Opinion statement
The internal tandem duplication (ITD) mutation of the FMS-like receptor tyrosine kinase 3 (FLT3-ITD) is the most common mutation observed in approximately 30% of acute myeloid leukemia (AML) patients. It represents poor prognosis due to continuous activation of downstream growth-promoting signaling pathways such as STAT5 and PI3K/AKT. Hence, FLT3 is considered an attractive druggable target; selective small FLT3 inhibitors (FLT3Is), such as midostaurin and quizartinib, have been clinically approved. However, patients possess generally poor remission rates and acquired resistance when FLT3I used alone. Various factors in patients could cause these adverse effects including altered epigenetic regulation, causing mainly abnormal gene expression patterns. Epigenetic modifications are required for hematopoietic stem cell (HSC) self-renewal and differentiation; however, critical driver mutations have been identified in genes controlling DNA methylation (such as DNMT3A, TET2, IDH1/2). These regulators cause leukemia pathogenesis and affect disease diagnosis and prognosis when they co-occur with FLT3-ITD mutation. Therefore, understanding the role of different epigenetic alterations in FLT3-ITD AML pathogenesis and how they modulate FLT3I’s activity is important to rationalize combinational treatment approaches including FLT3Is and modulators of methylation regulators or pathways. Data from ongoing pre-clinical and clinical studies will further precisely define the potential use of epigenetic therapy together with FLT3Is especially after characterized patients’ mutational status in terms of FLT3 and DNA methlome regulators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is a heterogeneous clonal disease characterized by aberrant proliferation of poorly differentiated cells in the hematopoietic system [1]. Patients are characterized based on the genetic alterations such as amplifications, deletions, rearrangements, and point mutations. The cytogenetic profiles of the patients are important in prognosis to assess risk levels and to decide on treatment approaches [2]. Some of the common gene mutations in AML are FLT3, NPM1, DNMT3A, and N/KRAS, considered significant diagnostic and/or prognostic markers [3, 4].
The FMS-like tyrosine kinase 3 (FLT3) encodes a receptor tyrosine kinase (RTK), which is mainly expressed on immature hematopoietic progenitors and hematopoietic stem cells (HSCs) [5•]. As these cells mature, the presence of the FLT3 receptor is reduced or completely lost [6]. FLT3 signaling is dependent on the binding of FLT3 ligand (FLT3L) to FLT3, resulting in dimerization of the receptor and autophosphorylation of the tyrosine residues. Then, downstream signaling pathways including PI3K/AKT, MAPK, and JAK2/STAT5 are activated, leading to increased cell growth and decreased apoptosis [7]. Two main mutations in the FLT3 receptor are internal tandem duplication (ITD) and tyrosine kinase domain (TKD) mutations, accounting for 20–25% and 5–10% of newly diagnosed AML patients, respectively [8]. These mutations cause FLT3L-independent dimerization and continuous activation of the receptor, initiating the aforementioned downstream signaling pathways, thereby increasing cell proliferation and suppressing apoptosis [1, 8]. FLT3-ITD mutations are associated with lower overall survival (OS) rate, poor treatment response, and shorter disease-free survival (DFS), which makes FLT3 an appealing treatment target in AML [9, 10]. Several small molecule inhibitors named FLT3 inhibitors (FLT3Is) have been developed with promising preclinical and clinical outcomes, some of which, including midostaurin, sorafenib, gilterinitib, and quizartinib, have been clinically approved for different clinical settings [11].
Pathogenesis of FLT3-ITD AML is not only triggered by this specific mutation but also by several epigenetic alterations [12]. Epigenetics alters gene expression without any change in the DNA sequence, which mainly includes DNA methylation, histone modification, and chromatin remodeling and impacts cell growth and disease development [13,14,15]. Dysregulation of epigenetic mechanisms activates oncogenes, inhibits tumor suppressor genes, and destabilizes the chromosomes, which leads to the development and progression of cancer [16]. Hence, several epi-mutations are commonly found in FLT3-ITD AML, including the gene mutations in histone modification Enhancer of Zeste Homologue 2 (EZH2) and the additional sex combs-like gene (ASXL1), regulation of DNA methylation (DNMT3A, TET2), and enzymes regulating metabolism (IDH1/2) with epigenetic consequences [14, 17]. Since epigenetic changes are reversible, targeting epigenetic regulators is thought to be a promising strategy in AML, such as using hypomethylating agents (HMAs), 5-azacitidine and decitabine, and histone deacetylase (HDAC) inhibitors [14]. However, the therapeutic efficacy of HMAs and HDAC inhibitors are limited when used as single agents. Hence, combination strategies of epigenetic therapy with targeted therapies such as FLT3Is are currently at different stages of pre-clinical and clinical studies.
In this review, the importance of DNA methylation in healthy and abnormal AML hematopoiesis will be summarized. Moreover, pre-clinical and clinical data regarding the role of DNA methylome alterations in the pathogenesis and treatment modalities of FLT3-ITD AML and potential approaches to target DNA methylation regulators alone or in combination with FLT3Is used in the clinic will be discussed.
FLT3-ITD AML
Molecular biology of FLT3-positive AML
The human FLT3 gene is found on chromosome 13q12, containing 24 exons and 993 amino acid residues and encodes for FLT3 transmembrane receptor belonging to type III RTK family [8, 18, 19]. Major cell types expressing FLT3 receptor are HSCs, multipotent progenitors, most myeloid and lymphoid progenitor cells, and mature dendritic cells [20]. Each FLT3 receptor contains an extracellular domain made up of 5 immunoglobulin-like subdomains, a transmembrane domain, an intracellular juxtamembrane (JM) domain, and an intracellular C-terminal domain [8]. The intracellular domain is composed of tyrosine kinase domain 1 (TKD1) and tyrosine kinase domain 2 (TKD2), which are linked by an activation loop (A-loop) [8].
FLT3L is an extracellular ligand being either attached to the cell membrane or in a soluble state, which is mainly produced by lymphocytes, HSCs, and bone marrow stromal cells [21]. FLT3L concentration is generally low but can increase due to aplasia, ensuring the controlled activation of FLT3 via negative-feedback mechanism [22]. When FLT3L binds to the extracellular domain of the receptor, FLT3 receptor undergoes dimerization followed by conformational changes in the JM domain, making the kinase domain accessible for ATP binding, and consequent autophosphorylation and activation of the receptor [10, 18, 23].
Two major FLT3 mutations, ITD and TKD, account for approximately 30% of AML patients, making them the most frequently identified mutations in AML [5•]. These mutations cause FLT3L-independent dimerization and activation of FLT3 receptor, hence, resulting in aberrant proliferation of the malignant cells even in the absence of FLT3L [24]. FLT3-ITD mutations occur in the JM domain, involving duplications of a fragment which vary in length and position [25, 26]. FLT3-ITD mutations are associated with increased relapse and reduced OS and the length of the duplicated fragment is inversely correlated with the OS [11, 25, 27]. On the other hand, FLT3-TKD mutations generally consist of single amino acid substitutions, deletions, or insertions located in the A-loop of the TKD, resulting in the loss of auto-inhibition [28]. Several signaling pathways regulating proliferation, differentiation, and apoptosis of HSCs are activated upon FLT3 dimerization [21]. Upon FLT3 binding, a series of events are triggered including autophosphorylation of tyrosine residues followed by adaptor proteins (such as GRB2, SHP2, and SRC family kinases) binding. These interactions primarily lead to the activation of PI3K/AKT/mTOR and RAS/MEK/ERK pathways [29,30,31,32,33]. FLT3-ITD and -TKD mutations activate similar pathways; however, FLT3-ITD specifically induces the JAK/STAT pathway through phosphorylation of STAT5A. Furthermore, FLT3-ITD mutations cause the reduced expression of C/EBPalpha and PU.1, which are crucial transcription factors for myeloid cell differentiation [34].
Clinically approved FLT3 inhibitors
Several tyrosine kinase inhibitors (TKIs) to target mutant FLT3 have been investigated. However, only some of them have been approved for the treatment of FLT3-ITD AML including midostaurin, sorafenib, gilterinitib, and quizartinib [5•]. TKIs are categorized as first- and next-generation inhibitors, distinguished by their particular capacity to inhibit FLT3 and the related downstream cascades [10, 11]. These inhibitors can be further characterized as type I or type II inhibitors depending on their effectiveness against both FLT3-ITD and -TKD mutations, or solely against FLT3-ITD mutations, respectively [10, 11, 35].
Midostaurin is a first-generation, type I FLT3I, targeting both FLT3-ITD and -TKD mutations [5•]. Midostaurin is originally a protein kinase C inhibitor; however, it also inhibits other tyrosine kinases including FLT3 [36]. After recognition of FLT3 mutations in AML pathogenesis, midostaurin is characterized as a FLT3i based on in vitro and in vivo studies [37]. Reports have shown that midostaurin inhibits FLT3 receptor signal transduction and induces cell cycle arrest and apoptosis [36]. In early clinical trials, midostaurin showed limited and transient activity as a single-agent treatment and induced about a 50% reduction in peripheral and bone marrow blast counts in relapsed/refractory (R/R) AML patients with FLT3 mutation [38]. When patients carrying either wild-type FLT3 or mutated FLT3 were treated, midostaurin achieved 42% and 71% reduction in the peripheral and bone marrow blasts, respectively [39]. Therefore, midostaurin failed to induce complete remission (CR). The limited clinical efficacy of midostaurin is resulted from the activation of alternative pathways, protection of leukemic clones, and limited presence of free midostaurin in the plasma [38, 39]. However, combination of midostaurin with other cytotoxic agents showed promising results in in vitro models followed by clinical trials [40, 41]. Combination of midostaurin with standard chemotherapy in newly diagnosed younger patients with FLT3-mutated AML achieved high CR and high OS rates [42]. The milestone RATIFY (NCT00651261) trial led to approval of midostaurin by Food and Drug Administration (FDA) in 2017 with the results of significantly increased OS and reduced death by 22% regardless of the high or low mutant allelic fractions or presence of TKD mutation [43, 44].
Sorafenib is a first-generation, type I FLT3I originally developed as a RAF kinase inhibitor. Sorafenib has also shown activity against other tyrosine kinases including FLT3 [45]. In vitro studies reported that sorafenib inhibits phosphorylation of downstream target proteins of FLT3 including RAF, MEK, ERK, and STAT5A and induces apoptosis in a Bim-dependent manner [45,46,47]. SORMAIN study demonstrated that addition of sorafenib results in higher probability of 24-month OS [48••]. Sorafenib showed safe and efficient profile on FLT3 mutant AML when it is combined with standard anthracycline/cytarabine induction therapy [49]. In the study including 99 newly diagnosed FLT3-ITD AML patient, sorafenib plus intensive chemotherapy showed better OS [50]. The results of these clinical studies resulted in approval of sorafenib by National Comprehensive Cancer Network (NCCN) in 2019 [51].
Gilteritinib is a type I, next-generation FLT3I having more potency against mutated FLT3. The mechanism of action of gilteritinib is through binding of the drug to the active site of the receptor and stabilizing the inactive conformation, thereby inhibiting the downstream signaling molecules including ERK and STAT5 [52]. FDA approval of gilteritinib in 2018 for the treatment of R/R AML FLT3 patients was based on ADMIRAL trial (NCT02421939) which reported higher CR and OS rates compared to salvage chemotherapy. In this trial, 49 patients treated with gilteritinib lived more than 2 years [53, 53, 54].
Quizartinib, a next-generation, type II FLT3i showed high potency, precise kinase selectivity, and favorable pharmacokinetic properties in in vitro and in vivo studies, making it a great candidate for clinical trials [55, 56]. QUANTUM-R (NCT02039726), which is a phase III study assessing quizartinib as a monotherapy in R/R FLT3-ITD AML patients, resulted in increased OS compared to salvage chemotherapy [57••]. Thirty-two percent of patients treated with quizartinib arm could proceed to an allogeneic stem cell transplantation (allo-SCT), which was 11% in salvage chemotherapy group. However, quizartinib caused cardiac toxicities and strong myeloid suppression which prevented its approval by FDA in the USA although it is approved as monotherapy in R/R FLT3-ITD AML in Japan in 2019 [58]. In 2023, FDA approved quizartinib based on the results from the QuANTUM-First (NCT02668653), a phase 3 clinical trial, to be used as an induction therapy with standard chemotherapy, cytarabine consolidation therapy, and as maintenance monotherapy, despite its side effects [59].
Epigenetics in FLT3-ITD AML
Cancer arises from a series of disruptions to the regulation of various cellular processes, such as cell growth, immortality, angiogenesis, cell death, invasion, and metastasis. Persistent changes in these functions are often driven by genetic mechanisms like mutations, copy number alterations, insertions, deletions, and recombination. As a result, cancer has traditionally been considered primarily a genetic disease. However, it is now clear that epigenetic changes offer an alternative route for acquiring stable oncogenic characteristics [12].
Epigenetics is commonly described as a genomic mechanism that exerts reversible effects on gene expression without changing DNA sequence [13]. These mechanisms involve DNA methylation, histone modification, chromatin remodeling, and RNA-associated modifications [14]. Epigenetic changes have the ability to influence cellular phenotype and to control several cellular activities such as cell growth, differentiation, and disease development [15]. Dysregulation of epigenetic mechanisms plays a crucial role in the development and progression of cancer, as they could activate oncogenes, cause chromosomal instability, and silence tumor suppressor genes [16]. Moreover, recurrent somatic alterations in genes with crucial roles in epigenetic regulation are frequently seen in AML [17]. Clinical observations and experimental evidences show that epigenetic mutations contribute to a pre-leukemic state but not adequate to cause full-blown acute leukemia [60]. Notably, the frequency of epigenetic mutations correlates with increasing age of AML patients. These mutations are also used as markers of prognostic risk stratification in AML [61]. As the changes caused by epigenetic mutations in the genome are frequently reversible, targeting epigenetic regulators or pathways holds important implications for therapeutic approaches in a specific subtype of AML, FLT3-ITD AML (Fig. 1) [14].
DNA methylome modifiers and their roles in FLT3-ITD AML
DNA methylation regulators in healthy and abnormal hematopoiesis
DNA methylation is a significant epigenetic modification in eukaryotic cells with a crucial role in regulating gene expression [62]. It is involved in several processes such as embryonic patterning, X-inactivation, and genomic imprinting [63]. The control of gene expression is achieved through addition of a methyl group to cytosine residues at specific CpG islands found in the promoter regions of about 50% of human genes, resulting in formation of 5-methylcytosine (5mC) [62, 64]. Cytosine methylation in these promoter regions leads to the recruitment of corepressor complexes, resulting in reduced gene expression [4]. Both hypo- and hypermethylation of CpG islands at different locations have been associated with the development of leukemia [62]. Hypermethylation of transcriptional enhancers and promoters of protein coding and non-coding genes is observed in different cancer types including AML [65]. These genes are associated with cell cycle control, DNA repair, apoptosis, and signaling pathways [66,67,68]. For instance, the results of a cohort study including 344 AML patients indicated that downregulation of genome-wide gene expression was found to be linked to hypermethylation of the genes in the majority of patients and distinct methylation profiles could be observed in different AML subtypes. However, DNA methylation is not likely to be the only factor for leukemogenesis [69].
