Opinion statement
Pathogenic germline variants in the setting of several associated cancer predisposition syndromes (CPS) may lead to the development of sarcoma. We would consider testing for a CPS in patients with a strong family history of cancer, multiple primary malignancies, and/or pediatric/adolescent/young adult patients diagnosed with other malignancies strongly associated with CPS. When a CPS is diagnosed in a patient with sarcoma, additional treatment considerations and imaging options for those patients are required. This applies particularly to the use of radiation therapy, ionizing radiation with diagnostic imaging, and the use of alkylating chemotherapy. As data and guidelines are currently lacking for many of these scenarios, we have adopted a shared decision-making process with patients and their families. If the best chance for cure in a patient with CPS requires utilization of radiation therapy or alkylating chemotherapy, we discuss the risks with the patient but do not omit these modalities. However, if there are treatment options that yield equivalent survival rates, yet avoid these modalities, we elect for those options. Considering staging imaging and post-therapy evaluation for sarcoma recurrence, we avoid surveillance techniques that utilize ionizing radiation when possible but do not completely omit them when their use is indicated.

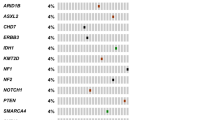
Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
• Vagher J, et al. Germline predisposition to soft tissue sarcoma. J Cancer Metastasis Treat. 2022;8:31. This reference is important as it has provided a detailed review of common soft tissue sarcomas related to cancer predisposition syndromes.
Zhang J, et al. Germline mutations in predisposition genes in pediatric cancer. N Engl J Med. 2015;373(24):2336–46.
Chavarri-Guerra Y, et al. Genetic cancer predisposition syndromes among older adults. J Geriatr Oncol. 2020;11(7):1054–60.
•• Kumamoto T, et al. Medical guidelines for Li–Fraumeni syndrome 2019, version 1.1. Int J Clin Oncol. 2021;26:2161–2178. This article is of major importance as it provides screening guidelines for LFS.
Vogt A, et al. Multiple primary tumours: challenges and approaches, a review. ESMO Open. 2017;2(2): e000172.
Li H, et al. Germline cancer predisposition variants in pediatric rhabdomyosarcoma: a report from the children’s oncology group. JNCI J Natl Cancer Inst. 2021;113(7):875–883.
Fair D, et al. TP53 germline pathogenic variant frequency in anaplastic rhabdomyosarcoma: A Children’s Oncology Group report. Pediatr Blood Cancer. 2023;70(9): e30413.
Schultz KAP, et al. DICER1 and associated conditions: identification of at-risk individuals and recommended surveillance strategies. Clin Cancer Res. 2018;24(10):2251–61.
Apellaniz-Ruiz M, McCluggage WG, Foulkes WD. DICER1-associated embryonal rhabdomyosarcoma and adenosarcoma of the gynecologic tract: pathology, molecular genetics, and indications for molecular testing. Genes Chromosomes Cancer. 2021;60(3):217–33.
Martin-Giacalone BA, et al. Pediatric Rhabdomyosarcoma: epidemiology and genetic susceptibility. J Clin Med. 2021;10(9):2028.
Miller RW, Rubinstein JH. Tumors in Rubinstein-Taybi syndrome. Am J Med Genet. 1995;56(1):112–5.
Mussa A, et al. Cancer risk in Beckwith-Wiedemann syndrome: a systematic review and meta-analysis outlining a novel (epi)genotype specific histotype targeted screening protocol. J Pediatr. 2016;176:142–149 e1.
Ducatman BS, et al. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer 1986;57(10):2006–21.
Wong WW, et al. Malignant peripheral nerve sheath tumor: analysis of treatment outcome. Int J Radiat Oncol Biol Phys. 1998;42(2):351–60.
Anghileri M, et al. Malignant peripheral nerve sheath tumors: prognostic factors and survival in a series of patients treated at a single institution. Cancer: Interdiscip Int J Am Cancer Soc. 2006;107(5):1065–1074.
Evans DG, et al. Malignant peripheral nerve sheath tumours in neurofibromatosis 1. J Med Genet. 2002;39(5):311–4.
Stucky CC, et al. Malignant peripheral nerve sheath tumors (MPNST): the Mayo Clinic experience. Ann Surg Oncol. 2012;19(3):878–85.
Evans DG, Huson SM, Birch JM. Malignant peripheral nerve sheath tumours in inherited disease. Clin Sarcoma Res. 2012;2(1):17.
Brohl AS, et al. Frequent inactivating germline mutations in DNA repair genes in patients with Ewing sarcoma. Genet Med. 2017;19(8):955–8.
Gillani R, et al. Germline predisposition to pediatric Ewing sarcoma is characterized by inherited pathogenic variants in DNA damage repair genes. Am J Hum Genet. 2022;109(6):1026–37.
Mirabello L, et al. Frequency of pathogenic germline variants in cancer-susceptibility genes in patients with osteosarcoma. JAMA Oncol. 2020;6(5):724–34.
