of the variation in PM2.5 and O3 effects by season and temperature. Ehelepola et al. found that minimum temperature (1 to 5 °C decrease) was associated with COPD-E (Ehelepola et al. 2018).
The results shown in this study for people diagnosed for COPD-E with a significant increase of 10 μg/m3 in PM2.5 and O3 from lag 0 to 7 days are supported by previous meta-analyses by Li et al. 2016, which showed a significant association with increases of 10 μg/m3 for air pollutants (PM2.5, PM10, CO, NO2, SO2, and O3), especially for NO2 (RR: 1.04; 95%CI: 1.03, 1.06) and O3 (RR: 1.03; 95%CI: 1.01, 1.04) from lags 0 to 3 days. Li et al. 2022 also showed that the risk of COPD-E events in the emergency department and hospitalization increased significantly with an increase of 10 μg/m3 for PM2.5 and PM10 with a lag of 0 to 7 days. This fact confirms that individual and cumulative 0 to 7-day lags affect COPD-E, as documented in this study.
Several biological mechanisms may explain the effect of PM2.5 on COPD-E. Among these, airway irritation is prominent, causing interactions with the immune system that promote respiratory infections, oxidative stress, and lung inflammation (Li et al. 2016; Szyszkowicz et al. 2018; Mu et al. 2014). At the same time, the toxicity and irritancy of the particles aggravate pulmonary infection and reduce the immune response of the lung (Tsai et al. 2013). Other effects on the respiratory system from acute or chronic inhalation of PM, O3, and Environmentally Persistent Free Radicals (EPFRs) are the generation of Reactive Oxygen Species (ROS), which trigger and amplify an inflammatory process through endogenous production of more ROS (de Paula Santos et al. 2021).
This study had several limitations. First, we did not evaluate the effects of exposure to other air pollutants on emergency department admissions and hospitalizations for COPD for example, sulfur dioxide and carbon monoxide. Second, the use of network data has limited geographic resolution, but in terms of daily measurements, these are still the best local estimates. In addition, the location of the monitoring stations in the city of Bogotá D.C. ensures that the air pollutant concentrations used in this study are broadly representative of the urban area. Nevertheless, non-differential measurement errors resulting from using centrally located monitors are likely to attenuate associations. In addition, personal behaviors such as using heaters, gas fireplaces, or time spent outdoors may affect personal exposure levels. This could affect the magnitude of the observed associations compared to other locations with different behavioral profiles.
Third, the applied ecological time series study does not consider individual demographic, socioeconomic, or behavioral characteristics; this could be the subject of further research. Fourth is aggregation bias, which assigns group characteristics to all individuals and does not allow identification of individual sources of risk. Fifth, there is information bias due to possible underreporting of persons treated during the COVID-19 pandemic (Alsallakh et al. 2021; So et al. 2021). Sixth, the current study adjusted for the effects of temperature, relative humidity, precipitation, solar radiation, day of week, holidays and weekends, COVID-19 cases, and care for upper and lower respiratory tract infections, but not for other variables explaining COPD-E, such as comorbidities, severity of COPD, nutritional and immunological status, COPD severity and access to health services, due to lack of availability of individual data.
Despite the above limitations, this study has several advantages. The ecological study design with time series allows us to examine short-term variation in outcomes that changes in the primary exposure can explain; in our study, whether changes in air concentrations of PM2.5, NO2, and O3 partly explain daily changes in the number of people seen for COPD-E. DNLM considers the delayed effects of exposure factors and the non-linear relationship between exposure and response. The current findings help to understand the associations of air pollutants with COPD and provide novel insights for assessing the potential health effects of air pollution, setting public health priorities, and taking preventive measures for susceptible subgroups in the future. The advantage of studying this associations in Bogotá, a capital city with high altitude located in middle country is that, we are increasingly unaware of the importance of air quality in these countries.
Our findings have public policy implications since PM2.5 and O3 are short-lived air pollutants that cause global warming and contribute to climate change. COPD and related hospitalizations generate healthcare costs and are associated with decreased lung function and disease progression, reduced quality of life, decreased survival in COPD patients, and increased disease burden.
Conclusion
This study found that short-term exposure to PM2.5, O3, and meteorological variables were associated with COPD-E. Concentrations of PM2.5, O3, and meteorological factors (solar radiation and not only temperature) influence the frequency of emergency room visits and hospitalizations for COPD. Therefore, more efforts are needed to reduce air pollution, and efforts should be focused on approaching the WHO air quality guideline targets.