DNA methyltransferases in hematopoiesis
DNA methyltransferases (DNMTs) are responsible for DNA methylation, which are encoded by DNMT1, DNMT2, DNMT3A, DNMT3B, and DNMT3L genes in the human genome [70]. DNMT1, DNMT3A, and DNMT3B possess functional methylation activities. DNMT3A and DNMT3B called de novo methyltransferases are responsible for methylation of several CpG islands while DNMT1, the maintenance methyltransferase, shows a higher affinity for hemi-methylated CpG dinucleotides [70,71,72]. DNMT1 level reaches the highest at the early S phase, methylating the newly synthesized CpG sites located opposite to methylated CpGs on the mother strand during the S phase of DNA replication, ensuring highly accurate maintenance of methylation patterns and decreases to its lowest level at G1 phase [72, 73]. The dynamics of DNA methylation determines the fate of HSCs [74, 75]. Although CpG methylation in HSCs and progenitor cells is low during normal differentiation process, CpG methylation is increased in the specific regions of the genes to be silenced that are not associated with the committed lineage to ensure proper differentiation [76]. For instance, loss of methylation of transcription factors like PRDM16, MEIS1, and HOXA9 is important for myeloid differentiation [77]. The maintenance of DNMT1 is essential for HSC survival and development through controlling self-renewal and differentiation, and suppressing apoptosis [74, 78, 79]. HSCs express higher levels of DNMT1 and its loss disrupts the differentiation and self-renewal potential of HSCs and progenitor cells [79]. DNMT1 depletion in HSCs leads to decreased promoter methylation of myeloerythroid genes including CD48, GATA1, C/EBPalpha, and ID2 resulting in reactivation of these genes, which hence induce skewed differentiation to myeloerythroid lineages with impaired lymphopoiesis [74, 80]. Similar to DNMT1, DNMT3A is also important for HSC self-renewal and differentiation [81]. DNMT3A-deficient HSCs in mice led to extensive repopulation of HSCs and declined the differentiation potential. Aberrant methylation pattern was observed in differentiation-related genes such as FLK2, PU.1, and IKAROS. Also, multipotency-related genes including RUNX1, GATA3, PBX1, and CDKN1A were hypomethylated [81,82,83]. Loss of DNMT3B appears to have similar phenotype to DNMT3A loss but the effects are milder [84].
DNA methyltransferases in FLT3-ITD AML
DNMTs are involved in cancer initiation by its increased or decreased expression resulting in hyper- or hypomethylation, respectively. Therefore, they regulate several tumor suppressor genes and oncogenes including BRCA1 and TGFβ in different cancer types and loss of DNMTs cause demethylation and re-expression of several tumor suppressor genes [85,86,87]. DNMT1 also maintains genomic stability through the interaction with DNA damage repair (DDR) systems that its disruption may contribute to cancer development. There are several studies showing hypermethylation of DDR genes in different cancer types [88,89,90]. In 2002, Di Croce provided the first mechanistic proof connecting genetic and epigenetic alterations in leukemogenesis suggesting that abnormal methylation of the genome plays a role in the early stages of tumorigenesis [91]. Di Croce found that PML-RAR fusion protein, an oncogenic transcription factor, recruited DNMT1 and DNMT3A to retinoic acid receptor beta 2 leading to its methylation and subsequent gene silencing in acute promyelocytic leukemia (APL) [91]. The interaction of DNMT1 with STAT3 and HDAC1 resulted in hypermethylation of SHP-1 tyrosine phosphatase in cutaneous T cell lymphoma [92]. The interaction of DNMT3A and DNMT3B with PU.1 in murine hematopoietic progenitor cells resulted in methylation of p16 tumor suppressor gene [93]. These studies suggest that DNMTs can be recruited by oncogenic transcription factors to CpG sites of tumor suppressor genes leading to aberrant methylation and silencing of the genes involved in tumorigenesis. Moreover, these three DNMTs were reported to be overexpressed in AML cells [94].
DNMT3B mutations are rare in AML and de novo methylation activity is mainly due to DNMT3A in AML cells [95, 96]. DNMT3A mutations can be missense, nonsense, frame-shift, and splice-site mutation. The most common mutation in DNMT3A is at a single amino acid residue which is arginine 882 [97]. HSCs with DNMT3A mutation undergo a pre-leukemic state with increased self-renewal which results in dysregulated DNA methylation [83, 98, 99]. This aberrant methylation pattern could be important to detect AML with no clinical indication [95]. Malignant transformation of HSCs in pre-leukemic state occurs by acquiring additional genetic alterations including FLT3, NPM1, and IDH1 mutations [97]. Moreover, this aberrant methylation in AML results in decreased expression of miRNA-370, a tumor suppressor, and increased expression of FOXM1, a tumor-promoting factor. Furthermore, dysregulated miRNAs in AML post-transcriptionally regulates DNMT1 which might lead to overexpression of DNMT1 [100]. Development and relapse of AML can be triggered by DNMT1 overexpression through hypermethylation of tumor suppressor genes. For instance, spalt-like transcription factor 4 (SALL4), which is a key molecule in hematopoiesis and leukemogenesis, leads to recruitment of DNMT1 to its promoter to block self-repression of HSCs [101,102,103]. Fatty acid-binding protein 4 (FABP4) also regulates DNMT1 expression by inducing IL-6/STAT3 axis promoting AML aggressiveness [104].
There are limited mechanistic studies on the role of DNMTs particularly in FLT3-ITD-positive AML. SHP-1 is a tumor suppressor gene negatively regulating JAK/STAT signaling which has an essential role in regulation of immune response, cell growth, and differentiation, therefore also in pathogenesis of AML. Mechanistically in FLT3-ITD-positive AML, upregulation of DNMT1, DNMT3A, and DNMT3B hypermethylate SHP-1 result in silenced SHP-1 and aberrant activation of STAT3 [105, 106]. Other tumor suppressor genes negatively controlling JAK/STAT pathway including SOCS-1 and SOCS-3 were also found to be silenced via promoter hypermethylation by DNMT1 [105]. Inhibition of DNMTs led to increased re-expression of tumor suppressor genes including CDKN2B, BIM, and CDKN2A in FLT3-ITD-positive AML [107]. The gene expression signature of FLT3-ITD/DNMT3A co-mutated murine models showed that HOXB3, CDKN2C, MYC1, ZFP521, and MEIS1 genes, some of which are related to HSC self-renewal and differentiation, were upregulated compared to wild-type murine models [108]. Another study showed that FLT3-ITD mutation together with DNMT3A mutation or deletion in mice caused resistance to PARP inhibitor [109]. High expression of DNMT3B was associated with low expression of MTSS1, a tumor suppressor, and decreased OS, while low expression of DNMT3B is linked to high expression of MTSS1 and increased OS. Moreover, in murine AML cells overexpressing FLT3-ITD, MTSS1 was found to be downregulated which might be linked to DNMT3B overexpression [110].
Ten-eleven-translocation enzymes in hematopoiesis
Another epigenetic regulator includes ten-eleven-translocation (TET) enzymes which catalyze the oxidation of 5mC to form 5-hydroxymethylcytosine (5hmC) [111]. These enzymes are crucial for both active and passive DNA demethylation influencing the binding and recruitment of chromatin regulators [112]. Active DNA methylation is carried out by oxidation of 5hmC to 5-formylcytosine and 5-carboxylcytosine which are directly recognized by thymine DNA glycosylase-mediated base-excision repair to produce unmethylated cytosine [113]. While TET1 and TET2 play a role in oxidation of 5mC, TET3 does not modify the DNA but it does regulate the expression level of TET2 [114], of which the enzymatic activity is important for myelopoiesis and noncatalytic activity is needed for HSC self-renewal and lymphopoiesis [115]. Moreover, 5hmC can be recognized by specific transcription factors (e.g., MECP2, the MBD3/NURD complex, UHRF1, UHRF2, SALL1/SALL4, PRMT1, RBM14, and WDR76) to induce gene expression [116, 117]. Also, TET proteins act as tumor repressor by maintaining genomic stability [113]. TET proteins mark the damaged DNA sites and control the expression of DNA repair genes including RAD50, BRCA1, RAD51, BRCA2, and TP53BP1 [118]. SMAD nuclear interacting protein 1 (SNIP1) is another TET2 interactor during DNA damage response. SNIP1 regulates c-MYC target genes participating in apoptosis by recruiting TET2 to the promoter region of c-MYC target genes [119]. Loss of TET1/TET2 or TET2/TET3 results in impaired DNA repair, suggesting that it promotes genomic stability. TET2 cooperates with TET1 and TET3 [120,121,122,123]. Consequently, loss of TET2 results in reduced 5hmC marks at the damaged regions impairing the DNA repair [118, 120, 124, 125].
As DNMTs, TET protein family is also important for normal hematopoiesis [95]. The regulation of epigenetic landscape in hematopoietic stem/progenitor cells (HSPCs) by TET family controls the phases of lineage commitment at various differentiation stages [112, 120, 126,127,128]. Therefore, TET proteins collaborate with lineage-specific transcription factors [129,130,131]. TET1 deficiency in HSCs of mice led to skewed differentiation into B cell lineage showing that TET1 is important for lymphoid differentiation [132]. TET3 deletion in mice resulted in increased number of HSCs without disturbing the frequency of differentiated cells [132]. TET2 is vastly expressed in HSCs but its expression is reduced after differentiation [133]. During myelopoiesis, C/EBPalpha activates TET2 and in cooperation with PU.1 and RUNX1 transcription factors, it is recruited to myeloid target genes including KLF4, CHD7, JUN, and SMAD3 [131, 134,135,136,137]. TET2 also regulates the genomic accessibility of erythroid transcription factors including GATA1, SCL, and KLF1 [129, 130]. Deletion of TET2 in mice enhanced the self-renewal capacity of HSCs by increasing the expression of MEIS1 and EVI1, and resulted in methylated erythroid transcription factor binding sites to block erythroid differentiation [137, 138]. Therefore, TET2 disruption shifted differentiation toward myeloid lineages [137]. Not only homozygous but also heterozygous disruption of TET2 enhanced the self-renewal capacity and myeloid differentiation showing that haploinsufficiency of TET2 is enough to disturb HSCs homeostasis [112, 128, 139, 140]. Moreover, miRNA-22 and CXXC-containing protein IDAX target TET2 for degradation. Overexpression of miRNA-22 and CXXC-containing protein IDAX also caused increased self-renewal and defective differentiation of HSCs [134, 141, 142].
Ten-eleven-translocation enzymes in FLT3-ITD AML
TET2 mutations are considerably common in hematological malignancies among three TET genes and TET3 alterations are the least common [143, 144]. In myeloid malignancies, TET1 has a tumor-promoting role. Especially in AML with MLL-fusion proteins, TET1 overexpression has been observed [145]. TET1 exerts an oncogenic role in AML as it upregulates the expression of oncogenes including HOXA9, MEIS1, and PBX3 [145] and downregulates the tumor suppressor targets such as miR-22 [146].
miR-22 represses CRTC1, FLT3, and MYCBP in FLT3-ITD human and mouse leukemic cells. Upregulation of TET1 represses miR-22 which eventually leads to aberrant activation of CREB, FLT3, and MYC pathway resulting in increased expression of oncogenic downstream targets [147]. High TET1 expression also regulates important oncogenic pathways as targeting STAT/TET1 axis proposed as a targeted therapeutic strategy in TET1 overexpressed AML [145, 148]. TET3 regulates the genes involved in AML-associated genes, glucose metabolism pathways, and STAT5A signaling pathway. Therefore, overexpression of TET3 promotes AML progression through epigenetic regulation of glucose metabolism and leukemic stem cell–associated pathways [149]. TET2 mutations can be deletions, nonsense, and missense mutations at highly conserved residues inactivating the enzyme [150, 151]. TET2 mutations are associated with reduced 5hmC levels, increased DNA methylation, and therefore increased epigenetic silencing [152]. TET2 controls the self-renewal of HSCs; hence, its loss in mouse model resulted in expansion of stem cells with increased repopulation ability [138, 146]. Consequently, TET2 mutations in HSCs leads to shift into pre-leukemic state which disrupts the ability of HSCs to differentiate into mature blood cells. TET2 mutations are considered early event in myeloid malignancies and additional mutations are needed for the development of full-blown leukemia [83, 98, 153]. TET2-mutated myeloid malignancies tend to have more mutational events than the TET2 wild-type malignancies suggesting that loss of TET2 causes hypermutagenicity [123]. Mutations in TET2 gene have been found in different hematologic malignancies including CMML, lymphoma, AML, MDS, and MPN [133]. Although the exact role of TET2 mutations and which genes and pathways it regulates is not fully understood in AML, in vitro studies and animal models suggest that loss of catalytic function of TET2 may contribute to leukemogenesis due to disruption of the cell renewal control, but its sole mutations are insufficient to induce AML [112, 152].
AML patients with TET2 mutations showed aberrant methylation and expression profiles of SRSF2, ASXL1, RUNX1, DNMT3A, FLT3-ITD, C/EBPalpha, and JAK2 compared to TET2 wild-type AML patients [154]. Although TET2 mutation alone is not enough to induce leukemia, TET2 loss in combination with FLT3-ITD mutation is found to be sufficient to induce AML in vivo [152, 155]. Moreover, survival of these TET2 ( −)/FLT3-ITD ( +) mice was significantly reduced compared to FLT3-ITD single mutated mice. Loss of TET2 in FLT3-ITD-mutated mice model resulted in reduced expression of GATA2, which is a regulatory gene in hematopoiesis and differentiation. Re-expression of GATA2 leads to restoration of differentiation and attenuates leukemogenesis [152]. TET2/FLT3-ITD co-mutation is also associated with the increased expression of long non-coding RNA (lnc) MORRBIDD specific to myeloid cells to regulate the lifespan, and loss of MORBID in TET2/FLT3-ITD-mutated mice model caused increased expression of BIM resulting in apoptosis and attenuated disease progression [156]. AML cells harboring both TET2 and FLT3-ITD mutations showed hypermethylation profiles in the regulatory elements of the genes including ID1, GATA1, MPL, and SOCS2 involved in self-renewal and differentiation [152].
Isocitrate dehydrogenases in hematopoiesis
Isocitrate dehydrogenases (IDHs) are NADP+-dependent enzymes catalyzing the conversion of isocitrate to a-ketoglutarate (a-KG) via oxidative decarboxylation within the krebs cycle [111, 157, 158]. The conversion of isocitrate to a-KG by IDH1/2 generates a crucial reducing agent, NADPH, which plays a pivotal role in regulating cellular defense mechanisms against oxidative stress through reduction of glutamine metabolism [159]. During this process, cells produce citrate and acetyl-CoA to sustain lipid metabolism and promote cellular growth under hypoxic conditions [160]. a-KG also binds to JmjC domain-containing histone demethylases (JmjC KDMs), TET2 and EGLN family of prolyl hydroxylases (PHDs), and ALKB homolog (ALKBH) DNA repair enzymes which have crucial roles in histone methylation, DNA methylation, and DNA repair, respectively [161, 162]. Hence, loss of IDH1/2 results in impaired detoxification mechanism and aberrant methylation leading to increased DNA damage and genome instability in cancer cells [163].