Diessner BJ, et al. Nearly half of TP53 germline variants predicted to be pathogenic in patients with osteosarcoma are de novo: a report from the Children’s Oncology Group. JCO Precis Oncol. 2020;4:1187–95.
Calvert GT, et al. At-risk populations for osteosarcoma: the syndromes and beyond. Sarcoma. 2012;2012: 152382.
Wong FL, et al. Cancer incidence after retinoblastoma: radiation dose and sarcoma risk. JAMA. 1997;278(15):1262–7.
Bougeard G, et al. Revisiting Li-Fraumeni syndrome from TP53 mutation carriers. J Clin Oncol. 2015;33(21):2345–52.
Villani A, et al. Biochemical and imaging surveillance in germline TP53 mutation carriers with Li-Fraumeni syndrome: a prospective observational study. Lancet Oncol. 2011;12(6):559–67.
de Andrade KC, et al. Cancer incidence, patterns, and genotype-phenotype associations in individuals with pathogenic or likely pathogenic germline TP53 variants: an observational cohort study. Lancet Oncol. 2021;22(12):1787–98.
Kleinerman RA, et al. Risk of new cancers after radiotherapy in long-term survivors of retinoblastoma: an extended follow-up. J Clin Oncol. 2005;23(10):2272–9.
MacCarthy A, et al. Second and subsequent tumours among 1927 retinoblastoma patients diagnosed in Britain 1951–2004. Br J Cancer. 2013;108(12):2455–63.
Bright CJ, et al. Risk of soft-tissue sarcoma among 69 460 five-year survivors of childhood cancer in Europe. JNCI J Natl Cancer Inst. 2018;110(6): 649–660.
Kleinerman RA, et al. Risk of soft tissue sarcomas by individual subtype in survivors of hereditary retinoblastoma. J Natl Cancer Inst. 2007;99(1):24–31.
Hensley ML, et al. Genomic landscape of uterine sarcomas defined through prospective clinical sequencing. Clin Cancer Res. 2020;26(14):3881–8.
Jonsson P, et al. Tumour lineage shapes BRCA-mediated phenotypes. Nature. 2019;571(7766):576–9.
Kraft S, Fletcher CD. Atypical intradermal smooth muscle neoplasms: clinicopathologic analysis of 84 cases and a reappraisal of cutaneous “leiomyosarcoma.” Am J Surg Pathol. 2011;35(4):599–607.
Fallen T, et al. Desmoid tumors–a characterization of patients seen at Mayo Clinic 1976–1999. Fam Cancer. 2006;5(2):191–4.
Eaton KW, et al. Spectrum of SMARCB1/INI1 mutations in familial and sporadic rhabdoid tumors. Pediatr Blood Cancer. 2011;56(1):7–15.
Bourdeaut F, et al. Frequent hSNF5/INI1 germline mutations in patients with rhabdoid tumor. Clin Cancer Res. 2011;17(1):31–8.
Foulkes WD, et al. Cancer surveillance in Gorlin syndrome and rhabdoid tumor predisposition syndrome. Clin Cancer Res. 2017;23(12):e62–7.
Schneppenheim R, et al. Germline nonsense mutation and somatic inactivation of SMARCA4/BRG1 in a family with rhabdoid tumor predisposition syndrome. Am J Hum Genet. 2010;86(2):279–84.
Nemes K, Bens S, Bourdeaut F. Rhabdoid tumor predisposition syndrome, 2017 Dec 7. GeneReviews®[Internet]. Seattle: University of Washington; 1993.
Hirota S, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279(5350):577–80.
Ponti G, et al. Gastrointestinal stromal tumor and other primary metachronous or synchronous neoplasms as a suspicion criterion for syndromic setting. Oncol Rep. 2010;23(2):437–44.
Postow MA, Robson ME. Inherited gastrointestinal stromal tumor syndromes: mutations, clinical features, and therapeutic implications. Clin Sarcoma Res. 2012;2(1):16.
Chompret A, et al. PDGFRA germline mutation in a family with multiple cases of gastrointestinal stromal tumor. Gastroenterology. 2004;126(1):318–21.
Janeway KA, et al. Defects in succinate dehydrogenase in gastrointestinal stromal tumors lacking KIT and PDGFRA mutations. Proc Natl Acad Sci U S A. 2011;108(1):314–8.
Miettinen M, et al. Succinate dehydrogenase deficient gists–a clinicopathologic, immunohistochemical, and molecular genetic study of 66 gastric gists with predilection to young age. Am J Surg Pathol. 2011;35(11):1712.
Zoller ME, et al. Malignant and benign tumors in patients with neurofibromatosis type 1 in a defined Swedish population. Cancer. 1997;79(11):2125–31.
Yang XR, et al. T (brachyury) gene duplication confers major susceptibility to familial chordoma. Nat Genet. 2009;41(11):1176–8.