Data availability
All data generated or analyzed during this study are included in this article. Further demand can be directed to the corresponding author in email.
References
Abbafati C, Machado DB, Cislaghi B, Salman OM, Karanikolos M, McKee M et al (2020) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1223–1249
Alsallakh MA, Sivakumaran S, Kennedy S, Vasileiou E, Lyons RA, Robertson C et al (2021) Impact of COVID-19 lockdown on the incidence and mortality of acute exacerbations of chronic obstructive pulmonary disease : national interrupted time series analyses for Scotland and Wales. BMC Med 19:1–10
Bălă GP, Râjnoveanu RM, Tudorache E, Motișan R, Oancea C (2021) Air pollution exposure — the (in) visible risk factor for respiratory diseases. Environ Sci Pollut Res 28:19615–19628
Belleudi V, Faustini A, Stafoggia M, Cattani G, Marconi A, Perucci CA et al (2010) Impact of fine and ultrafine particles on emergency hospital admissions for cardiac and respiratory diseases. Epidemiology 21(3):414–423
Celli BR, Fabbri LM, Aaron SD, Agusti A, Brook R, Criner GJ et al (2021) An updated definition and severity classification of chronic obstructive pulmonary disease exacerbations: the Rome proposal. Am J Respir Crit Care Med. 204(11):1251–1258
CIOMS, OMS (2017) Pautas éticas internacionales para la investigación relacionada con la salud con seres humanos. Pautas éticas internacionales para la investigación biomédica en seres humanos
D’Amato G, Holgate ST, Pawankar R, Ledford DK, Cecchi L, Al-Ahmad M et al (2015) Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. a statement of the World Allergy Organization. World Allergy Organ J 8(1):25
de Paula Santos U, Arbex MA, ALF B, Mizutani RF, JED C, Terra-Filho M et al (2021) Environmental air pollution: respiratory effects. J Bras Pneumol 47(1):e20200267–e20200267
DeVries R, Kriebel D, Sama S (2016) Low level air pollution and exacerbation of existing copd: a case crossover analysis. Environ Health 15(1):98
Devries R, Kriebel D, Sama S (2017) Outdoor air pollution and copd related emergency department visits, hospital admissions and mortality: a meta-analysis. COPD: Int J Chron Obstruct Pulmon Dis 14(1):113–121. https://doi.org/10.1080/15412555.2016.1216956
Dominski FH, Lorenzetti Branco JH, Buonanno G, Stabile L, Gameiro da Silva M, Andrade A (2021) Effects of air pollution on health: a mapping review of systematic reviews and meta-analyses. Environ Res 201:111487
Dong J, You J, Wang J, Bao H (2023) Association between short-term ambient air pollution and outpatient visits for acute exacerbation of chronic obstructive pulmonary disease in Lanzhou, 2013–19. Environ Geochem Health 45(5):2495–2509. https://doi.org/10.1007/s10653-022-01363-0
Du W, Zhang W, Hu H, Zhang M, He Y, Li Z (2021) Associations between ambient air pollution and hospitalizations for acute exacerbation of chronic obstructive pulmonary disease in Jinhua, 2019. Chemosphere 267:128905. https://doi.org/10.1016/j.chemosphere.2020.128905
Ehelepola NDB, Ariyaratne K, Jayaratne A (2018) The association between local meteorological changes and exacerbation of acute wheezing in Kandy, Sri Lanka. Glob Health Action 11(1):1482998
Ferrari U, Exner T, Wanka ER, Bergemann C, Meyer-Arnek J, Hildenbrand B et al (2012) Influence of air pressure, humidity, solar radiation, temperature, and wind speed on ambulatory visits due to chronic obstructive pulmonary disease in Bavaria, Germany. Int J Biometeorol 56(1):137–143
Gasparrini A (2021) Distributed lag linear and non-linear models for time series data, dlnm version 2.4.7, 2021-10-07, pp 1–12
Gasparrini A, Armstrong B (2011a) Multivariate meta-analysis: A method to summarize non-linear associations. Stat Med 30(20):2504–2506
Gasparrini A, Armstrong B. Distributed lag non-linear models in R: the package dlnm. 2011b, Available cran r-project org/web/packages/dlnm/vignettes/dlnmOverview pdf (accessed 20 July 2011]. 43(8):1–20.