IDH1 is primarily located in the cytoplasm and peroxisomes, while IDH2 is localized in mitochondria [164]. IDH3 is the third isozyme located in the mitochondria; however, it has not been defined as mutated in cancer [165]. IDH1/2 mutations are heterozygous missense mutations in a single R residue within the active site of the enzyme [166]. Three conserved arginine residues, R132 for IDH1 and R172 and R140 for IDH2, are commonly mutated with wide-range of substitutions including polar (H, C, K, S, T, Q) and bulky nonpolar (W, V, M) amino acids [158]. The most common substitutions include IDH1 R132H, IDH1 R132C, IDH2 R172K, IDH2 172 M, and R140Q [167]. These mutations change the structure of the enzyme leading to reduced affinity to isocitrate and increased affinity to a-KG and NADPH to produce 2-hydroxyglutarate (2-HG) and NADP+ [168]. 2-HG disrupts metabolic processes and suppresses the krebs cycle, reducing the availability of α-ketoglutarate [169]. In cancer cells, IDH1/2 mutations lead to excessive accumulation of 2-HG, which is an oncometabolite inducing biochemical and epigenetic alterations though competitive inhibition of a-KG-dependent enzymes including KDMs, PHDs, TETs, and ALKBH DNA repairs enzymes [167]. For instance, inhibition of TET2 by 2-HG leads to increased 5mC levels; hence, IDH1/2 and TET2 mutations are mutually exclusive showing significant overlap methylation signatures [111]. IDH1 R132H mutant allele expression in mice mirrored many aspects of TET2 mutation and led to an increase in total 5-mC amount in HSPC compartment and bone marrow [114, 170]. Moreover, hypermethylation signatures in IDH1/2 mutant AML patient samples and TET2 mutant AML patient samples overlap and 93% of the genes which were overexpressed in TET2-mutated samples were also overexpressed in IDH1/2 mutated samples [111].
Expression of IDH2 R140Q mutation in murine bone marrow cells inhibited myeloid differentiation and caused accumulation of immature progenitor cells [111]. Furthermore, expression of either IDH2 R140Q or IDH1 R132H in TF-1 human erythroleukemia cell line blocked the differentiation [171,172,173]. Retroviral transfection of CKIT+ with IDH2 140Q and IDH2 R172K resulted in decreased number of myeloid progenitor cells and HSC accumulation [174]. Moreover, IDH1 R132H or IDH2 R140Q overexpression in HSCs led to extramedullary hematopoiesis and splenomegaly showing the presence of a myeloproliferative disease [175,176,177]. Mechanistically, TET2 is inhibited by 2-HG; therefore, TET2 cannot regulate PU.1 and WT1 target genes, leading to transcriptional repression [178, 179]. Not only PU.1 target genes but also GATA1 and GATA2 binding sites were 5mC enriched in IDH1/IDH2 mutant cells [111, 178, 180]. IDH1-mutated cells displayed overexpression of HOXA and HOXB cluster genes altering the differentiation which was associated with altered expression of RUNX1, PU.1, GATA1, and C/EBPalpha transcription factors [181]. In addition to TET2 inhibition, KDM inhibition by 2-HG results in decreased histone demethylation leading to differentiation blockage and promoted self-renewal of HSCs [162]. Hence, IDH1/2 mutations and 2-HG accumulation result in inhibition of blocked differentiation of HSCs and enhanced self-renewal through inhibition of DNA and histone demethylation [182]. 2-HG inhibits ALKB family proteins in a similar manner to TET enzymes; therefore, inhibition of ALKB family proteins leads to reduced DNA repair and accumulated DNA damage which may lead to cancer development through mutations [183].
Isocitrate dehydrogenases in cancer
Inhibition of PHD, which are the regulatory proteins to degrade hypoxia-inducible factor 1a (HIF-1a), also promotes cancer development and progression [162]. In addition to aforementioned effects of accumulation of 2-HG, apoptosis and cell cycle regulation are also affected by the IDH1/2 mutations. Mutant IDH1 leads to suppression of CDKN2A and CDKN2B stimulating MAPK pathway and results in enhanced cell proliferation [176, 184]. Furthermore, 2-HG inhibits cytochrome-c oxygenase, a component of the mitochondrial electron transport chain involved in removal of reactive oxygen species. Although the precise mechanism remains unclear, this inhibition leads to elevated BCL-2 expression, thereby inhibiting apoptosis in leukemic cells [185]. 2-HG stabilizes NF-kB activation in bone marrow stromal cells through ERK kinase pathway; hence, active NF-kB activates IL-6 and IL-8 secretion inducing AML cell proliferation [183]. 2-HG also induces hypermethylation signatures on the WNT inhibitory signals leading to increased stemness [186].
Despite the epigenetic and cellular changes caused by IDH1/2 mutations, expression of mutant IDH1/2 enzymes does not induce leukemic transformation [182]. Mouse models expressing mutant IDH1 or IDH2 showed similar patterns to those found in AML patients such as increased early hematopoietic progenitors, splenomegaly, anemia, hypermethylated DNA, and histone signatures. However, the mouse models did not develop full-blown leukemia [175]. Therefore, IDH1/2 mutations are considered early events in leukemogenesis and additional mutations including FLT3, MEIS1A, HOXA9, and NRAS are crucial to drive leukemogenesis [174, 177].
Prognostic impact of DNMTs in FLT3-ITD AML
Mutations in DNMT3A is identified in 15–25% of AML patients [62] and 36–44% of FLT3-ITD-positive AML patients carry concurrent DNMT3A mutations [187]. Although the role of mutant DNMT3A in leukemia development remains unclear, one hypothesis proposes that mutant DNMT3A has a dominant negative effect over wild-type DNMT3A [98]. Notably, R882H mutation in AML cells has been reported to have a significant reduction in de novo methyltransferase activity and increased proliferation [96, 188]. Co-occurrence of DNMT3A mutations with FLT3-ITD mutation is found to be indicative of a poorer prognosis [97, 189]. The peripheral white blood cell count is significantly higher in DNMT3A/FLT3-ITD co-mutated AML patients compared to FLT3-ITD AML patients and DNMT3A/FLT3-ITD mutations results in higher burden of disease compared to only DNMT3A-mutated AML patients [190, 191]. Concurrent DNMT3A and FLT3-ITD mutation in AML patients is related to poorer OS and worse outcomes after chemotherapy compared to single mutated FLT3-ITD or DNMT3A AML patients [190,191,192,193,194] The effectiveness of chemotherapy is also decreased in DNMT3A/FLT3-ITD-mutated patient group [191]. Moreover, patients carrying persistent DNMT3A/FLT3-ITD mutations had the highest rate of relapse after induction therapy [195]. Furthermore, early presence of DNMT3A mutations is found to be linked to a higher incidence of FLT3-ITD-positive clones at relapse [64, 196]. While DNMT3A mutations are the most studied ones in FLT3-ITD AML, there are limited studies related to the roles of other DNMTs. High DNMT1 expression was correlated with p15 methylation in FLT3-ITD AML and DNMT1 inhibition caused upregulation of p15 and p16 tumor suppressor genes [107]. Another report showed that high DNMT3B expression was observed in FLT3-ITD AML patients compared to FLT3-WT AML patients, which was associated with poor prognosis [110].
Prognostic impact of TETs in FLT3-ITD AML
TET1 mutations are found in 1–5% AML patients [17]. As the most mutated TET family protein is TET2, mutations in TET2 gene are observed in 7 to 23% of AML patients particularly with a normal karyotype and are associated with poorer OS and reduced response to chemotherapy [62, 64, 197]. One study demonstrated that AML patients with homozygous TET2 mutations showed inferior event-free survival (EFS) and higher relapse rate compared to heterozygous TET2-mutated AML patients [198]. Moreover, the presence of TET2 mutations together with FLT3 mutations indicates an adverse outcome [199,200,201]. Patients with TET2/FLT3-ITD double mutation had lower the 3-year OS (37.9% vs 25%), DFS (48.9% vs 16.7%), and EFS (27.8% vs 16.7%) compared to patients with FLT3-ITD mutation [202]. Co-occurrence of TET2 mutations with FLT3-ITD mutations may result in the development of leukemia inducing synergistic gain-of-function effects on DNA methylation, therefore gene expression. Moreover, blocking only FLT3 signaling in TET2/FLT3-ITD-mutated AML is not enough to restore mutated TET2 activity. Therefore, methylated CpGs cannot be reversed, presenting a potential resistance mechanism to FLT3 inhibitor monotherapy [152]. However, deletion of TET2 from FLT3-ITD-mutated cells increased sensitivity toward PARP inhibitor or PARP inhibitor plus quizartinib therapy, while deletion of DNMT3A caused resistance compared to FLT3-ITD-mutated cells [109]. In contrary, in TET2/FLT3-ITD-mutated mice model, CXCR4 and CXCL12 expressions were increased compared to FLT3-ITD mice causing resistance to chemotherapy and FLT3 inhibitor [155]. In a de novo study, high frequency of FLT3-ITD mutations at relapse was associated with TET2 or IDH1/2 mutations suggesting that mutations in epigenetic regulators in AML may induce FLT3-ITD mutations through genetic instability and it may lead to relapse and resistance to therapy [196].
Prognostic impact of IDHs in FLT3-ITD AML
The frequencies of IDH1 and IDH2 mutations in AML are 7–14% and 8–19%, respectively [165]. IDH1/2 mutations are exclusively heterozygous and are generally found in AML patients with normal cytogenetics [17, 200, 203]. The prevalence of IDH1/2 mutations is higher in older AML patients carrying intermediate risk [17]. Moreover, patients carrying IDH1/2 mutations frequently have higher platelet count, higher peripheral blast, and bone marrow percentages compared to wild-type IDH1/2 AML patients [204,205,206]. IDH mutations are mostly considered an early event in carcinogenesis and may remain after chemotherapy or at relapse [207,208,209]. Although AML patients with IDH1 mutations and AML patients with IDH2 mutations show a significant overlap in the differentially expressed genes, in a meta-analysis including 12,747 patients, it was reported that IDH1 mutation was associated with inferior OS and EFS while IDH2 mutation was associated with favorable OS [210]. Another meta-analysis showed that the most frequent concurrent mutation is NPM1 followed by FLT3-ITD [206]. Moreover, IDH1 and IDH2 mutations co-occur in 15–27% and 8–30% of AML patient with FLT3-ITD, respectively [211]. Furthermore, co-occurrence of FLT3-ITD and IDH1 mutation is considered a negative prognostic factor and is associated with shorter OS and EFS [210].
Targeting DNA methylome in FLT3-ITD AML
Targeting DNA methylation in AML has gained significant attention, given the fact that it represents a potential therapeutic strategy to reverse the epigenetic dysregulations that contribute to disease progression, drug resistance, and inferior prognostic impact in the presence of FLT3-ITD mutations.
Azacitidine and decitabine are pyrimidine analogs approved for the treatment of AML, resulting in low blast count. These compounds function as the inhibitors of DNMTs to reverse DNA hypermethylation, therefore restoring the expression of critical genes including tumor suppressor genes [212]. Azacitidine incorporates into RNA and to a lesser extent into DNA while decitabine only incorporates into DNA. DNA incorporation leads to formation of covalent bonds with DNA methyltransferases, hence blocking DNA hypermethylation [213, 214]. Although there are several studies on decitabine or azacitidine for AML treatment, studies of these drugs as a single agent on FLT3-ITD-mutated AML are limited. Hu and colleagues showed that decitabine, as a single agent, on MV4-11 and MOLM-13 FLT3-ITD AML cells, induced C/EBP alpha-PU.1 pathway, which is required for myeloid differentiation, leading to downregulation of FLT3 and induction of apoptosis. In another study, FLT3-ITD + /TET2 mutant mice model treated with azacitidine, which resulted in normalization in peripheral blood cell counts and splenomegaly, decreased total white blood cell count and spleen weight. Also, treatment with azacitidine reduced the aberrant DNA methylation in the stem-progenitor cells. Additionally, azacitidine treatment restored the myeloid maturation toward normal neutrophil populations [215]. In mouse xenograft models of FLT3-ITD AML, decitabine was effective to reduce the tumor volume [216]. Treatment of CEP-701, a TKI, resistant-MV4-11 cell line with azacitidine, resulted in re-expression of SHP-1, a tumor suppressor gene and negative regulator of STAT3, leading to suppression of STAT3 and induction of apoptosis [106]. Another study evaluating the effects of decitabine and azacitidine showed that both azacitidine and decitabine treatment resulted in DNA double-strand breaks and subsequent activation of p53 in MOLM-13 cells. Also, both agents reduced the expression of TERT, BCL-2, and MYC oncogenes in these cells [217]. In a post hoc analysis of QUAZAR AML-001 phase 3 trial (NCT01757535), 66 patients with FLT3-mutated AML (46 patients with FLT3-ITD) were treated with oral azacitidine and the median OS was prolonged in FLT3-mutated AML patients compared to the placebo group (28.2 months vs 9.7 months). Relapse-free survival (RFS) was also improved in FLT3-mutated AML patients with 23.1 months compared to placebo (4.6 months) [218].
Targeting DNMT in FLT3-ITD AML is also achieved through modulation of DNMT regulators. Sp1 is a zinc finger transcription factor which binds to the promoter region of DNMT1 and p65 is NF-κB signaling component which interplays with Sp1 for DNMT1 transactivation in FLT3-ITD AML. Therefore, disruption of Sp1/NF-κB complex impairs the expression of DNMT1 leading to DNA hypomethylation [219,220,221]. Bortezomib, a proteasome inhibitor, is used to reduce Sp1 levels in MV4-11 cells resulting in decreased DNMT1 expression, therefore leading to lower global genomic DNA methylation compared to the control [221]. Thymoquinone is a natural product with anti-cancer activity which decreases the Sp1 levels. It decreases DNMT1 and DNMT3A expression levels leading to downregulation of KIT, FLT3, STAT5, and AKT in MV4-11 cells [220]. Moreover, treatment of MV4-11 cells with either thymoquinone or azacitidine leads to decreased methylation levels on the promoter regions of SOCS-1, SHP-1, and SOCS-3 tumor suppressor genes, causing increased expression of these genes and decreased expression of FLT3-ITD, JAK2, STAT3, and STAT5 [105].
Two agents are recently approved to target IDH mutations [222]. Enasidenib is a selective allosteric inhibitor of IDH2 which binds to open conformation of the enzyme and stabilizes it, thereby blocking the conversion of a-KG to 2-HG [223]. Ivosidenib is a reversible allosteric competitive inhibitor of IDH1, competing with the essential cofactor, magnesium ion, to bind to IDH1, which prevents the formation of a catalytically active site [224]. Enasidenib therapy in FLT3-ITD + /IDH2 R140Q double mutated mice model decreased the 2-HG serum levels and induced demethylation of the hypermethylated promoters in leukemia-derived cells. Moreover, treatment with enasidenib normalized the myeloid maturation [215]. In clinical trials, enasidenib alone was not effective for the patients with FLT3 and IDH co-mutations [225].
