Opinion statement
The vast majority of patients newly diagnosed with melanoma present with clinically localized disease, and sentinel lymph node biopsy (SLNB) is a standard of care in the management of these patients, particularly in intermediate thickness cases, in order to provide important prognostic data. However, SLNB also has an important role in the management of patients with other subtypes of melanoma such as thick melanomas, certain thin melanomas, and specific histologic variants of melanoma such as desmoplastic melanoma. Furthermore, there have been technical advances in the SLNB technique, such as the development of newer radiotracers and use of SPECT/CT, and there is some data to suggest performing a SLNB may be therapeutic. Finally, the management of patients with a positive sentinel lymph node (SLN) has undergone dramatic changes over the past several years based on the results of recent important clinical trials. Treatment options for patients with SLN metastases now include surveillance, completion lymph node dissection, and adjuvant therapy with checkpoint inhibitors and targeted therapy. SLNB continues to play a crucial role in the management of patients with melanoma, allowing for risk stratification, potential regional disease control, and further treatment options for patients with a positive SLN.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Ding S, Byrd DR, et al. Multivariate analysis of prognostic factors among 2,313 patients with stage III melanoma: comparison of nodal micrometastases versus macrometastases. J Clin Oncol. 2010;28(14):2452–9. https://doi.org/10.1200/JCO.2009.27.1627.
Morton DL, Cochran AJ, Thompson JF. The rationale for sentinel-node biopsy in primary melanoma. Nat Clin Pract Oncol. 2008;5(9):510–1. https://doi.org/10.1038/ncponc1205.
Gershenwald J. Melanoma of the skin. In: Amin MBES, Greene F, Byrd DR, Brookland RK, Washington MK, Gershenwald JE, Compton CC, Hess KR, Sullivan DC, Jessup JM, Brierley JD, Gaspar LE, Schilsky RL, Balch CM, Winchester DP, Asare DA, Madera M, Gress DM, Meyer LR, editors. AJCC cancer staging manual. Cham: Springer International; 2017. p. 563–85.
Coit DG, Thompson JA, Albertini MR, Barker C, Carson WE, Contreras C, et al. Cutaneous melanoma, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2019;17(4):367–402. https://doi.org/10.6004/jnccn.2019.0018.
Cascinelli N, Morabito A, Santinami M, MacKie RM, Belli F. Immediate or delayed dissection of regional nodes in patients with melanoma of the trunk: a randomised trial. WHO Melanoma Programme. Lancet. 1998;351(9105):793–6. https://doi.org/10.1016/s0140-6736(97)08260-3.
Morton DL, Wen DR, Wong JH, Economou JS, Cagle LA, Storm FK, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992;127(4):392–9. https://doi.org/10.1001/archsurg.1992.01420040034005.
Morton DL, Thompson JF, Cochran AJ, Mozzillo N, Nieweg OE, Roses DF, et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med. 2014;370(7):599–609. https://doi.org/10.1056/NEJMoa1310460.
Bigby M, Zagarella S, Sladden M, Popescu CM. Time to reconsider the role of sentinel lymph node biopsy in melanoma. J Am Acad Dermatol. 2019;80(4):1168–71. https://doi.org/10.1016/j.jaad.2018.11.026.
Delman KA, Wong SL. Completion node dissection after sentinel node biopsy in melanoma. JAMA Surg. 2018;153(11):1045–6. https://doi.org/10.1001/jamasurg.2018.1516.
•• Wong SL, Faries MB, Kennedy EB, Agarwala SS, Akhurst TJ, Ariyan C, et al. Sentinel lymph node biopsy and management of regional lymph nodes in melanoma: American Society of Clinical Oncology and Society of Surgical Oncology clinical practice guideline update. Ann Surg Oncol. 2018;25(2):356–77. https://doi.org/10.1245/s10434-017-6267-7. Provides key guidelines for the use of sentinel lymph node biopsy in melanoma and underlying data.
Criscione VD, Weinstock MA. Melanoma thickness trends in the United States, 1988-2006. J Invest Dermatol. 2010;130(3):793–7. https://doi.org/10.1038/jid.2009.328.
Sondak VK, Taylor JM, Sabel MS, Wang Y, Lowe L, Grover AC, et al. Mitotic rate and younger age are predictors of sentinel lymph node positivity: lessons learned from the generation of a probabilistic model. Ann Surg Oncol. 2004;11(3):247–58. https://doi.org/10.1245/aso.2004.03.044.