Gold Science Committee (2022) 2022 GOLD REPORTS 2022 Global strategy for prevention, diagnosis and management of COPD
Gold Science Committee (2023) Global Initiative for Chronic Obstructive Lung Disease 2023
Health Effects Institute, Institute for Health Metrics and Evaluation’s Global Burden of Desease project (2020) State of Global Air 2020, p 28 Available from: https://www.stateofglobalair.org/resources
Hoffmann C, Maglakelidze M, Evon S, Witt C, Hoffmann P, Butler T (2022) Asthma and COPD exacerbation in relation to outdoor air pollution in the metropolitan area of Berlin, Germany. Respir Res 23:64 Available from: https://search.ebscohost.com/login.aspx?direct=true&db=mnh&AN=35307034&site=eds-live
Hoogendoorn M, Feenstra TL, Boland M, Briggs AH, Borg S, Jansson SA et al (2017) Prediction models for exacerbations in different COPD patient populations: comparing results of five large data sources. Int J Chron Obstruct Pulmon Dis. 12:3183–3194
Huh JY, Hong J, Han DW, Park YJ, Jung J, Lee SW (2022) The impact of air pollutants and meteorological factors on chronic obstructive pulmonary disease exacerbations: a nationwide study. Ann Am Thorac Soc. 19(2):214–226
Hwang SL, Lin YC, Guo SE, Chou CT, Lin CM, Chi MC (2017) Fine particulate matter on hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in southwestern Taiwan during 2006-2012. Int J Environ Health Res 27(2):95–105
Jin JQ, Han D, Tian Q, Chen ZY, Ye YS, Lin QX et al (2022) Individual exposure to ambient PM2.5 and hospital admissions for COPD in 110 hospitals: a case-crossover study in Guangzhou, China. Environ Sci Pollut Res 29(8):11699–11706. https://doi.org/10.1007/s11356-021-16539-x
Kloog I, Nordio F, Zanobetti A, Coull BA, Koutrakis P, Schwartz JD (2014) Short term effects of particle exposure on hospital admissions in the Mid-Atlantic states: a population estimate. PLoS One 9(2):e88578
Ko FWS, Tam W, Wong TW, Chan DPS, Tung AH, Lai CKW et al (2007) Temporal relationship between air pollutants and hospital admissions for chronic obstructive pulmonary disease in Hong Kong. Thorax 62(9):780–785
Lam HCY, Chan EYY, Goggins WB 3rd. (2018) Comparison of short-term associations with meteorological variables between COPD and pneumonia hospitalization among the elderly in Hong Kong-a time-series study. Int J Biometeorol 62(8):1447–1460
Lee J, Jung HM, Kim SK, Yoo KH, Jung KS, Lee SH et al (2019) Factors associated with chronic obstructive pulmonary disease exacerbation, based on big data analysis. Sci Rep 9(1):1–8. https://doi.org/10.1038/s41598-019-43167-w
Li J, Sun S, Tang R, Qiu H, Huang Q, Mason TG et al (2016) Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 11:3079–3091. https://doi.org/10.2147/COPD.S122282
Li N, Ma J, Ji K, Wang L (2022) Association of PM2.5 and PM10 with Acute Exacerbation of Chronic Obstructive Pulmonary Disease at lag0 to lag7: a systematic review and meta-analysis. COPD 19(1):243–254
Liang L, Cai Y, Barratt B, Lyu B, Chan Q, Hansell AL et al (2019) Associations between daily air quality and hospitalisations for acute exacerbation of chronic obstructive pulmonary disease in Beijing, 2013-17: an ecological analysis. Lancet Planet Heal 3(6):e270–e279
Lin C, Li D, Lu J, Yu Z, Zhu Y, Shen P, Tang M, Jin M, Lin H, Shui L, Chen KWJ (2020) Short-term associations between ambient fine particulate matter pollution and hospital visits for chronic obstructive pulmonary disease in Yinzhou District, China. Env Sci Pollut Res 27(17):21647–21653
Liu Y, Han X, Cui X, Zhao X, Zhao X, Zheng H et al (2022) Association between air pollutants and acute exacerbation of chronic obstructive pulmonary disease: a time stratified case-crossover design with a distributed lag nonlinear model. Geohealth 6(2):e2021GH000529
Ministerio de Salud y ProtecciónSocial (2022) Sitio web. Sistema Integral de Información de la Protección Social