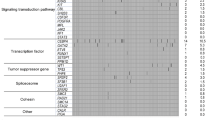
Combinational therapies including clinically approved FLT3Is and epi-drugs
The rationale behind combining FLT3Is with epigenetic drugs lies in the potential synergy they could create to enhance FLT3I’s activity especially when FLT3I resistance occurs. FLT3 inhibitors can directly target the cancer cells with FLT3 mutations while epigenetic drugs can modify the epigenetic landscape of the cells, potentially enhancing the effectiveness of FLT3 inhibition. Several pre-clinical and clinical studies have explored the combination of FLT3Is and epi-drugs in FLT3-ITD AML treatment (Tables 1 and 2, Fig. 2).
Sequential treatment with decitabine followed by midostaurin synergistically induced apoptosis through overexpression of apoptotic BIM in FLT3-ITD AML-positive MV4-11 and MOLM-13 cells [227]. Treatment of FLT3-ITD + /TET2-mutant and FLT3-ITD + /IDH2 R140Q double mutated mice models with quizartinib in combination with azacitidine or enasidenib, respectively, showed significant response compared to control or monotherapy, reducing leukemic blast in the bone marrow, spleen, and liver. Combination therapy decreased DNA methylation even more than the monotherapy [215]. FLT3-ITD and IDH2 R172K or IDH2 R140Q double mutated zebrafish model, when treated with quizartinib and enasidenib, showed reduction in the blast population and spleen size [226]. Treatment of MOLM-14 cells and newly diagnosed and relapsed FLT3-ITD-mutated AML patient–derived cells with quizartinib and azacitidine/decitabine resulted in synergistic growth inhibition. When sequential or simultaneous treatment with quizartinib and DNMT inhibition were compared, simultaneous DNMT inhibition and quizartinib treatment induced synergistic or additive effect compared to sequential treatment [228]. In another study, treatment of MV4-11 and MOLM-13 cells with gilteritinib and azacitidine resulted in induction of apoptosis, and in xenografted mouse tumor volume was significantly decreased in gilteritinib plus azacitidine–treated group compared to gilteritinib-treated group [229]. Similar to quizartinib and gilteritinib, the combination of azacitidine with sorafenib also synergistically inhibited MOLM-13 and MV4-11 cell growth, induced apoptosis, and decreased tumor volume in xenograft mouse model of FLT3-ITD AML. In another study, sorafenib is combined with decitabine to treat MV4-11 cells, resulting in growth inhibition and synergistic effect [231].
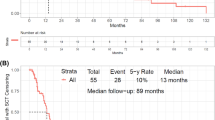
Quizartinib plus azacitidine treatment was given as a frontline or salvage therapy in a cohort of 38 FLT3-ITD AML patients. Eighty-seven percent of composite response (CRc) rate was achieved in the frontline-treated group and 67% of CRc was achieved in R/R AML patients [232]. When FLT3-ITD AML patients treated with azacitidine combined with sorafenib, allelic burden and FLT3-ITD clone size were significantly reduced and progression-free survival (PFS) was significantly increased compared to sorafenib treatment alone [230]. Patients who had relapsed after allo-SCT and had FLT3-ITD mutations treated with 5-azacitidine and sorafenib. While three out of 5 patients achieved CR, the remaining 2 patients experienced disease progression [233]. In a cohort of 40 FLT3-ITD-mutated AML patients, treatment with sorafenib plus azacitidine resulted in 46% of overall CRc rate. While previously untreated patients had 67% of response rate, it was lower for primary refractory or relapsed patients with 58% and 32%, respectively (NCT01254890) [234]. Another clinical trial, in which 27 newly diagnosed elderly (61–86 years) AML patients with FLT3-ITD mutation were treated with sorafenib plus azacitidine, resulted in 78% of overall response rate (ORR) suggesting that azacitidine and sorafenib combination is well tolerated and effective to treat older patients with FLT3-ITD-mutated AML who have not received previous treatment (NCT02196857) [235]. In a phase 3 trial, 123 patients with FLT3-ITD-positive AML who are not eligible for intensive chemotherapy were treated with gilteritinib plus azacitidine or azacitidine alone and CRc rates were 58.1% and 26.5% respectively showing no new significant safety issues compared to individual therapy (NCT02752035) [236••].
Murine model of FLT3-ITD and IDH2 co-mutated AML showed that enasidenib treatment significantly reduced 2-HG levels and induced demethylation of hypermethylated CpG islands, but enasidenib alone was not enough to suppress the malignant clones. However, when combined with quizartinib, leukocytosis reduction was more effective compared to enasidenib monotherapy [215]. In a recent study, FLT3 and/or IDH inhibitors (FLT3Is and/or IDHIs) were administered as a single agent or in combination with cytotoxic chemotherapy (CCT) or low-intensity therapy (LIT) in 91 AML patients with FLT3-ITD/IDH1 or FLT3-ITD/IDH2 double mutations. The results demonstrated that a combination of a FLT3I with CCT or LIT was effective in patients with FLT3-ITD/IDH co-mutated disease in both the frontline and R/R settings [237].
Conclusions
Understanding the roles of epigenetic regulators in normal hematopoiesis and in initiation and maintenance of hematopoietic malignancies including FLT3-ITD AML have paved the way for the development of epigenetically targeted therapies including small-molecule inhibitors of certain epigenetic regulators involved in DNA methylation (azacitidine and decitabine) and other epigenetic-related processes such as IDH-related modifications. Some of these therapeutic approaches have already undergone clinical trials alone or in combination with clinically approved FLT3Is including midostaurin, sorafenib, and gilteritinib which evaluate their efficacy, safety profile, and patients’ benefit as indicated in Table 2. However, majority of them is still infant passing through in vitro and in vivo experimental stages with promising outcomes (Table 1). On the other hand, it is quite important to define epigenetic alterations at the individual level for the development of specific epigenetic biomarkers to predict response to therapy and to identify epi-drugs with specific and durable outcomes in the near future for the treatment of FLT3-ITD AML patients. It would be assumed that combination of epigenetic therapy and FLT3Is could promise higher success rates as compared to epi-drugs or FLT3Is alone after revealing mechanisms of action of novel epigenetic alterations and carrying out larger randomized trials.
Data Availability
No datasets were generated or analysed during the current study.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grafone T, Palmisano M, Nicci C, Storti S. An overview on the role of FLT3-tyrosine kinase receptor in acute myeloid leukemia: biology and treatment. Oncol Rev. 2012;6(1):e8. https://doi.org/10.4081/oncol.2012.e8.
Daver N, Schlenk RF, Russell NH, Levis MJ. Targeting FLT3 mutations in AML: review of current knowledge and evidence. Leukemia. 2019;33(2):299–312. https://doi.org/10.1038/s41375-018-0357-9.
Kihara R, Nagata Y, Kiyoi H, Kato T, Yamamoto E, Suzuki K, et al. Comprehensive analysis of genetic alterations and their prognostic impacts in adult acute myeloid leukemia patients. Leukemia. 2014;28(8):1586–95. https://doi.org/10.1038/leu.2014.55.
Takahashi S. Current findings for recurring mutations in acute myeloid leukemia. J Hematol Oncol. 2011;4:36. https://doi.org/10.1186/1756-8722-4-36.
• Tecik M, Adan A. Therapeutic targeting of FLT3 in acute myeloid leukemia: current status and novel approaches. Onco Targets Ther. 2022;15:1449–78. https://doi.org/10.2147/ott.S384293. Reference 5 is a comprehensive study explaining all clinically FLT3 inhibitors and novel therapeutics targeting FLT3 in detail.
Small D, Levenstein M, Kim E, Carow C, Amin S, Rockwell P, et al. STK-1, the human homolog of Flk-2/Flt-3, is selectively expressed in CD34+ human bone marrow cells and is involved in the proliferation of early progenitor/stem cells. Proc Natl Acad Sci U S A. 1994;91(2):459–63. https://doi.org/10.1073/pnas.91.2.459.
Leick MB, Levis MJ. The Future of Targeting FLT3 Activation in AML. Curr Hematol Malig Rep. 2017;12(3):153–67. https://doi.org/10.1007/s11899-017-0381-2.
Kiyoi H, Kawashima N, Ishikawa Y. FLT3 mutations in acute myeloid leukemia: therapeutic paradigm beyond inhibitor development. Cancer Sci. 2020;111(2):312–22. https://doi.org/10.1111/cas.14274.
• Daver N, Venugopal S, Ravandi F. FLT3 mutated acute myeloid leukemia: 2021 treatment algorithm. Blood Cancer J. 2021;11(5):104. https://doi.org/10.1038/s41408-021-00495-3. Reference 9 represent updated review of treatment options specifically for FLT3-mutated AML in 2021, focusing on the MD Anderson approach.
Antar AI, Otrock ZK, Jabbour E, Mohty M, Bazarbachi A. FLT3 inhibitors in acute myeloid leukemia: ten frequently asked questions. Leukemia. 2020;34(3):682–96. https://doi.org/10.1038/s41375-019-06. This refers to a recently updated review of treatment optionsspecifically for FLT3-mutated AML in 2021, highlighting theMD Anderson approach.4-3.
Wang Z, Cai J, Cheng J, Yang W, Zhu Y, Li H, et al. FLT3 inhibitors in acute myeloid leukemia: challenges and recent developments in overcoming resistance. J Med Chem. 2021;64(6):2878–900. https://doi.org/10.1021/acs.jmedchem.0c01851.
Shen H, Laird PW. Interplay between the cancer genome and epigenome. Cell. 2013;153(1):38–55. https://doi.org/10.1016/j.cell.2013.03.008.
Cheng Y, He C, Wang M, Ma X, Mo F, Yang S, et al. Targeting epigenetic regulators for cancer therapy: mechanisms and advances in clinical trials. Signal Transduct Target Ther. 2019;4(1):62. https://doi.org/10.1038/s41392-019-0095-0.
Wouters BJ, Delwel R. Epigenetics and approaches to targeted epigenetic therapy in acute myeloid leukemia. Blood. 2016;127(1):42–52. https://doi.org/10.1182/blood-2015-07-604512.
Bird A. Perceptions of epigenetics. Nature. 2007;447(7143):396–8. https://doi.org/10.1038/nature05913.
Bhalla KN. Epigenetic and chromatin modifiers as targeted therapy of hematologic malignancies. J Clin Oncol. 2005;23(17):3971–93. https://doi.org/10.1200/jco.2005.16.600.
Ley TJ, Miller C, Ding L, Raphael BJ, Mungall AJ, Robertson A, et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368(22):2059–74. https://doi.org/10.1056/NEJMoa1301689.
Rosnet O, Schiff C, Pébusque MJ, Marchetto S, Tonnelle C, Toiron Y, et al. Human FLT3/FLK2 gene: cDNA cloning and expression in hematopoietic cells. Blood. 1993;82(4):1110–9.
Gilliland DG, Griffin JD. The roles of FLT3 in hematopoiesis and leukemia. Blood. 2002;100(5):1532–42. https://doi.org/10.1182/blood-2002-02-0492.
Tsapogas P, Mooney CJ, Brown G, Rolink A. The cytokine Flt3-ligand in normal and malignant hematopoiesis. Int J Mol Sci. 2017; 18(6). https://doi.org/10.3390/ijms18061115
Hannum C, Culpepper J, Campbell D, McClanahan T, Zurawski S, Bazan JF, et al. Ligand for FLT3/FLK2 receptor tyrosine kinase regulates growth of haematopoietic stem cells and is encoded by variant RNAs. Nature. 1994;368(6472):643–8. https://doi.org/10.1038/368643a0.
Zhao JC, Agarwal S, Ahmad H, Amin K, Bewersdorf JP, Zeidan AM. A review of FLT3 inhibitors in acute myeloid leukemia. Blood Rev. 2022;52:100905. https://doi.org/10.1016/j.blre.2021.100905.
Dosil M, Wang S, Lemischka IR. Mitogenic signalling and substrate specificity of the Flk2/Flt3 receptor tyrosine kinase in fibroblasts and interleukin 3-dependent hematopoietic cells. Mol Cell Biol. 1993;13(10):6572–85. https://doi.org/10.1128/mcb.13.10.6572-6585.1993.
Nakao M, Yokota S, Iwai T, Kaneko H, Horiike S, Kashima K, et al. Internal tandem duplication of the flt3 gene found in acute myeloid leukemia. Leukemia. 1996;10(12):1911–8.
Janke H, Pastore F, Schumacher D, Herold T, Hopfner KP, Schneider S, et al. Activating FLT3 mutants show distinct gain-of-function phenotypes in vitro and a characteristic signaling pathway profile associated with prognosis in acute myeloid leukemia. PLoS ONE. 2014;9(3):e89560. https://doi.org/10.1371/journal.pone.0089560.
Schnittger S, Bacher U, Haferlach C, Alpermann T, Kern W, Haferlach T. Diversity of the juxtamembrane and TKD1 mutations (exons 13–15) in the FLT3 gene with regards to mutant load, sequence, length, localization, and correlation with biological data. Genes Chromosomes Cancer. 2012;51(10):910–24. https://doi.org/10.1002/gcc.21975.
Patnaik MM. The importance of FLT3 mutational analysis in acute myeloid leukemia. Leuk Lymphoma. 2018;59(10):2273–86. https://doi.org/10.1080/10428194.2017.1399312.
Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S, et al. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood. 2001;97(8):2434–9. https://doi.org/10.1182/blood.v97.8.2434.
Rottapel R, Turck CW, Casteran N, Liu X, Birnbaum D, Pawson T, et al. Substrate specificities and identification of a putative binding site for PI3K in the carboxy tail of the murine Flt3 receptor tyrosine kinase. Oncogene. 1994;9(6):1755–65.
Heiss E, Masson K, Sundberg C, Pedersen M, Sun J, Bengtsson S, et al. Identification of Y589 and Y599 in the juxtamembrane domain of Flt3 as ligand-induced autophosphorylation sites involved in binding of Src family kinases and the protein tyrosine phosphatase SHP2. Blood. 2006;108(5):1542–50. https://doi.org/10.1182/blood-2005-07-008896.
Zhang S, Fukuda S, Lee Y, Hangoc G, Cooper S, Spolski R, et al. Essential role of signal transducer and activator of transcription (Stat)5a but not Stat5b for Flt3-dependent signaling. J Exp Med. 2000;192(5):719–28. https://doi.org/10.1084/jem.192.5.719.
Zhang S, Broxmeyer HE. Flt3 ligand induces tyrosine phosphorylation of gab1 and gab2 and their association with shp-2, grb2, and PI3 kinase. Biochem Biophys Res Commun. 2000;277(1):195–9. https://doi.org/10.1006/bbrc.2000.3662.
Zhang S, Mantel C, Broxmeyer HE. Flt3 signaling involves tyrosyl-phosphorylation of SHP-2 and SHIP and their association with Grb2 and Shc in Baf3/Flt3 cells. J Leukoc Biol. 1999;65(3):372–80. https://doi.org/10.1002/jlb.65.3.372.
Choudhary C, Schwäble J, Brandts C, Tickenbrock L, Sargin B, Kindler T, et al. AML-associated Flt3 kinase domain mutations show signal transduction differences compared with Flt3 ITD mutations. Blood. 2005;106(1):265–73. https://doi.org/10.1182/blood-2004-07-2942.
Senapati J, Kadia TM. Which FLT3 inhibitor for treatment of AML? Curr Treat Options Oncol. 2022;23(3):359–80. https://doi.org/10.1007/s11864-022-00952-6.