Bartlett EK, Gimotty PA, Sinnamon AJ, Wachtel H, Roses RE, Schuchter L, et al. Clark level risk stratifies patients with mitogenic thin melanomas for sentinel lymph node biopsy. Ann Surg Oncol. 2014;21(2):643–9. https://doi.org/10.1245/s10434-013-3313-y.
Han D, Yu D, Zhao X, Marzban SS, Messina JL, Gonzalez RJ, et al. Sentinel node biopsy is indicated for thin melanomas ≥0.76 mm. Ann Surg Oncol. 2012;19(11):3335–42. https://doi.org/10.1245/s10434-012-2469-1.
Han D, Zager JS, Shyr Y, Chen H, Berry LD, Iyengar S, et al. Clinicopathologic predictors of sentinel lymph node metastasis in thin melanoma. J Clin Oncol. 2013;31(35):4387–93. https://doi.org/10.1200/JCO.2013.50.1114.
Warycha MA, Zakrzewski J, Ni Q, Shapiro RL, Berman RS, Pavlick AC, et al. Meta-analysis of sentinel lymph node positivity in thin melanoma (≤1 mm). Cancer. 2009;115(4):869–79. https://doi.org/10.1002/cncr.24044.
McMasters KM, Noyes RD, Reintgen DS, Goydos JS, Beitsch PD, Davidson BS, et al. Lessons learned from the Sunbelt Melanoma Trial. J Surg Oncol. 2004;86(4):212–23. https://doi.org/10.1002/jso.20084.
Morton DL, Cochran AJ, Thompson JF, Elashoff R, Essner R, Glass EC, et al. Sentinel node biopsy for early-stage melanoma: accuracy and morbidity in MSLT-I, an international multicenter trial. Ann Surg. 2005;242(3):302–11; discussion 11-3. https://doi.org/10.1097/01.sla.0000181092.50141.fa.
Valsecchi ME, Silbermins D, de Rosa N, Wong SL, Lyman GH. Lymphatic mapping and sentinel lymph node biopsy in patients with melanoma: a meta-analysis. J Clin Oncol. 2011;29(11):1479–87. https://doi.org/10.1200/JCO.2010.33.1884.
Gajdos C, Griffith KA, Wong SL, Johnson TM, Chang AE, Cimmino VM, et al. Is there a benefit to sentinel lymph node biopsy in patients with T4 melanoma? Cancer. 2009;115(24):5752–60. https://doi.org/10.1002/cncr.24660.
Kachare SD, Singla P, Vohra NA, Zervos EE, Wong JH, Fitzgerald TL. Sentinel lymph node biopsy is prognostic but not therapeutic for thick melanoma. Surgery. 2015;158(3):662–8. https://doi.org/10.1016/j.surg.2015.05.012.
Ribero S, Osella-Abate S, Sanlorenzo M, Balagna E, Senetta R, Fierro MT, et al. Sentinel lymph node biopsy in thick-melanoma patients (N=350): what is its prognostic role? Ann Surg Oncol. 2015;22(6):1967–73. https://doi.org/10.1245/s10434-014-4211-7.
Scoggins CR, Bowen AL, Martin RC 2nd, Edwards MJ, Reintgen DS, Ross MI, et al. Prognostic information from sentinel lymph node biopsy in patients with thick melanoma. Arch Surg. 2010;145(7):622–7. https://doi.org/10.1001/archsurg.2010.115.
Ferrone CR, Panageas KS, Busam K, Brady MS, Coit DG. Multivariate prognostic model for patients with thick cutaneous melanoma: importance of sentinel lymph node status. Ann Surg Oncol. 2002;9(7):637–45. https://doi.org/10.1007/BF02574479.
• Han D, Han G, Duque MT, Morrison S, Leong SP, Kashani-Sabet M, et al. Sentinel lymph node biopsy is prognostic in thickest melanoma cases and should be performed for thick melanomas. Ann Surg Oncol. 2020;28:1007–16. https://doi.org/10.1245/s10434-020-08706-0. The largest study on thick melanoma which demonstrates the prognostic significance of and importance of performing sentinel lymph node biopsy in patients who present with clinically localized thick melanomas.