Parry DM, et al. Clinical findings in families with chordoma with and without T gene duplications and in patients with sporadic chordoma reported to the surveillance, epidemiology, and end results program. J Neurosurg. 2020;134(5):1399–408.
Kelley M, et al. Characterization of T gene sequence variants and germline duplications in familial and sporadic chordoma. Hum Genet. 2014;133(10):1289.
Pillay N, et al. A common single-nucleotide variant in T is strongly associated with chordoma. Nat Genet. 2012;44(11):1185–7.
Yepes S, et al. Rare germline variants in chordoma-related genes and chordoma susceptibility. Cancers. 2021;13(11):2704.
Young RJ, et al. Angiosarcoma. Lancet Oncol. 2010;11(10):983–91.
El Abiad JM, et al. Natural history of Ollier disease and Maffucci syndrome: patient survey and review of clinical literature. Am J Med Genet A. 2020;182(5):1093–103.
Blatt J, et al. Cancer risk in Klippel-Trenaunay syndrome. Lymphat Res Biol. 2019;17(6):630–6.
West JG, et al. BRCA mutations and the risk of angiosarcoma after breast cancer treatment. Clin Breast Cancer. 2008;8(6):533–7.
Kadouri L, et al. Genetic predisposition to radiation induced sarcoma: possible role for BRCA and p53 mutations. Breast Cancer Res Treat. 2013;140(1):207–11.
Calvete O, et al. The wide spectrum of POT1 gene variants correlates with multiple cancer types. Eur J Hum Genet. 2017;25(11):1278–81.
Calvete O, et al. A mutation in the POT1 gene is responsible for cardiac angiosarcoma in TP53-negative Li-Fraumeni-like families. Nat Commun. 2015;6:8383.
Anderson WJ, Doyle LA. Updates from the 2020 World Health Organization classification of soft tissue and bone tumours. Histopathology. 2021;78(5):644–57.
Frebourg T, et al. Guidelines for the Li-Fraumeni and heritable TP53-related cancer syndromes. Eur J Hum Genet. 2020;28(10):1379–86.
Hampel H, et al. A practice guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: referral indications for cancer predisposition assessment. Genet Med. 2015;17(1):70–87.
•• Waespe N, et al. Cancer predisposition syndromes as a risk factor for early second primary neoplasms after childhood cancer–a national cohort study. Eur J Cancer. 2021;145:71–80. This article is of major importance as it outlines the risks for secondary primary malignancies in pediatric patients in relation to their cancer predisposition syndrome.
Stiller CA, et al. Subsequent cancers within 5 years from initial diagnosis of childhood cancer. Patterns and risks in the population of Great Britain. Pediatr Blood Cancer 2023;70(5): e30258.
Eulo V, et al. Secondary sarcomas: biology, presentation, and clinical care. Am Soc Clin Oncol Educ Book. 2020;40:463–74.
•• Hendrickson PG, et al. Radiation therapy and secondary malignancy in Li‐Fraumeni syndrome: a hereditary cancer registry study. Cancer Med. 2020;9(21): 7954–7963. This article is of major importance as it proved radiation therapy does not significantly increase the risk for second primary malignancies induced by RT in patients with LFS.
Funato M, et al. Characteristics of Li-Fraumeni syndrome in Japan; a review study by the Special Committee of JSHT. Cancer Sci. 2021;112(7):2821–34.
Kasper E, et al. Contribution of genotoxic anticancer treatments to the development of multiple primary tumours in the context of germline TP53 mutations. Eur J Cancer. 2018;101:254–62.
• Clarke JE, et al. Radiologic screening and surveillance in hereditary cancers. Eur J Radiol Open. 2022;9: 100422. This article is of importance as it shows that imaging surveillance with whole body MRI is beneficial in patients with cancer predisposition syndromes.
Reid JR. Ionizing radiation use and cancer predisposition syndromes in children. J Am Coll Radiol. 2018;15(9):1238–9.
Author information
Authors and Affiliations
Contributions
CJM and JV are co-first authors
Corresponding author
Ethics declarations
Conflict of Interests
Jennie Vagher declares she has received payment or honoraria for participation in the National Society of Genetic Counselors AC.2022 and AAMDS Foundation 2023. Casey Mehrhoff declares she has no conflict of interest. Vaia Florou declares she has received consulting fees from Deciphera and Incyte. Luke Maese declares he has served as a consultant, received payment or honoraria for involvement with, and has participated on the Data Safety Monitoring or Advisory Board for Jazz Pharmaceuticals. Luke Maese also declares he has participated on the Data Safety Monitoring or Advisory Board for Servier Pharmaceuticals.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jennie Vagher and Casey J. Mehrhoff are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vagher, J., Mehrhoff, C.J., Florou, V. et al. Genetic Predisposition to Sarcoma: What Should Clinicians Know?. Curr. Treat. Options in Oncol. (2024). https://doi.org/10.1007/s11864-024-01192-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s11864-024-01192-6