Weisberg E, Boulton C, Kelly LM, Manley P, Fabbro D, Meyer T, et al. Inhibition of mutant FLT3 receptors in leukemia cells by the small molecule tyrosine kinase inhibitor PKC412. Cancer Cell. 2002;1(5):433–43. https://doi.org/10.1016/s1535-6108(02)00069-7.
Levis M. Midostaurin approved for FLT3-mutated AML. Blood. 2017;129(26):3403–6. https://doi.org/10.1182/blood-2017-05-782292.
Stone RM, DeAngelo DJ, Klimek V, Galinsky I, Estey E, Nimer SD, et al. Patients with acute myeloid leukemia and an activating mutation in FLT3 respond to a small-molecule FLT3 tyrosine kinase inhibitor, PKC412. Blood. 2005;105(1):54–60. https://doi.org/10.1182/blood-2004-03-0891.
Fischer T, Stone RM, Deangelo DJ, Galinsky I, Estey E, Lanza C, et al. Phase IIB trial of oral Midostaurin (PKC412), the FMS-like tyrosine kinase 3 receptor (FLT3) and multi-targeted kinase inhibitor, in patients with acute myeloid leukemia and high-risk myelodysplastic syndrome with either wild-type or mutated FLT3. J Clin Oncol. 2010;28(28):4339–45. https://doi.org/10.1200/jco.2010.28.9678.
Furukawa Y, Vu HA, Akutsu M, Odgerel T, Izumi T, Tsunoda S, et al. Divergent cytotoxic effects of PKC412 in combination with conventional antileukemic agents in FLT3 mutation-positive versus -negative leukemia cell lines. Leukemia. 2007;21(5):1005–14. https://doi.org/10.1038/sj.leu.2404593.
Möllgård L, Deneberg S, Nahi H, Bengtzen S, Jonsson-Videsäter K, Fioretos T, et al. The FLT3 inhibitor PKC412 in combination with cytostatic drugs in vitro in acute myeloid leukemia. Cancer Chemother Pharmacol. 2008;62(3):439–48. https://doi.org/10.1007/s00280-007-0623-4.
Stone RM, Fischer T, Paquette R, Schiller G, Schiffer CA, Ehninger G, et al. Phase IB study of the FLT3 kinase inhibitor midostaurin with chemotherapy in younger newly diagnosed adult patients with acute myeloid leukemia. Leukemia. 2012;26(9):2061–8. https://doi.org/10.1038/leu.2012.115.
•• Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med. 2017;377(5):454–64. https://doi.org/10.1056/NEJMoa1614359. Reference 43 is the milestone study resulted in the approval of midostaurin as a first approved FLT3 inhibitor in newly diagnosed FLT3-mutated AML patients in combination with chemoherapy.
Larson RA, Mandrekar SJ, Huebner LJ, Sanford BL, Laumann K, Geyer S, et al. Midostaurin reduces relapse in FLT3-mutant acute myeloid leukemia: the Alliance CALGB 10603/RATIFY trial. Leukemia. 2021;35(9):2539–51. https://doi.org/10.1038/s41375-021-01179-4.
Zhang W, Konopleva M, Ruvolo VR, McQueen T, Evans RL, Bornmann WG, et al. Sorafenib induces apoptosis of AML cells via Bim-mediated activation of the intrinsic apoptotic pathway. Leukemia. 2008;22(4):808–18. https://doi.org/10.1038/sj.leu.2405098.
Lierman E, Lahortiga I, Van Miegroet H, Mentens N, Marynen P, Cools J. The ability of sorafenib to inhibit oncogenic PDGFRbeta and FLT3 mutants and overcome resistance to other small molecule inhibitors. Haematologica. 2007;92(1):27–34. https://doi.org/10.3324/haematol.10692.
Auclair D, Miller D, Yatsula V, Pickett W, Carter C, Chang Y, et al. Antitumor activity of sorafenib in FLT3-driven leukemic cells. Leukemia. 2007;21(3):439–45. https://doi.org/10.1038/sj.leu.2404508.
•• Burchert A, Bug G, Fritz LV, Finke J, Stelljes M, Röllig C, et al. Sorafenib maintenance after allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia with FLT3-internal tandem duplication mutation (SORMAIN). J Clin Oncol. 2020;38(26):2993–3002. https://doi.org/10.1200/jco.19.03345. Reference 48 explains the results of SORMAIN trial. 24-month OS and RFS was obtained when sorafenib maintenance was used as a maintenance therapy after allogeneic SCT in FLT3 ITD-mutated AML.
Ravandi F, Cortes JE, Jones D, Faderl S, Garcia-Manero G, Konopleva MY, et al. Phase I/II study of combination therapy with sorafenib, idarubicin, and cytarabine in younger patients with acute myeloid leukemia. J Clin Oncol. 2010;28(11):1856–62. https://doi.org/10.1200/jco.2009.25.4888.
Wei AH, Kennedy GA, Morris KL, Grigg A, He S, Schwarer A, et al. Results of a phase 2, randomized, double-blind study of sorafenib versus placebo in combination with intensive chemotherapy in previously untreated patients with FLT3-ITD acute myeloid leukemia (ALLG AMLM16). Blood. 2020;136:36–8. https://doi.org/10.1182/blood-2020-137334.
Tallman MS, Wang ES, Altman JK, Appelbaum FR, Bhatt VR, Bixby D, et al. Acute Myeloid Leukemia, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2019;17(6):721–49. https://doi.org/10.6004/jnccn.2019.0028.
Kawase T, Nakazawa T, Eguchi T, Tsuzuki H, Ueno Y, Amano Y, et al. Effect of Fms-like tyrosine kinase 3 (FLT3) ligand (FL) on antitumor activity of gilteritinib, a FLT3 inhibitor, in mice xenografted with FL-overexpressing cells. Oncotarget. 2019;10(58):6111–23. https://doi.org/10.18632/oncotarget.27222.
Perl AE, Larson RA, Podoltsev NA, Strickland S, Wang ES, Atallah E, et al. Follow-up of patients with R/R FLT3-mutation-positive AML treated with gilteritinib in the phase 3 ADMIRAL trial. Blood. 2022;139(23):3366–75. https://doi.org/10.1182/blood.2021011583.
•• Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, et al. Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med. 2019;381(18):1728–40. https://doi.org/10.1056/NEJMoa1902688. Reference 54 is the landmark ADMIRAL trial resulted in the approval of gilteritinib monotherapy in R/R FLT3-mutated AML by the FDA.
Zarrinkar PP, Gunawardane RN, Cramer MD, Gardner MF, Brigham D, Belli B, et al. AC220 is a uniquely potent and selective inhibitor of FLT3 for the treatment of acute myeloid leukemia (AML). Blood. 2009;114(14):2984–92. https://doi.org/10.1182/blood-2009-05-222034.
Chao Q, Sprankle KG, Grotzfeld RM, Lai AG, Carter TA, Velasco AM, et al. Identification of N-(5-tert-Butyl-isoxazol-3-yl)-N′-{4-[7-(2-morpholin-4-yl-ethoxy)imidazo[2,1-b][1,3]benzothiazol-2-yl]phenyl}urea Dihydrochloride (AC220), a uniquely potent, selective, and efficacious FMS-Like Tyrosine Kinase-3 (FLT3) Inhibitor. J Med Chem. 2009;52(23):7808–16. https://doi.org/10.1021/jm9007533.
•• Cortes JE, Khaled S, Martinelli G, Perl AE, Ganguly S, Russell N, et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019;20(7):984–97. https://doi.org/10.1016/s1470-2045(19)30150-0. Reference 57 explains the results of QUANTUM-R trial that showed improvement in OS of quizartinib monotherapy compared to salvage chemotherapy in R/R FLT3 ITD-mutated AML. However, quizartinib did not get the FDA approval due to some safety issues.
Ganguly S, Cortes JE, Krämer A, Levis MJ, Martinelli G, Perl AE, et al. Clinical outcomes in patients with FLT3-ITD-mutated relapsed/refractory acute myelogenous leukemia undergoing hematopoietic stem cell transplantation after quizartinib or salvage chemotherapy in the QuANTUM-R trial. Transplant Cell Ther. 2021;27(2):153–62. https://doi.org/10.1016/j.bbmt.2020.09.036.
US Food and Drug Administration. FDA approves quizartinib for newly diagnosed acute myeloid leukemia. 2023. https://www.fda.gov/drugs/drug-approvals-and-databases/fda-approves-quizartinib-newly-diagnosed-acute-myeloid-leukemia. Accessed 25 Feb 2024.
Jaiswal S, Fontanillas P, Flannick J, Manning A, Grauman PV, Mar BG, et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med. 2014;371(26):2488–98. https://doi.org/10.1056/NEJMoa1408617.
Abdel-Wahab O, Levine RL. Mutations in epigenetic modifiers in the pathogenesis and therapy of acute myeloid leukemia. Blood. 2013;121(18):3563–72. https://doi.org/10.1182/blood-2013-01-451781.
Conway O’Brien E, Prideaux S, Chevassut T. The epigenetic landscape of acute myeloid leukemia. Adv Hematol. 2014;2014:103175. https://doi.org/10.1155/2014/103175.
Suzuki MM, Bird A. DNA methylation landscapes: provocative insights from epigenomics. Nat Rev Genet. 2008;9(6):465–76. https://doi.org/10.1038/nrg2341.
Fong CY, Morison J, Dawson MA. Epigenetics in the hematologic malignancies. Haematologica. 2014;99(12):1772–83. https://doi.org/10.3324/haematol.2013.092007.
Benetatos L, Vartholomatos G. On the potential role of DNMT1 in acute myeloid leukemia and myelodysplastic syndromes: not another mutated epigenetic driver. Ann Hematol. 2016;95(10):1571–82. https://doi.org/10.1007/s00277-016-2636-8.
Benetatos L, Hatzimichael E, Dasoula A, Dranitsaris G, Tsiara S, Syrrou M, et al. CpG methylation analysis of the MEG3 and SNRPN imprinted genes in acute myeloid leukemia and myelodysplastic syndromes. Leuk Res. 2010;34(2):148–53. https://doi.org/10.1016/j.leukres.2009.06.019.
Aran D, Sabato S, Hellman A. DNA methylation of distal regulatory sites characterizes dysregulation of cancer genes. Genome Biol. 2013;14(3):R21. https://doi.org/10.1186/gb-2013-14-3-r21.
Zhang L, Padron E, Lancet J. The molecular basis and clinical significance of genetic mutations identified in myelodysplastic syndromes. Leuk Res. 2015;39(1):6–17. https://doi.org/10.1016/j.leukres.2014.10.006.
Figueroa ME, Lugthart S, Li Y, Erpelinck-Verschueren C, Deng X, Christos PJ, et al. DNA methylation signatures identify biologically distinct subtypes in acute myeloid leukemia. Cancer Cell. 2010;17(1):13–27. https://doi.org/10.1016/j.ccr.2009.11.020.
Hoang NM, Rui L. DNA methyltransferases in hematological malignancies. J Genet Genomics. 2020;47(7):361–72. https://doi.org/10.1016/j.jgg.2020.04.006.
Bestor TH, Ingram VM. Growth-dependent expression of multiple species of DNA methyltransferase in murine erythroleukemia cells. Proc Natl Acad Sci. 1985;82(9):2674–8. https://doi.org/10.1073/pnas.82.9.2674.
Okano M, Xie S, Li E. Cloning and characterization of a family of novel mammalian DNA (cytosine-5) methyltransferases [1]. Nat Genet. 1998;19(3):219–20. https://doi.org/10.1038/890.
Du Z, Song J, Wang Y, Zhao Y, Guda K, Yang S, et al. DNMT1 stability is regulated by proteins coordinating deubiquitination and acetylation-driven ubiquitination. Sci Signal. 2010;3(146):ra80–ra80. https://doi.org/10.1126/scisignal.2001462.
Bröske A-M, Vockentanz L, Kharazi S, Huska MR, Mancini E, Scheller M, et al. DNA methylation protects hematopoietic stem cell multipotency from myeloerythroid restriction. Nat Genet. 2009;41(11):1207–15. https://doi.org/10.1038/ng.463.
Tadokoro Y, Ema H, Okano M, Li E, Nakauchi H. De novo DNA methyltransferase is essential for self-renewal, but not for differentiation, in hematopoietic stem cells. J Exp Med. 2007;204(4):715–22. https://doi.org/10.1084/jem.20060750.
Bock C, Beerman I, Lien W-H, Smith Zachary D, Gu H, Boyle P, et al. DNA methylation dynamics during in vivo differentiation of blood and skin stem cells. Mol Cell. 2012;47(4):633–47. https://doi.org/10.1016/j.molcel.2012.06.019.
Ji H, Ehrlich LIR, Seita J, Murakami P, Doi A, Lindau P, et al. Comprehensive methylome map of lineage commitment from haematopoietic progenitors. Nature. 2010;467(7313):338–42. https://doi.org/10.1038/nature09367.
Trowbridge JJ, Snow JW, Kim J, Orkin SH. DNA methyltransferase 1 is essential for and uniquely regulates hematopoietic stem and progenitor cells. Cell Stem Cell. 2009;5(4):442–9. https://doi.org/10.1016/j.stem.2009.08.016.
Li M, Zhang D. DNA methyltransferase-1 in acute myeloid leukaemia: beyond the maintenance of DNA methylation. Ann Med. 2022;54(1):2011–23. https://doi.org/10.1080/07853890.2022.2099578.
An J, Ko M. Epigenetic modification of cytosines in hematopoietic differentiation and malignant transformation. Int J Mol Sci. 2023;24(2):1727.
Challen GA, Sun D, Jeong M, Luo M, Jelinek J, Berg JS, et al. Dnmt3a is essential for hematopoietic stem cell differentiation. Nat Genet. 2012;44(1):23–31. https://doi.org/10.1038/ng.1009.
Jeong M, Park HJ, Celik H, Ostrander EL, Reyes JM, Guzman A, et al. Loss of Dnmt3a immortalizes hematopoietic stem cells in vivo. Cell Rep. 2018;23(1):1–10. https://doi.org/10.1016/j.celrep.2018.03.025.
Chan SM, Majeti R. Role of DNMT3A, TET2, and IDH1/2 mutations in pre-leukemic stem cells in acute myeloid leukemia. Int J Hematol. 2013;98(6):648–57. https://doi.org/10.1007/s12185-013-1407-8.
Challen Grant A, Sun D, Mayle A, Jeong M, Luo M, Rodriguez B, et al. Dnmt3a and Dnmt3b have overlapping and distinct functions in hematopoietic stem cells. Cell Stem Cell. 2014;15(3):350–64. https://doi.org/10.1016/j.stem.2014.06.018.
Merry CR, Forrest ME, Sabers JN, Beard L, Gao X-H, Hatzoglou M, et al. DNMT1-associated long non-coding RNAs regulate global gene expression and DNA methylation in colon cancer. Hum Mol Genet. 2015;24(21):6240–53. https://doi.org/10.1093/hmg/ddv343.
Shukla V, Coumoul X, Lahusen T, Wang R-H, Xu X, Vassilopoulos A, et al. BRCA1 affects global DNA methylation through regulation of DNMT1. Cell Res. 2010;20(11):1201–15. https://doi.org/10.1038/cr.2010.128.