Han D, Han G, Morrison S, Leong SP, Kashani-Sabet M, Vetto J, et al. Factors predicting survival in thick melanoma: do all thick melanomas have the same prognosis? Surgery. 2020;168:518–26. https://doi.org/10.1016/j.surg.2020.04.048.
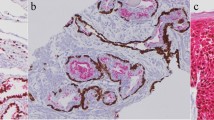
Nicolson NG, Han D. Desmoplastic melanoma. J Surg Oncol. 2019;119(2):208–15. https://doi.org/10.1002/jso.25317.
Busam KJ, Mujumdar U, Hummer AJ, Nobrega J, Hawkins WG, Coit DG, et al. Cutaneous desmoplastic melanoma: reappraisal of morphologic heterogeneity and prognostic factors. Am J Surg Pathol. 2004;28(11):1518–25. https://doi.org/10.1097/01.pas.0000141391.91677.a4.
Thelmo MC, Sagebiel RW, Treseler PA, Morita ET, Nguyen LH, Kashani-Sabet M, et al. Evaluation of sentinel lymph node status in spindle cell melanomas. J Am Acad Dermatol. 2001;44(3):451–5. https://doi.org/10.1067/mjd.2001.110881.
Han D, Zager JS, Yu D, Zhao X, Walls B, Marzban SS, et al. Desmoplastic melanoma: is there a role for sentinel lymph node biopsy? Ann Surg Oncol. 2013;20(7):2345–51. https://doi.org/10.1245/s10434-013-2883-z.
Pawlik TM, Ross MI, Prieto VG, Ballo MT, Johnson MM, Mansfield PF, et al. Assessment of the role of sentinel lymph node biopsy for primary cutaneous desmoplastic melanoma. Cancer. 2006;106(4):900–6. https://doi.org/10.1002/cncr.21635.
Dixon A, Steinman H, Anderson S, Nirenberg A, Dixon J. Routine usage of sentinel node biopsy in melanoma management must cease. Br J Dermatol. 2016;175(6):1340–1. https://doi.org/10.1111/bjd.14769.
El Sharouni MA, Witkamp AJ, Sigurdsson V, van Diest PJ. Trends in sentinel lymph node biopsy enactment for cutaneous melanoma. Ann Surg Oncol. 2019;26(5):1494–502. https://doi.org/10.1245/s10434-019-07204-2.
• Murtha TD, Han G, Han D. Predictors for use of sentinel node biopsy and the association with improved survival in melanoma patients who have nodal staging. Ann Surg Oncol. 2018;34(4):903–11. https://doi.org/10.1245/s10434-018-6348-2. This study analyzed rates of performing sentinel lymph node biopsy in eligible patients and factors associated with not performing nodal staging in eligible patients; 68.2% of patients with intermediate thickness melanoma and 52.6% of patients with thick melanoma were treated with sentinel node biopsy, demonstrating that measures are needed to improve adherence to melanoma treatment guidelines.
Gershenwald JE, Colome MI, Lee JE, Mansfield PF, Tseng C, Lee JJ, et al. Patterns of recurrence following a negative sentinel lymph node biopsy in 243 patients with stage I or II melanoma. J Clin Oncol. 1998;16(6):2253–60. https://doi.org/10.1200/JCO.1998.16.6.2253.
Gershenwald JE, Thompson W, Mansfield PF, Lee JE, Colome MI, Tseng CH, et al. Multi-institutional melanoma lymphatic mapping experience: the prognostic value of sentinel lymph node status in 612 stage I or II melanoma patients. J Clin Oncol. 1999;17(3):976–83. https://doi.org/10.1200/JCO.1999.17.3.976.
Essner R, Conforti A, Kelley MC, Wanek L, Stern S, Glass E, et al. Efficacy of lymphatic mapping, sentinel lymphadenectomy, and selective complete lymph node dissection as a therapeutic procedure for early-stage melanoma. Ann Surg Oncol. 1999;6(5):442–9. https://doi.org/10.1007/s10434-999-0442-4.
McMasters KM, Reintgen DS, Ross MI, Gershenwald JE, Edwards MJ, Sober A, et al. Sentinel lymph node biopsy for melanoma: controversy despite widespread agreement. J Clin Oncol. 2001;19(11):2851–5. https://doi.org/10.1200/JCO.2001.19.11.2851.