Morantes-Caballero JA, Fajardo Rodriguez HA (2019) Effects of air pollution on acute exacerbation of chronic obstructive pulmonary disease: a descriptive retrospective study (pol-AECOPD). Int J Chron Obstruct Pulmon Dis. 14:1549–1557
Mu L, Deng F, Tian L, Li Y, Swanson M, Ying J et al (2014) Peak expiratory flow, breath rate and blood pressure in adults with changes in particulate matter air pollution during the Beijing Olympics: a panel study. Environ Res 133:4–11
Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K et al (2005) Ambient air pollution and respiratory emergency department visits. Epidemiology 16(2):164–174
Proud D, Bailey GS, Naclerio RM, Reynolds CJ, Cruz AA, Eggleston PA et al (1992) Tryptase and histamine as markers to evaluate mast cell activation during the responses to nasal challenge with allergen, cold, dry air, and hyperosmolar solutions. J Allergy Clin Immunol 89(6):1098–1110
Roque A, Taborda-Barata L, Cruz ÁA, Viegi G, Maricoto T (2023)COPD treatment - a conceptual review based on critical endpoints. Pulmonology 29(5):410–420. https://doi.org/10.1016/j.pulmoe.2023.02.015https://www.sciencedirect.com/science/article/pii/S2531043723000557
Ross BA, Doiron D, Benedetti A, Aaron SD, Chapman K, Hernandez P et al (2023) Short-term air pollution exposure and exacerbation events in mild to moderate COPD: a case-crossover study within the CanCOLD cohort. Thorax 78(10):974–982
Saki H, Goudarzi G, Jalali S, Barzegar G, Farhadi M, Parseh I, Geravandi S, Salmanzadeh S, Yousefi F, Mohammadi MJ (2020) Study of relationship between nitrogen dioxide and chronic obstructive pulmonary disease in Bushehr, Iran. Clin Epidemiol Glob Heal. 8(2):446–449. https://doi.org/10.1016/j.cegh.2019.10.006
Santus P, Russo A, Madonini E, Allegra L, Blasi F, Centanni S, Miadonna A, Schiraldi G, Amaducci S (2012) How air pollution influences clinical management of respiratory diseases. a case-crossover study in Milan. Respir Res 13(95):1–12
Slaughter JC, Kim E, Sheppard L, Sullivan JH, Larson TV, Claiborn C (2005) Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J Expo Anal Environ Epidemiol 15(2):153–159
So JY, Hara NNO, Kenaa B, Williams JG, Christopher L, Slejko JF et al (2021) Population decline in COPD admissions during the COVID-19 pandemic associated with lower burden of community respiratory viral infections. Am J Med 134(10):1252–1259.e3. https://doi.org/10.1016/j.amjmed.2021.05.008
Soler-Cataluña JJ, Lopez-Campos JL (2022) COPD exacerbation syndrome: the Spanish perspective on an old dilemma. Int J Chron Obstruct Pulmon Dis 17:3139–3149
Sooryanarain H, Elankumaran S (2015) Environmental role in influenza virus outbreaks. Annu Rev Anim Biosci 3:347–373
Soriano JB, Kendrick PJ, Paulson KR, Gupta V, Abrams EM, Adedoyin RA et al (2020) Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med 8(6):585–596
Stieb DM, Szyszkowicz M, Rowe BH, Leech JA (2009) Air pollution and emergency department visits for cardiac and respiratory conditions: a multi-city time-series analysis. Environ Health 8:25
Stolz D, Mkorombindo T, Schumann DM, Agusti A, Ash SY, Bafadhel M et al (2022) The Lancet Commissions Towards the elimination of chronic obstructive pulmonary disease : a Lancet Commission. Lancet 400:921–972
Stoner O, Lewis J, Martínez IL, Gumy S, Economou T, Adair-Rohani H (2021) Household cooking fuel estimates at global and country level for 1990 to 2030. Nat Commun 12(1):5793
Szyszkowicz M, Kousha T, Castner J, Dales R (2018) Air pollution and emergenc department visits for respiratory diseases. Environ Res 163:263–269
Tang L, Shi S, Wang B, Liu L, Yang Y, Sun X et al (2021) Effect of urban air pollution on CRP and coagulation: a study on inpatients with acute exacerbation of chronic obstructive pulmonary disease. BMC Pulm Med 21(1):296
The R Foundation for Statistical Computing, Posit Software P. R version 4.3.1. 2023.