You H, Ding W, Rountree CB. Epigenetic regulation of cancer stem cell marker CD133 by transforming growth factor-beta. Hepatology. 2010;51(5):1635–44. https://doi.org/10.1002/hep.23544.
Ha K, Lee GE, Palii SS, Brown KD, Takeda Y, Liu K, et al. Rapid and transient recruitment of DNMT1 to DNA double-strand breaks is mediated by its interaction with multiple components of the DNA damage response machinery. Hum Mol Genet. 2010;20(1):126–40. https://doi.org/10.1093/hmg/ddq451.
Loughery JEP, Dunne PD, O’Neill KM, Meehan RR, McDaid JR, Walsh CP. DNMT1 deficiency triggers mismatch repair defects in human cells through depletion of repair protein levels in a process involving the DNA damage response. Hum Mol Genet. 2011;20(16):3241–55. https://doi.org/10.1093/hmg/ddr236.
Kim M, Trinh BN, Long TI, Oghamian S, Laird PW. Dnmt1 deficiency leads to enhanced microsatellite instability in mouse embryonic stem cells. Nucleic Acids Res. 2004;32(19):5742–9. https://doi.org/10.1093/nar/gkh912.
Di Croce L, Raker VA, Corsaro M, Fazi F, Fanelli M, Faretta M, et al. Methyltransferase recruitment and DNA hypermethylation of target promoters by an oncogenic transcription factor. Science. 2002;295(5557):1079–82. https://doi.org/10.1126/science.1065173.
Zhang Q, Wang HY, Marzec M, Raghunath PN, Nagasawa T, Wasik MA. STAT3- and DNA methyltransferase 1-mediated epigenetic silencing of SHP-1 tyrosine phosphatase tumor suppressor gene in malignant T lymphocytes. Proc Natl Acad Sci. 2005;102(19):6948–53. https://doi.org/10.1073/pnas.0501959102.
Suzuki M, Yamada T, Kihara-Negishi F, Sakurai T, Hara E, Tenen DG, et al. Site-specific DNA methylation by a complex of PU.1 and Dnmt3a/b. Oncogene. 2006;25(17):2477–88. https://doi.org/10.1038/sj.onc.1209272.
Mizuno S, Chijiwa T, Okamura T, Akashi K, Fukumaki Y, Niho Y, et al. Expression of DNA methyltransferases DNMT1, 3A, and 3B in normal hematopoiesis and in acute and chronic myelogenous leukemia. Blood. 2001;97(5):1172–9. https://doi.org/10.1182/blood.v97.5.1172.
Yang X, Wong MPM, Ng RK. Aberrant DNA methylation in acute myeloid leukemia and its clinical implications. Int J Mol Sci. 2019;20(18):4576.
Russler-Germain David A, Spencer David H, Young Margaret A, Lamprecht Tamara L, Miller Christopher A, Fulton R, et al. The R882H DNMT3A mutation associated with AML dominantly inhibits wild-type DNMT3A by blocking its ability to form active tetramers. Cancer Cell. 2014;25(4):442–54. https://doi.org/10.1016/j.ccr.2014.02.010.
Ley TJ, Ding L, Walter MJ, McLellan MD, Lamprecht T, Larson DE, et al. DNMT3A mutations in acute myeloid leukemia. N Engl J Med. 2010;363(25):2424–33. https://doi.org/10.1056/NEJMoa1005143.
Shlush LI, Zandi S, Mitchell A, Chen WC, Brandwein JM, Gupta V, et al. Identification of pre-leukaemic haematopoietic stem cells in acute leukaemia. Nature. 2014;506(7488):328–33. https://doi.org/10.1038/nature13038.
Sato H, Wheat JC, Steidl U, Ito K. DNMT3A and TET2 in the pre-leukemic phase of hematopoietic disorders. Front Oncol. 2016;6:187. https://doi.org/10.3389/fonc.2016.00187.
Zhang X, Zeng J, Zhou M, Li B, Zhang Y, Huang T, et al. The tumor suppressive role of miRNA-370 by targeting FoxM1 in acute myeloid leukemia. Mol Cancer. 2012;11:56. https://doi.org/10.1186/1476-4598-11-56.
Yang J. SALL4 as a transcriptional and epigenetic regulator in normal and leukemic hematopoiesis. Biomarker Research. 2018;6(1):1. https://doi.org/10.1186/s40364-017-0115-6.
Yang J, Corsello TR, Ma Y. Stem cell gene SALL4 suppresses transcription through recruitment of DNA methyltransferases. J Biol Chem. 2012;287(3):1996–2005. https://doi.org/10.1074/jbc.M111.308734.
Yang L, Liu L, Gao H, Pinnamaneni JP, Sanagasetti D, Singh VP, et al. The stem cell factor SALL4 is an essential transcriptional regulator in mixed lineage leukemia-rearranged leukemogenesis. J Hematol Oncol. 2017;10(1):159. https://doi.org/10.1186/s13045-017-0531-y.
Yan F, Shen N, Pang JX, Zhao N, Zhang YW, Bode AM, et al. A vicious loop of fatty acid-binding protein 4 and DNA methyltransferase 1 promotes acute myeloid leukemia and acts as a therapeutic target. Leukemia. 2018;32(4):865–73. https://doi.org/10.1038/leu.2017.307.
Al-Rawashde FA, Johan MF, Taib WRW, Ismail I, Johari SATT, Almajali B, et al. Thymoquinone inhibits growth of acute myeloid leukemia cells through reversal SHP-1 and SOCS-3 hypermethylation: In Vitro and In Silico Evaluation. Pharmaceuticals. 2021;14(12):1287.
Al-Jamal HAN, Mat Jusoh SA, Hassan R, Johan MF. Enhancing SHP-1 expression with 5-azacytidine may inhibit STAT3 activation and confer sensitivity in lestaurtinib (CEP-701)-resistant FLT3-ITD positive acute myeloid leukemia. BMC Cancer. 2015;15(1):869. https://doi.org/10.1186/s12885-015-1695-x.
Kowolik CM, Lin M, Xie J, Overman LE, Horne DA. NT1721, a novel epidithiodiketopiperazine, exhibits potent in vitro and in vivo efficacy against acute myeloid leukemia. Oncotarget. 2016;7:86186–97. https://doi.org/10.18632/oncotarget.13364.
Ramdas B, Lakshmi Reddy P, Mali RS, Pasupuleti SK, Zhang J, Kelley MR et al. Combined heterozygosity of FLT3ITD, TET2, and DNMT3A results in aggressive leukemia. JCI Insight. 2022;7(17). https://doi.org/10.1172/jci.insight.162016
Maifrede S, Le BV, Nieborowska-Skorska M, Golovine K, Sullivan-Reed K, Dunuwille WMB, et al. TET2 and DNMT3A mutations exert divergent effects on DNA repair and sensitivity of leukemia cells to PARP inhibitors. Cancer Res. 2021;81(19):5089–101. https://doi.org/10.1158/0008-5472.Can-20-3761.
Schemionek M, Kharabi Masouleh B, Klaile Y, Krug U, Hebestreit K, Schubert C, et al. Identification of the adapter molecule MTSS1 as a potential oncogene-specific tumor suppressor in acute myeloid leukemia. PLoS ONE. 2015;10(5):e0125783. https://doi.org/10.1371/journal.pone.0125783.
Figueroa ME, Abdel-Wahab O, Lu C, Ward PS, Patel J, Shih A, et al. Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype, disrupt TET2 function, and impair hematopoietic differentiation. Cancer Cell. 2010;18(6):553–67. https://doi.org/10.1016/j.ccr.2010.11.015.
Moran-Crusio K, Reavie L, Shih A, Abdel-Wahab O, Ndiaye-Lobry D, Lobry C, et al. Tet2 loss leads to increased hematopoietic stem cell self-renewal and myeloid transformation. Cancer Cell. 2011;20(1):11–24. https://doi.org/10.1016/j.ccr.2011.06.001.
Kunimoto H, Nakajima H. TET2: a cornerstone in normal and malignant hematopoiesis. Cancer Sci. 2021;112(1):31–40. https://doi.org/10.1111/cas.14688.
Tahiliani M, Koh KP, Shen Y, Pastor WA, Bandukwala H, Brudno Y, et al. Conversion of 5-methylcytosine to 5-hydroxymethylcytosine in mammalian DNA by MLL partner TET1. Science. 2009;324(5929):930–5. https://doi.org/10.1126/science.1170116.
Ito K, Lee J, Chrysanthou S, Zhao Y, Josephs K, Sato H, et al. Non-catalytic roles of Tet2 are essential to regulate hematopoietic stem and progenitor cell homeostasis. Cell Rep. 2019;28(10):2480-2490.e2484. https://doi.org/10.1016/j.celrep.2019.07.094.
Mellén M, Ayata P, Dewell S, Kriaucionis S, Heintz N. MeCP2 binds to 5hmC enriched within active genes and accessible chromatin in the nervous system. Cell. 2012;151(7):1417–30. https://doi.org/10.1016/j.cell.2012.11.022.
Spruijt CG, Gnerlich F, Smits AH, Pfaffeneder T, Jansen PW, Bauer C, et al. Dynamic readers for 5-(hydroxy)methylcytosine and its oxidized derivatives. Cell. 2013;152(5):1146–59. https://doi.org/10.1016/j.cell.2013.02.004.
Kafer GR, Li X, Horii T, Suetake I, Tajima S, Hatada I, et al. 5-Hydroxymethylcytosine marks sites of DNA damage and promotes genome stability. Cell Rep. 2016;14(6):1283–92. https://doi.org/10.1016/j.celrep.2016.01.035.
Chen LL, Lin HP, Zhou WJ, He CX, Zhang ZY, Cheng ZL, et al. SNIP1 Recruits TET2 to regulate c-MYC target genes and cellular DNA damage response. Cell Rep. 2018;25(6):1485-1500.e1484. https://doi.org/10.1016/j.celrep.2018.10.028.
An J, González-Avalos E, Chawla A, Jeong M, López-Moyado IF, Li W, et al. Acute loss of TET function results in aggressive myeloid cancer in mice. Nat Commun. 2015;6(1):10071. https://doi.org/10.1038/ncomms10071.
Lio CW, Zhang J, González-Avalos E, Hogan PG, Chang X, Rao A. Tet2 and Tet3 cooperate with B-lineage transcription factors to regulate DNA modification and chromatin accessibility. Elife. 2016;5. https://doi.org/10.7554/eLife.18290
Zhao Z, Chen L, Dawlaty MM, Pan F, Weeks O, Zhou Y, et al. Combined loss of Tet1 and Tet2 promotes B cell, but not myeloid malignancies, in mice. Cell Rep. 2015;13(8):1692–704. https://doi.org/10.1016/j.celrep.2015.10.037.
Pan F, Wingo TS, Zhao Z, Gao R, Makishima H, Qu G, et al. Tet2 loss leads to hypermutagenicity in haematopoietic stem/progenitor cells. Nat Commun. 2017;8:15102. https://doi.org/10.1038/ncomms15102.
Ding N, Bonham EM, Hannon BE, Amick TR, Baylin SB, O’Hagan HM. Mismatch repair proteins recruit DNA methyltransferase 1 to sites of oxidative DNA damage. J Mol Cell Biol. 2016;8(3):244–54. https://doi.org/10.1093/jmcb/mjv050.
O’Hagan HM, Wang W, Sen S, Destefano Shields C, Lee SS, Zhang YW, et al. Oxidative damage targets complexes containing DNA methyltransferases, SIRT1, and polycomb members to promoter CpG Islands. Cancer Cell. 2011;20(5):606–19. https://doi.org/10.1016/j.ccr.2011.09.012.
Tsagaratou A, González-Avalos E, Rautio S, Scott-Browne JP, Togher S, Pastor WA, et al. TET proteins regulate the lineage specification and TCR-mediated expansion of iNKT cells. Nat Immunol. 2017;18(1):45–53. https://doi.org/10.1038/ni.3630.
Rasmussen KD, Jia G, Johansen JV, Pedersen MT, Rapin N, Bagger FO, et al. Loss of TET2 in hematopoietic cells leads to DNA hypermethylation of active enhancers and induction of leukemogenesis. Genes Dev. 2015;29(9):910–22. https://doi.org/10.1101/gad.260174.115.
Ko M, Bandukwala HS, An J, Lamperti ED, Thompson EC, Hastie R, et al. Ten-Eleven-Translocation 2 (TET2) negatively regulates homeostasis and differentiation of hematopoietic stem cells in mice. Proc Natl Acad Sci. 2011;108(35):14566–71. https://doi.org/10.1073/pnas.1112317108.
Rasmussen KD, Berest I, Keβler S, Nishimura K, Simón-Carrasco L, Vassiliou GS, et al. TET2 binding to enhancers facilitates transcription factor recruitment in hematopoietic cells. Genome Res. 2019;29(4):564–75. https://doi.org/10.1101/gr.239277.118.
Tulstrup M, Soerensen M, Hansen JW, Gillberg L, Needhamsen M, Kaastrup K, et al. TET2 mutations are associated with hypermethylation at key regulatory enhancers in normal and malignant hematopoiesis. Nat Commun. 2021;12(1):6061. https://doi.org/10.1038/s41467-021-26093-2.
Sardina JL, Collombet S, Tian TV, Gómez A, Di Stefano B, Berenguer C, et al. Transcription factors drive Tet2-mediated enhancer demethylation to reprogram cell fate. Cell Stem Cell. 2018;23(5):727-741.e729. https://doi.org/10.1016/j.stem.2018.08.016.
Ko M, An J, Pastor WA, Koralov SB, Rajewsky K, Rao A. TET proteins and 5-methylcytosine oxidation in hematological cancers. Immunol Rev. 2015;263(1):6–21. https://doi.org/10.1111/imr.12239.
Haladyna JN, Yamauchi T, Neff T, Bernt KM. Epigenetic modifiers in normal and malignant hematopoiesis. Epigenomics. 2015;7(2):301–20. https://doi.org/10.2217/epi.14.88.
Kallin EM, Rodríguez-Ubreva J, Christensen J, Cimmino L, Aifantis I, Helin K, et al. Tet2 facilitates the derepression of myeloid target genes during CEBPα-induced transdifferentiation of pre-B cells. Mol Cell. 2012;48(2):266–76. https://doi.org/10.1016/j.molcel.2012.08.007.
van Oevelen C, Collombet S, Vicent G, Hoogenkamp M, Lepoivre C, Badeaux A, et al. C/EBPα activates pre-existing and de novo macrophage enhancers during induced pre-B cell transdifferentiation and myelopoiesis. Stem Cell Reports. 2015;5(2):232–47. https://doi.org/10.1016/j.stemcr.2015.06.007.
Suzuki T, Shimizu Y, Furuhata E, Maeda S, Kishima M, Nishimura H, et al. RUNX1 regulates site specificity of DNA demethylation by recruitment of DNA demethylation machineries in hematopoietic cells. Blood Adv. 2017;1(20):1699–711. https://doi.org/10.1182/bloodadvances.2017005710.
Izzo F, Lee SC, Poran A, Chaligne R, Gaiti F, Gross B, et al. DNA methylation disruption reshapes the hematopoietic differentiation landscape. Nat Genet. 2020;52(4):378–87. https://doi.org/10.1038/s41588-020-0595-4.