Doepker MP, Thompson ZJ, Harb JN, Messina JL, Puleo CA, Egan KM, et al. Dermal melanoma: a report on prognosis, outcomes, and the utility of sentinel lymph node biopsy. J Surg Oncol. 2016;113(1):98–102. https://doi.org/10.1002/jso.24088.
Pavri SN, Han G, Khan S, Han D. Does sentinel lymph node status have prognostic significance in patients with acral lentiginous melanoma? J Surg Oncol. 2019;119(8):1060–9. https://doi.org/10.1002/jso.25445.
Kim J, Sun Z, Gulack BC, Adam MA, Mosca PJ, Rice HE, et al. Sentinel lymph node biopsy is a prognostic measure in pediatric melanoma. J Pediatr Surg. 2016;51(6):986–90. https://doi.org/10.1016/j.jpedsurg.2016.02.067.
Ellis MC, Weerasinghe R, Corless CL, Vetto JT. Sentinel lymph node staging of cutaneous melanoma: predictors and outcomes. Am J Surg. 2010;199(5):663–8. https://doi.org/10.1016/j.amjsurg.2010.01.019.
White RL Jr, Ayers GD, Stell VH, Ding S, Gershenwald JE, Salo JC, et al. Factors predictive of the status of sentinel lymph nodes in melanoma patients from a large multicenter database. Ann Surg Oncol. 2011;18(13):3593–600. https://doi.org/10.1245/s10434-011-1826-9.
Karakousis GC, Gimotty PA, Leong SP, Pockaj BA, White RL, O'Donoghue C, et al. Microsatellitosis in patients with melanoma. Ann Surg Oncol. 2019;26(1):33–41. https://doi.org/10.1245/s10434-018-7006-4.
Gerami P, Cook RW, Russell MC, Wilkinson J, Amaria RN, Gonzalez R, et al. Gene expression profiling for molecular staging of cutaneous melanoma in patients undergoing sentinel lymph node biopsy. J Am Acad Dermatol. 2015;72(5):780–5 e3. https://doi.org/10.1016/j.jaad.2015.01.009.
Gerami P, Cook RW, Wilkinson J, Russell MC, Dhillon N, Amaria RN, et al. Development of a prognostic genetic signature to predict the metastatic risk associated with cutaneous melanoma. Clin Cancer Res. 2015;21(1):175–83. https://doi.org/10.1158/1078-0432.CCR-13-3316.
Vetto JT, Hsueh EC, Gastman BR, Dillon LD, Monzon FA, Cook RW, et al. Guidance of sentinel lymph node biopsy decisions in patients with T1-T2 melanoma using gene expression profiling. Future Oncol. 2019;15(11):1207–17. https://doi.org/10.2217/fon-2018-0912.
Gershenwald JE, Andtbacka RH, Prieto VG, Johnson MM, Diwan AH, Lee JE, et al. Microscopic tumor burden in sentinel lymph nodes predicts synchronous nonsentinel lymph node involvement in patients with melanoma. J Clin Oncol. 2008;26(26):4296–303. https://doi.org/10.1200/JCO.2007.15.4179.
Murali R, Desilva C, Thompson JF, Scolyer RA. Non-sentinel node risk score (N-SNORE): a scoring system for accurately stratifying risk of non-sentinel node positivity in patients with cutaneous melanoma with positive sentinel lymph nodes. J Clin Oncol. 2010;28(29):4441–9. https://doi.org/10.1200/JCO.2010.30.9567.
van Akkooi AC, Nowecki ZI, Voit C, Schafer-Hesterberg G, Michej W, de Wilt JH, et al. Sentinel node tumor burden according to the Rotterdam criteria is the most important prognostic factor for survival in melanoma patients: a multicenter study in 388 patients with positive sentinel nodes. Ann Surg. 2008;248(6):949–55. https://doi.org/10.1097/SLA.0b013e31818fefe0.
Starz H, Siedlecki K, Balda BR. Sentinel lymphonodectomy and s-classification: a successful strategy for better prediction and improvement of outcome of melanoma. Ann Surg Oncol. 2004;11(3 Suppl):162S–8S. https://doi.org/10.1007/BF02523622.