Ting MJ, Tsai YH, Chuang SP, Wang PH, Cheng SL (2021) Is PM(2.5) associated with emergency department visits for mechanical ventilation in acute exacerbation of chronic obstructive pulmonary disease? Am J Emerg Med 50:566–573
Tsai SS, Chang CC, Yang CY (2013) Fine particulate air pollution and hospital admissions for chronic obstructive pulmonary disease: a case-crossover study in Taipei. Int J Environ Res Public Health 10:6015–6026
WHO (2005) Guías de calidad del aire de la OMS relativas al material particulado, el ozono, el dióxido de nitrógeno y el dióxido de azufre.
World Health Organization WHO (2021) WHO global air quality guidelines Particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide.
World Health Organization WHO (2022) Ambient (outdoor) air pollution.
Xie J, Teng J, Fan Y, Xie R, Shen A (2019) The short-term effects of air pollutants on hospitalizations for respiratory disease in Hefei, China. Int J Biometeorol 63(3):315–326
Yan P, Liu P, Lin R, Xiao K, Xie S, Wang K et al (2019) Effect of ambient air quality on exacerbation of COPD in patients and its potential mechanism. Int J Chron Obstruct Pulmon Dis 14:1517–1526
Zhang H, Niu Y, Yao Y, Chen R, Zhou X, Kan H (2018) The Impact of ambient air pollution on daily hospital visits for various respiratory diseases and the relevant medical expenditures in Shanghai, China. Int J Environ Res Public Heal 15(15):425
Acknowledgments
To the National Institute of Public Health of Mexico (Instituto Nacional de Salud de Pública de México) for the research visit that allowed the methodology developed in this article to be carried out. To the Subdirectorate of Air, Auditory and Visual Quality of the District Secretary of Environment of Bogotá D.C. (Subdirección de calidad del aire, auditiva y visual de la secretaria Distrital de Ambiente de Bogotá D.C.), for providing the data on criteria air pollutants and meteorological variables. This work was approved by the Ethics Committee of the National School of Public Health of the University of Antioquia (Comité de Ética de la Facultad Nacional de Salud Pública de la Universidad de Antioquia), the Research Committee, and the Ethics Committee of the Colombian Pneumology Foundation (Comité de Ética de la Fundación Neumológica Colombiana). The study received no direct funding.
Funding
Open Access funding provided by Colombia Consortium No Applicable.
Author information
Authors and Affiliations
Contributions
Astrid Berena Herrera López: Conceptualization; Methodology; depuration of data, analysis statistics; write - corridor original; Visualization; Investigation y Analysis formals.
María Patricia Arbeláez: Supervision; Redaction: revision and edition.
Carlos Arturo Torres-Duque: Supervision; Redaction: revision and edition.
Néstor Yezid Rojas Roa: Supervision; Redaction: revision and edition.
Víctor Herrera: Supervision; Redaction: revision
José Luis Texcalac Sangrador: Supervision; Redaction: revision and edition; Analysis formals
Horacio Riojas Rodríguez: Supervision; Redaction: revision and edition; Analysis formals
Laura Andrea Rodríguez- Villamizar: Conceptualization; Supervision; Redaction: revision and edition; Analysis formals.
Corresponding author
Ethics declarations
Consent to publication
By means of this communication we, the authors, declare
- That the document is original
- That the document has not been previously published in any printed or digital media.
- That the document has not been submitted simultaneously to another publication for study or evaluation.
- That the document is the result of the intellectual collaboration of the authors.
- That the final version of the document, submitted for evaluation, has been read and approved by all authors.
- That in order to obtain the data and results shown in this article, the criteria of scientific ethics were followed, in accordance with the type of research carried out.
- We confirm that neither the manuscript nor any parts of its content are currently under consideration or published in another journal.
- All authors have approved the manuscript and agree with its submission to Journal Quality Atmosphere and Health.
Conflicts of Interest
The authors declare that they have no competing financial interests or known personal relationships that could have influenced the work reported in this paper. The authors are solely responsible for the content and writing of the article.
Ethics approval and consent to participate
This work was approved by the Ethics Committee of the National School of Public Health of the University of Antioquia (Comité de Ética de la Facultad Nacional de Salud Pública de la Universidad de Antioquia), the Research Committee, and the Ethics Committee of the Colombian Pneumology Foundation (Comité de Ética de la Fundación Neumológica Colombiana). The study received no direct funding. The ecological data were obtained from administrative records.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 2.66 MB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
López, A.B.H., Torres-Duque, C.A., Arbeláez, M.P. et al. Short-term effect of air pollution exposure on COPD exacerbations: a time series study in Bogota, Colombia. Air Qual Atmos Health (2024). https://doi.org/10.1007/s11869-024-01600-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11869-024-01600-8