Li Z, Cai X, Cai C-L, Wang J, Zhang W, Petersen BE, et al. Deletion of Tet2 in mice leads to dysregulated hematopoietic stem cells and subsequent development of myeloid malignancies. Blood. 2011;118(17):4509–18. https://doi.org/10.1182/blood-2010-12-325241.
Roche-Lestienne C, Marceau A, Labis E, Nibourel O, Coiteux V, Guilhot J, et al. Mutation analysis of TET2, IDH1, IDH2 and ASXL1 in chronic myeloid leukemia. Leukemia. 2011;25(10):1661–4. https://doi.org/10.1038/leu.2011.139.
Kunimoto H, Fukuchi Y, Sakurai M, Sadahira K, Ikeda Y, Okamoto S, et al. Tet2 disruption leads to enhanced self-renewal and altered differentiation of fetal liver hematopoietic stem cells. Sci Rep. 2012;2(1):273. https://doi.org/10.1038/srep00273.
Song SJ, Ito K, Ala U, Kats L, Webster K, Sun SM, et al. The oncogenic microRNA miR-22 targets the TET2 tumor suppressor to promote hematopoietic stem cell self-renewal and transformation. Cell Stem Cell. 2013;13(1):87–101. https://doi.org/10.1016/j.stem.2013.06.003.
Ko M, An J, Bandukwala HS, Chavez L, Äijö T, Pastor WA, et al. Modulation of TET2 expression and 5-methylcytosine oxidation by the CXXC domain protein IDAX. Nature. 2013;497(7447):122–6. https://doi.org/10.1038/nature12052.
Rasmussen KD, Helin K. Role of TET enzymes in DNA methylation, development, and cancer. Genes Dev. 2016;30(7):733–50. https://doi.org/10.1101/gad.276568.115.
Joshi K, Zhang L, Breslin SJP, Kini AR, Zhang J. Role of TET dioxygenases in the regulation of both normal and pathological hematopoiesis. J Exp Clin Cancer Res. 2022;41(1):294. https://doi.org/10.1186/s13046-022-02496-x.
Huang H, Jiang X, Li Z, Li Y, Song CX, He C, et al. TET1 plays an essential oncogenic role in MLL-rearranged leukemia. Proc Natl Acad Sci U S A. 2013;110(29):11994–9. https://doi.org/10.1073/pnas.1310656110.
Nabil R, Hassan NM, Abdellateif MS, Gawdat RM, Elshazly SS. The prognostic role of C-KIT, TET1 and TET2 gene expression in acute myeloid leukemia. Mol Biol Rep. 2023;50(1):641–53. https://doi.org/10.1007/s11033-022-08000-0.
Jiang X, Hu C, Arnovitz S, Bugno J, Yu M, Zuo Z, et al. miR-22 has a potent anti-tumour role with therapeutic potential in acute myeloid leukaemia. Nat Commun. 2016;7(1):11452. https://doi.org/10.1038/ncomms11452.
Jiang X, Hu C, Ferchen K, Nie J, Cui X, Chen C-H, et al. Targeted inhibition of STAT/TET1 axis as a therapeutic strategy for acute myeloid leukemia. Nat Commun. 2017;8(1):2099. https://doi.org/10.1038/s41467-017-02290-w.
Pulikkottil AJ, Bamezai S, Ammer T, Mohr F, Feder K, Vegi NM, et al. TET3 promotes AML growth and epigenetically regulates glucose metabolism and leukemic stem cell associated pathways. Leukemia. 2022;36(2):416–25. https://doi.org/10.1038/s41375-021-01390-3.
Delhommeau F, Dupont S, Valle VD, James C, Trannoy S, Massé A, et al. Mutation in TET2 in myeloid cancers. N Engl J Med. 2009;360(22):2289–301. https://doi.org/10.1056/NEJMoa0810069.
Lazarenkov A, Sardina JL. Dissecting TET2 regulatory networks in blood differentiation and cancer. Cancers (Basel). 2022;14(3). https://doi.org/10.3390/cancers14030830
Shih Alan H, Jiang Y, Meydan C, Shank K, Pandey S, Barreyro L, et al. Mutational cooperativity linked to combinatorial epigenetic gain of function in acute myeloid leukemia. Cancer Cell. 2015;27(4):502–15. https://doi.org/10.1016/j.ccell.2015.03.009.
Corces-Zimmerman MR, Majeti R. Pre-leukemic evolution of hematopoietic stem cells: the importance of early mutations in leukemogenesis. Leukemia. 2014;28(12):2276–82. https://doi.org/10.1038/leu.2014.211.
Lin TL, Nagata Y, Kao HW, Sanada M, Okuno Y, Huang CF, et al. Clonal leukemic evolution in myelodysplastic syndromes with TET2 and IDH1/2 mutations. Haematologica. 2014;99(1):28–36. https://doi.org/10.3324/haematol.2013.091249.
Anderson NR, Sheth V, Li H, Harris MW, Qiu S, Crossman DK, et al. Microenvironmental CXCL12 deletion enhances Flt3-ITD acute myeloid leukemia stem cell response to therapy by reducing p38 MAPK signaling. Leukemia. 2023;37(3):560–70. https://doi.org/10.1038/s41375-022-01798-5.
Cai Z, Aguilera F, Ramdas B, Daulatabad SV, Srivastava R, Kotzin JJ, et al. Targeting bim via a lncRNA morrbid regulates the survival of preleukemic and leukemic cells. Cell Rep. 2020;31(12):107816. https://doi.org/10.1016/j.celrep.2020.107816.
Desikan SP, Daver N, DiNardo C, Kadia T, Konopleva M, Ravandi F. Resistance to targeted therapies: delving into FLT3 and IDH. Blood Cancer J. 2022;12(6):91. https://doi.org/10.1038/s41408-022-00687-5.
Dang L, Yen K, Attar EC. IDH mutations in cancer and progress toward development of targeted therapeutics. Ann Oncol. 2016;27(4):599–608. https://doi.org/10.1093/annonc/mdw013.
Cairns RA, Mak TW. Oncogenic isocitrate dehydrogenase mutations: mechanisms, models, and clinical opportunities. Cancer Discov. 2013;3(7):730–41. https://doi.org/10.1158/2159-8290.Cd-13-0083.
Gruber E, Kats LM. The curious case of IDH mutant acute myeloid leukaemia: biochemistry and therapeutic approaches. Biochem Soc Trans. 2023;51(4):1675–86. https://doi.org/10.1042/bst20230017.
Mg L, Boulay K, Topisirovic I, Huot M, Mallette FA. Oncogenic activities of IDH1/2 mutations: from epigenetics to cellular signaling. Trends Cell Biol. 2017;27(10):738–52. https://doi.org/10.1016/j.tcb.2017.06.002.
Loenarz C, Schofield CJ. Expanding chemical biology of 2-oxoglutarate oxygenases. Nat Chem Biol. 2008;4(3):152–6. https://doi.org/10.1038/nchembio0308-152.
Bleeker FE, Atai NA, Lamba S, Jonker A, Rijkeboer D, Bosch KS, et al. The prognostic IDH1( R132) mutation is associated with reduced NADP+-dependent IDH activity in glioblastoma. Acta Neuropathol. 2010;119(4):487–94. https://doi.org/10.1007/s00401-010-0645-6.
Fathi AT, Stein EM, DiNardo CD, Levis MJ, Montesinos P, de Botton S. Differentiation syndrome with lower-intensity treatments for acute myeloid leukemia. Am J Hematol. 2021;96(6):735–46. https://doi.org/10.1002/ajh.26142.
Montalban-Bravo G, DiNardo CD. The role of IDH mutations in acute myeloid leukemia. Future Oncol. 2018;14(10):979–93. https://doi.org/10.2217/fon-2017-0523.
Daver N, Wei AH, Pollyea DA, Fathi AT, Vyas P, DiNardo CD. New directions for emerging therapies in acute myeloid leukemia: the next chapter. Blood Cancer J. 2020;10(10):107. https://doi.org/10.1038/s41408-020-00376-1.
Madala HR, Punganuru SR, Arutla V, Misra S, Thomas TJ, Srivenugopal KS. Beyond brooding on oncometabolic havoc in IDH-mutant gliomas and AML: current and future therapeutic strategies. Cancers (Basel). 2018;10(2). https://doi.org/10.3390/cancers10020049
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009;462(7274):739–44. https://doi.org/10.1038/nature08617.
Lo Presti C, Fauvelle F, Jacob MC, Mondet J, Mossuz P. The metabolic reprogramming in acute myeloid leukemia patients depends on their genotype and is a prognostic marker. Blood Adv. 2021;5(1):156–66. https://doi.org/10.1182/bloodadvances.2020002981.
Lorsbach RB, Moore J, Mathew S, Raimondi SC, Mukatira ST, Downing JR. TET1, a member of a novel protein family, is fused to MLL in acute myeloid leukemia containing the t(10;11)(q22;q23). Leukemia. 2003;17(3):637–41. https://doi.org/10.1038/sj.leu.2402834.
Kernytsky A, Wang F, Hansen E, Schalm S, Straley K, Gliser C, et al. IDH2 mutation-induced histone and DNA hypermethylation is progressively reversed by small-molecule inhibition. Blood. 2015;125(2):296–303. https://doi.org/10.1182/blood-2013-10-533604.
Losman J-A, Looper RE, Koivunen P, Lee S, Schneider RK, McMahon C, et al. (<i>R</i>)-2-Hydroxyglutarate is sufficient to promote leukemogenesis and its effects are reversible. Science. 2013;339(6127):1621–5. https://doi.org/10.1126/science.1231677.
Wang F, Travins J, DeLaBarre B, Penard-Lacronique V, Schalm S, Hansen E, et al. Targeted inhibition of mutant IDH2 in leukemia cells induces cellular differentiation. Science. 2013;340(6132):622–6. https://doi.org/10.1126/science.1234769.
Chen C, Liu Y, Lu C, Cross JR, Morris JPt, Shroff AS, et al. Cancer-associated IDH2 mutants drive an acute myeloid leukemia that is susceptible to Brd4 inhibition. Genes Dev. 2013;27(18):1974–85. https://doi.org/10.1101/gad.226613.113.
Sasaki M, Knobbe CB, Munger JC, Lind EF, Brenner D, Brüstle A, et al. IDH1(R132H) mutation increases murine haematopoietic progenitors and alters epigenetics. Nature. 2012;488(7413):656–9. https://doi.org/10.1038/nature11323.
Chaturvedi A, Araujo Cruz MM, Jyotsana N, Sharma A, Yun H, Görlich K, et al. Mutant IDH1 promotes leukemogenesis in vivo and can be specifically targeted in human AML. Blood. 2013;122(16):2877–87. https://doi.org/10.1182/blood-2013-03-491571.
Kats LM, Reschke M, Taulli R, Pozdnyakova O, Burgess K, Bhargava P, et al. Proto-oncogenic role of mutant IDH2 in leukemia initiation and maintenance. Cell Stem Cell. 2014;14(3):329–41. https://doi.org/10.1016/j.stem.2013.12.016.
Rampal R, Alkalin A, Madzo J, Vasanthakumar A, Pronier E, Patel J, et al. DNA hydroxymethylation profiling reveals that WT1 mutations result in loss of TET2 function in acute myeloid leukemia. Cell Rep. 2014;9(5):1841–55. https://doi.org/10.1016/j.celrep.2014.11.004.
Wang Y, Xiao M, Chen X, Chen L, Xu Y, Lv L, et al. WT1 recruits TET2 to regulate its target gene expression and suppress leukemia cell proliferation. Mol Cell. 2015;57(4):662–73. https://doi.org/10.1016/j.molcel.2014.12.023.
Akalin A, Garrett-Bakelman FE, Kormaksson M, Busuttil J, Zhang L, Khrebtukova I, et al. Base-pair resolution DNA methylation sequencing reveals profoundly divergent epigenetic landscapes in acute myeloid leukemia. PLoS Genet. 2012;8(6): e1002781. https://doi.org/10.1371/journal.pgen.1002781.
Adan A. DNA methylation alterations in acute myeloid leukemia: therapeutic potential. In. Springer International Publishing, Cham. 2023. pp 1–28. https://doi.org/10.1007/16833_2023_192
Garrett-Bakelman FE, Melnick AM. Mutant IDH: a targetable driver of leukemic phenotypes linking metabolism, epigenetics and transcriptional regulation. Epigenomics. 2016;8(7):945–57. https://doi.org/10.2217/epi-2016-0008.
Chen JY, Lai YS, Tsai HJ, Kuo CC, Yen BL, Yeh SP, et al. The oncometabolite R-2-hydroxyglutarate activates NF-κB-dependent tumor-promoting stromal niche for acute myeloid leukemia cells. Sci Rep. 2016;6:32428. https://doi.org/10.1038/srep32428.
Boutzen H, Saland E, Larrue C, de Toni F, Gales L, Castelli FA, et al. Isocitrate dehydrogenase 1 mutations prime the all-trans retinoic acid myeloid differentiation pathway in acute myeloid leukemia. J Exp Med. 2016;213(4):483–97. https://doi.org/10.1084/jem.20150736.
Chan SM, Thomas D, Corces-Zimmerman MR, Xavy S, Rastogi S, Hong WJ, et al. Isocitrate dehydrogenase 1 and 2 mutations induce BCL-2 dependence in acute myeloid leukemia. Nat Med. 2015;21(2):178–84. https://doi.org/10.1038/nm.3788.
Zhan T, Rindtorff N, Boutros M. Wnt signaling in cancer. Oncogene. 2017;36(11):1461–73. https://doi.org/10.1038/onc.2016.304.
Meyer SE, Qin T, Muench DE, Masuda K, Venkatasubramanian M, Orr E, et al. DNMT3A haploinsufficiency transforms FLT3ITD myeloproliferative disease into a rapid, spontaneous, and fully penetrant acute myeloid leukemia. Cancer Discov. 2016;6(5):501–15. https://doi.org/10.1158/2159-8290.Cd-16-0008.
Yan XJ, Xu J, Gu ZH, Pan CM, Lu G, Shen Y, et al. Exome sequencing identifies somatic mutations of DNA methyltransferase gene DNMT3A in acute monocytic leukemia. Nat Genet. 2011;43(4):309–15. https://doi.org/10.1038/ng.788.
Thol F, Damm F, Lüdeking A, Winschel C, Wagner K, Morgan M, et al. Incidence and prognostic influence of DNMT3A mutations in acute myeloid leukemia. J Clin Oncol. 2011;29(21):2889–96. https://doi.org/10.1200/jco.2011.35.4894.
Chen M, Zeng Z, Li X, Qin W, Cai X, Chen S, et al. Clinical features and prognostic significance of DNMT3A, FLT3, and NPM1 mutations in de novo acute myeloid leukemia patients. Int J Lab Hematol. 2023;45(6):899–907. https://doi.org/10.1111/ijlh.14133.
Zhang Q, Wu X, Cao J, Gao F, Huang K. Association between increased mutation rates in DNMT3A and FLT3-ITD and poor prognosis of patients with acute myeloid leukemia. Exp Ther Med. 2019;18(4):3117–24. https://doi.org/10.3892/etm.2019.7891.