Dewar DJ, Newell B, Green MA, Topping AP, Powell BW, Cook MG. The microanatomic location of metastatic melanoma in sentinel lymph nodes predicts nonsentinel lymph node involvement. J Clin Oncol. 2004;22(16):3345–9. https://doi.org/10.1200/JCO.2004.12.177.
Uhara H, Yamazaki N, Takata M, Inoue Y, Sakakibara A, Nakamura Y, et al. Applicability of radiocolloids, blue dyes and fluorescent indocyanine green to sentinel node biopsy in melanoma. J Dermatol. 2012;39(4):336–8. https://doi.org/10.1111/j.1346-8138.2011.01340.x.
Liu LC, Parrett BM, Jenkins T, Lee W, Morita E, Treseler P, et al. Selective sentinel lymph node dissection for melanoma: importance of harvesting nodes with lower radioactive counts without the need for blue dye. Ann Surg Oncol. 2011;18(10):2919–24. https://doi.org/10.1245/s10434-011-1689-0.
Hu Y, Melmer PD, Slingluff CL Jr. Localization of the sentinel lymph node in melanoma without blue dye. Ann Surg. 2016;263(3):588–92. https://doi.org/10.1097/SLA.0000000000001187.
McMasters KM, Reintgen DS, Ross MI, Wong SL, Gershenwald JE, Krag DN, et al. Sentinel lymph node biopsy for melanoma: how many radioactive nodes should be removed? Ann Surg Oncol. 2001;8(3):192–7. https://doi.org/10.1007/s10434-001-0192-4.
Sondak VK, King DW, Zager JS, Schneebaum S, Kim J, Leong SP, et al. Combined analysis of phase III trials evaluating [99mTc]tilmanocept and vital blue dye for identification of sentinel lymph nodes in clinically node-negative cutaneous melanoma. Ann Surg Oncol. 2013;20(2):680–8. https://doi.org/10.1245/s10434-012-2612-z.
Leong SP, Kim J, Ross M, Faries M, Scoggins CR, Metz WL, et al. A phase 2 study of (99m)Tc-tilmanocept in the detection of sentinel lymph nodes in melanoma and breast cancer. Ann Surg Oncol. 2011;18(4):961–9. https://doi.org/10.1245/s10434-010-1524-z.
Wallace AM, Hoh CK, Limmer KK, Darrah DD, Schulteis G, Vera DR. Sentinel lymph node accumulation of Lymphoseek and Tc-99m-sulfur colloid using a “2-day” protocol. Nucl Med Biol. 2009;36(6):687–92. https://doi.org/10.1016/j.nucmedbio.2009.04.007.
Unkart JT, Baker JL, Hosseini A, Hoh CK, Wallace MS, Vera DR, et al. Comparison of post-injection site pain between technetium sulfur colloid and technetium tilmanocept in breast cancer patients undergoing sentinel lymph node biopsy. Ann Surg Oncol. 2015;22(Suppl 3):S559–65. https://doi.org/10.1245/s10434-015-4802-y.
Cloyd JM, Wapnir IL, Read BM, Swetter S, Greco RS. Indocyanine green and fluorescence lymphangiography for sentinel lymph node identification in cutaneous melanoma. J Surg Oncol. 2014;110(7):888–92. https://doi.org/10.1002/jso.23745.
Murakami K, Kotani Y, Suzuki A, Takaya H, Nakai H, Matsuki M, et al. Superparamagnetic iron oxide as a tracer for sentinel lymph node detection in uterine cancer: a pilot study. Sci Rep. 2020;10(1):7945. https://doi.org/10.1038/s41598-020-64926-0.
Pouw JJ, Grootendorst MR, Bezooijen R, Klazen CA, De Bruin WI, Klaase JM, et al. Pre-operative sentinel lymph node localization in breast cancer with superparamagnetic iron oxide MRI: the SentiMAG Multicentre Trial imaging subprotocol. Br J Radiol. 2015;88(1056):20150634. https://doi.org/10.1259/bjr.20150634.
Rubio IT, Rodriguez-Revuelto R, Espinosa-Bravo M, Siso C, Rivero J, Esgueva A. A randomized study comparing different doses of superparamagnetic iron oxide tracer for sentinel lymph node biopsy in breast cancer: the SUNRISE study. Eur J Surg Oncol. 2020;46:2195–201. https://doi.org/10.1016/j.ejso.2020.06.018.