Lo MY, Tsai XC, Lin CC, Tien FM, Kuo YY, Lee WH, et al. Validation of the prognostic significance of the 2022 European LeukemiaNet risk stratification system in intensive chemotherapy treated aged 18 to 65 years patients with de novo acute myeloid leukemia. Am J Hematol. 2023;98(5):760–9. https://doi.org/10.1002/ajh.26892.
Tang F, Zhao X, Ruan G, Jiang Q, Jiang H, Xu L, et al. The effect of haploidentical hematopoietic stem cell transplantation on comutations based on next-generation sequencing in adult acute myeloid leukemia patients with the FLT3-ITD mutation. Hematol Oncol. 2023;41(4):733–42. https://doi.org/10.1002/hon.3186.
Elrhman H, El-Meligui YM, Elalawi SM. Prognostic impact of concurrent DNMT3A, FLT3 and NPM1 gene mutations in acute myeloid leukemia patients. Clin Lymphoma Myeloma Leuk. 2021;21(12):e960–9. https://doi.org/10.1016/j.clml.2021.07.011.
Ma J, Dunlap J, Paliga A, Traer E, Press R, Shen L, et al. DNMT3A co-mutation is required for FLT3-ITD as an adverse prognostic indicator in intermediate-risk cytogenetic group AML. Leuk Lymphoma. 2018;59(8):1938–48. https://doi.org/10.1080/10428194.2017.1397659.
Wakita S, Yamaguchi H, Omori I, Terada K, Ueda T, Manabe E, et al. Mutations of the epigenetics-modifying gene (DNMT3a, TET2, IDH1/2) at diagnosis may induce FLT3-ITD at relapse in de novo acute myeloid leukemia. Leukemia. 2013;27(5):1044–52. https://doi.org/10.1038/leu.2012.317.
Metzeler KH, Maharry K, Radmacher MD, Mrózek K, Margeson D, Becker H, et al. TET2 mutations improve the new European LeukemiaNet risk classification of acute myeloid leukemia: a Cancer and Leukemia Group B study. J Clin Oncol. 2011;29(10):1373–81. https://doi.org/10.1200/jco.2010.32.7742.
Ahn JS, Kim HJ, Kim YK, Jung SH, Yang DH, Lee JJ, et al. Adverse prognostic effect of homozygous TET2 mutation on the relapse risk of acute myeloid leukemia in patients of normal karyotype. Haematologica. 2015;100(9):e351-353. https://doi.org/10.3324/haematol.2015.126227.
Hou HA, Lin CC, Chou WC, Liu CY, Chen CY, Tang JL, et al. Integration of cytogenetic and molecular alterations in risk stratification of 318 patients with de novo non-M3 acute myeloid leukemia. Leukemia. 2014;28(1):50–8. https://doi.org/10.1038/leu.2013.236.
Patel JP, Gönen M, Figueroa ME, Fernandez H, Sun Z, Racevskis J, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012;366(12):1079–89. https://doi.org/10.1056/NEJMoa1112304.
Weissmann S, Alpermann T, Grossmann V, Kowarsch A, Nadarajah N, Eder C, et al. Landscape of TET2 mutations in acute myeloid leukemia. Leukemia. 2012;26(5):934–42. https://doi.org/10.1038/leu.2011.326.
Guan W, Zhou L, Li Y, Yang E, Liu Y, Lv N, et al. Profiling of somatic mutations and fusion genes in acute myeloid leukemia patients with FLT3-ITD or FLT3-TKD mutation at diagnosis reveals distinct evolutionary patterns. Exp Hematol Oncol. 2021;10(1):27. https://doi.org/10.1186/s40164-021-00207-4.
Green CL, Evans CM, Zhao L, Hills RK, Burnett AK, Linch DC, et al. The prognostic significance of IDH2 mutations in AML depends on the location of the mutation. Blood. 2011;118(2):409–12. https://doi.org/10.1182/blood-2010-12-322479.
DiNardo CD, Jabbour E, Ravandi F, Takahashi K, Daver N, Routbort M, et al. IDH1 and IDH2 mutations in myelodysplastic syndromes and role in disease progression. Leukemia. 2016;30(4):980–4. https://doi.org/10.1038/leu.2015.211.
DiNardo CD, Ravandi F, Agresta S, Konopleva M, Takahashi K, Kadia T, et al. Characteristics, clinical outcome, and prognostic significance of IDH mutations in AML. Am J Hematol. 2015;90(8):732–6. https://doi.org/10.1002/ajh.24072.
Patel KP, Ravandi F, Ma D, Paladugu A, Barkoh BA, Medeiros LJ, et al. Acute myeloid leukemia with IDH1 or IDH2 mutation: frequency and clinicopathologic features. Am J Clin Pathol. 2011;135(1):35–45. https://doi.org/10.1309/ajcpd7nr2rmnqdvf.
Getta BM, Devlin SM, Levine RL, Arcila ME, Mohanty AS, Zehir A, et al. Multicolor flow cytometry and multigene next-generation sequencing are complementary and highly predictive for relapse in acute myeloid leukemia after allogeneic transplantation. Biol Blood Marrow Transplant. 2017;23(7):1064–71. https://doi.org/10.1016/j.bbmt.2017.03.017.
Wiseman DH, Williams EL, Wilks DP, Sun Leong H, Somerville TD, Dennis MW, et al. Frequent reconstitution of IDH2(R140Q) mutant clonal multilineage hematopoiesis following chemotherapy for acute myeloid leukemia. Leukemia. 2016;30(9):1946–50. https://doi.org/10.1038/leu.2016.93.
Debarri H, Lebon D, Roumier C, Cheok M, Marceau-Renaut A, Nibourel O, et al. IDH1/2 but not DNMT3A mutations are suitable targets for minimal residual disease monitoring in acute myeloid leukemia patients: a study by the Acute Leukemia French Association. Oncotarget. 2015;6(39):42345–53. https://doi.org/10.18632/oncotarget.5645.
Xu Q, Li Y, Lv N, Jing Y, Xu Y, Li Y, et al. Correlation between isocitrate dehydrogenase gene aberrations and prognosis of patients with acute myeloid leukemia: a systematic review and meta-analysis. Clin Cancer Res. 2017;23(15):4511–22. https://doi.org/10.1158/1078-0432.Ccr-16-2628.
Boddu P, Takahashi K, Pemmaraju N, Daver N, Benton CB, Pierce S, et al. Influence of IDH on FLT3-ITD status in newly diagnosed AML. Leukemia. 2017;31(11):2526–9. https://doi.org/10.1038/leu.2017.244.
Navada SC, Steinmann J, Lübbert M, Silverman LR. Clinical development of demethylating agents in hematology. J Clin Invest. 2014;124(1):40–6. https://doi.org/10.1172/jci69739.
Leone G, Voso MT, Teofili L, Lübbert M. Inhibitors of DNA methylation in the treatment of hematological malignancies and MDS. Clin Immunol. 2003;109(1):89–102. https://doi.org/10.1016/s1521-6616(03)00207-9.
Pinto A, Attadia V, Fusco A, Ferrara F, Spada OA, Fiore PPD. 5-Aza-2’-deoxycytidine induces terminal differentiation of leukemic blasts from patients with acute myeloid leukemias. Blood. 1984;64(4):922–9. https://doi.org/10.1182/blood.V64.4.922.922.
Shih AH, Meydan C, Shank K, Garrett-Bakelman FE, Ward PS, Intlekofer AM, et al. Combination targeted therapy to disrupt aberrant oncogenic signaling and reverse epigenetic dysfunction in IDH2- and TET2-mutant acute myeloid leukemia. Cancer Discov. 2017;7(5):494–505. https://doi.org/10.1158/2159-8290.Cd-16-1049.
Hu X, Cai J, Zhu J, Lang W, Zhong J, Zhong H, et al. Modulation of FLT3 through decitabine-activated C/EBPa-PU.1 signal pathway in FLT3-ITD positive cells. Cell Signal. 2019;64:109409. https://doi.org/10.1016/j.cellsig.2019.109409.
Aumer T, Gremmelmaier CB, Runtsch LS, Pforr JC, Yeşiltaç GN, Kaiser S, et al. Comprehensive comparison between azacytidine and decitabine treatment in an acute myeloid leukemia cell line. Clin Epigenetics. 2022;14(1):113. https://doi.org/10.1186/s13148-022-01329-0.
Döhner H, Wei AH, Roboz GJ, Montesinos P, Thol FR, Ravandi F, et al. Prognostic impact of NPM1 and FLT3 mutations in patients with AML in first remission treated with oral azacitidine. Blood. 2022;140(15):1674–85. https://doi.org/10.1182/blood.2022016293.
Yu J, Peng Y, Wu L-C, Xie Z, Deng Y, Hughes T, et al. Curcumin down-regulates DNA methyltransferase 1 and plays an anti-leukemic role in acute myeloid leukemia. PLoS ONE. 2013;8(2):e55934. https://doi.org/10.1371/journal.pone.0055934.
Pang J, Shen N, Yan F, Zhao N, Dou L, Wu L-C et al. Thymoquinone exerts potent growth-suppressive activity on leukemia through DNA hypermethylation reversal in leukemia cells. Oncotarget. 2017;8(21):34453–67. https://doi.org/10.18632/oncotarget.16431.
Liu S, Liu Z, Xie Z, Pang J, Yu J, Lehmann E, et al. Bortezomib induces DNA hypomethylation and silenced gene transcription by interfering with Sp1/NF-κB–dependent DNA methyltransferase activity in acute myeloid leukemia. Blood. 2008;111(4):2364–73. https://doi.org/10.1182/blood-2007-08-110171.
McMurry H, Fletcher L, Traer E. IDH inhibitors in AML-promise and pitfalls. Curr Hematol Malig Rep. 2021;16(2):207–17. https://doi.org/10.1007/s11899-021-00619-3.
Yen K, Travins J, Wang F, David MD, Artin E, Straley K, et al. AG-221, a first-in-class therapy targeting acute myeloid leukemia harboring oncogenic idh2 mutations. Cancer Discov. 2017;7(5):478–93. https://doi.org/10.1158/2159-8290.Cd-16-1034.
Golub D, Iyengar N, Dogra S, Wong T, Bready D, Tang K, et al. Mutant isocitrate dehydrogenase inhibitors as targeted cancer therapeutics. Front Oncol. 2019;9:417. https://doi.org/10.3389/fonc.2019.00417.
Aiman W, Ali MA, Basit MA, Omar Z, Suleman M, Hassan M, et al. Efficacy and tolerability of isocitrate dehydrogenase inhibitors in patients with acute myeloid leukemia: a systematic review of clinical trials. Leuk Res. 2023;129:107077. https://doi.org/10.1016/j.leukres.2023.107077.
Wang D, Zheng L, Cheng BYL, Sin CF, Li R, Tsui SP, et al. Transgenic IDH2(R172K) and IDH2(R140Q) zebrafish models recapitulated features of human acute myeloid leukemia. Oncogene. 2023;42(16):1272–81. https://doi.org/10.1038/s41388-023-02611-y.
Williams CB, Kambhampati S, Fiskus W, Wick J, Dutreix C, Ganguly S, et al. Preclinical and phase I results of decitabine in combination with midostaurin (PKC412) for newly diagnosed elderly or relapsed/refractory adult patients with acute myeloid leukemia. Pharmacotherapy. 2013;33(12):1341–52. https://doi.org/10.1002/phar.1316.
Chang E, Ganguly S, Rajkhowa T, Gocke CD, Levis M, Konig H. The combination of FLT3 and DNA methyltransferase inhibition is synergistically cytotoxic to FLT3/ITD acute myeloid leukemia cells. Leukemia. 2016;30(5):1025–32. https://doi.org/10.1038/leu.2015.346.
Ueno Y, Mori M, Kamiyama Y, Saito R, Kaneko N, Isshiki E, et al. Evaluation of gilteritinib in combination with chemotherapy in preclinical models of FLT3-ITD(+) acute myeloid leukemia. Oncotarget. 2019;10(26):2530–45. https://doi.org/10.18632/oncotarget.26811.
Gill H, Man CH, Ip AH, Choi WW, Chow HC, Kwong YL, et al. Azacitidine as post-remission consolidation for sorafenib-induced remission of Fms-like tyrosine kinase-3 internal tandem duplication positive acute myeloid leukemia. Haematologica. 2015;100(7):e250-253. https://doi.org/10.3324/haematol.2014.123034.
Muppidi MR, Portwood S, Griffiths EA, Thompson JE, Ford LA, Freyer CW, et al. Decitabine and sorafenib therapy in FLT-3 ITD-mutant acute myeloid leukemia. Clin Lymphoma Myeloma Leuk. 2015;15(Suppl):S73-79. https://doi.org/10.1016/j.clml.2015.02.033.
Swaminathan M, Kantarjian HM, Levis M, Guerra V, Borthakur G, Alvarado Y, et al. A phase I/II study of the combination of quizartinib with azacitidine or low-dose cytarabine for the treatment of patients with acute myeloid leukemia and myelodysplastic syndrome. Haematologica. 2021;106(8):2121–30. https://doi.org/10.3324/haematol.2020.263392.
Sid S, Rey J, Charbonnier A, D’Incan E, Mohty B, Blaise D, et al. Treatment of Post-transplant relapse of FLT3-ITD mutated AML using 5-azacytidine and sorafenib bitherapy. Clin Lymphoma Myeloma Leuk. 2017;17(4):241–2. https://doi.org/10.1016/j.clml.2016.10.002.
Ravandi F, Alattar ML, Grunwald MR, Rudek MA, Rajkhowa T, Richie MA, et al. Phase 2 study of azacytidine plus sorafenib in patients with acute myeloid leukemia and FLT-3 internal tandem duplication mutation. Blood. 2013;121(23):4655–62. https://doi.org/10.1182/blood-2013-01-480228.
Ohanian M, Garcia-Manero G, Levis M, Jabbour E, Daver N, Borthakur G, et al. Sorafenib combined with 5-azacytidine in older patients with untreated FLT3-ITD mutated acute myeloid leukemia. Am J Hematol. 2018;93(9):1136–41. https://doi.org/10.1002/ajh.25198.
•• Wang ES, Montesinos P, Minden MD, Lee J-H, Heuser M, Naoe T, et al. Phase 3 trial of gilteritinib plus azacitidine vs azacitidine for newly diagnosed FLT3 mut+ AML ineligible for intensive chemotherapy. Blood. 2022;140(17):1845–57. https://doi.org/10.1182/blood.2021014586. Reference 236 explains the improved outcomes with the addition of gilteritinib to azacitidine in newly diagnosed, unfit patients.
Shoukier M, Kadia T, Konopleva M, Alotaibi AS, Alfayez M, Loghavi S, et al. Clinical characteristics and outcomes in patients with acute myeloid leukemia with concurrent FLT3-ITD and IDH mutations. Cancer. 2021;127(3):381–90. https://doi.org/10.1002/cncr.33293.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
A.A. and M.T. wrote the main manuscript text, M.T. prepared figures and A.A. and M.T prepared the tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tecik, M., Adan, A. Emerging DNA Methylome Targets in FLT3-ITD-Positive Acute Myeloid Leukemia: Combination Therapy with Clinically Approved FLT3 Inhibitors. Curr. Treat. Options in Oncol. (2024). https://doi.org/10.1007/s11864-024-01202-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s11864-024-01202-7