Taruno K, Kurita T, Kuwahata A, Yanagihara K, Enokido K, Katayose Y, et al. Multicenter clinical trial on sentinel lymph node biopsy using superparamagnetic iron oxide nanoparticles and a novel handheld magnetic probe. J Surg Oncol. 2019;120(8):1391–6. https://doi.org/10.1002/jso.25747.
Brouwer OR, Buckle T, Vermeeren L, Klop WM, Balm AJ, van der Poel HG, et al. Comparing the hybrid fluorescent-radioactive tracer indocyanine green-99mTc-nanocolloid with 99mTc-nanocolloid for sentinel node identification: a validation study using lymphoscintigraphy and SPECT/CT. J Nucl Med. 2012;53(7):1034–40. https://doi.org/10.2967/jnumed.112.103127.
Polom K, Murawa D, Nowaczyk P, Rho YS, Murawa P. Breast cancer sentinel lymph node mapping using near infrared guided indocyanine green and indocyanine green--human serum albumin in comparison with gamma emitting radioactive colloid tracer. Eur J Surg Oncol. 2012;38(2):137–42. https://doi.org/10.1016/j.ejso.2011.11.004.
Forte S, Kubik-Huch RA, Leo C. Improvement in breast magnetic resonance imaging after a sentinel procedure for breast cancer with superparamagnetic tracers. Eur J Radiol Open. 2019;6:215–9. https://doi.org/10.1016/j.ejro.2019.05.006.
Zhang L, Huang Y, Yang C, Zhu T, Lin Y, Gao H, et al. Application of a carbon nanoparticle suspension for sentinel lymph node mapping in patients with early breast cancer: a retrospective cohort study. World J Surg Oncol. 2018;16(1):112. https://doi.org/10.1186/s12957-018-1414-6.
Even-Sapir E, Lerman H, Lievshitz G, Khafif A, Fliss DM, Schwartz A, et al. Lymphoscintigraphy for sentinel node mapping using a hybrid SPECT/CT system. J Nucl Med. 2003;44(9):1413–20.
Kretschmer L, Altenvoerde G, Meller J, Zutt M, Funke M, Neumann C, et al. Dynamic lymphoscintigraphy and image fusion of SPECT and pelvic CT-scans allow mapping of aberrant pelvic sentinel lymph nodes in malignant melanoma. Eur J Cancer. 2003;39(2):175–83. https://doi.org/10.1016/s0959-8049(02)00534-8.
Veenstra HJ, Vermeeren L, Olmos RA, Nieweg OE. The additional value of lymphatic mapping with routine SPECT/CT in unselected patients with clinically localized melanoma. Ann Surg Oncol. 2012;19(3):1018–23. https://doi.org/10.1245/s10434-011-2031-6.
Stoffels I, Boy C, Poppel T, Kuhn J, Klotgen K, Dissemond J, et al. Association between sentinel lymph node excision with or without preoperative SPECT/CT and metastatic node detection and disease-free survival in melanoma. JAMA. 2012;308(10):1007–14. https://doi.org/10.1001/2012.jama.11030.
Vermeeren L, Valdes Olmos RA, Meinhardt W, Bex A, van der Poel HG, Vogel WV, et al. Intraoperative radioguidance with a portable gamma camera: a novel technique for laparoscopic sentinel node localisation in urological malignancies. Eur J Nucl Med Mol Imaging. 2009;36(7):1029–36. https://doi.org/10.1007/s00259-009-1100-6.
Carlson GW, Page AJ, Cohen C, Parker D, Yaar R, Li A, et al. Regional recurrence after negative sentinel lymph node biopsy for melanoma. Ann Surg. 2008;248(3):378–86. https://doi.org/10.1097/SLA.0b013e3181855718.
Sondak VK, Zager JS. Who is to blame for false-negative sentinel node biopsies in melanoma? Ann Surg Oncol. 2010;17(3):670–3. https://doi.org/10.1245/s10434-009-0857-y.
Thomas DC, Han G, Leong SP, Kashani-Sabet M, Vetto J, Pockaj B, et al. Recurrence of melanoma after a negative sentinel node biopsy: predictors and impact of recurrence site on survival. Ann Surg Oncol. 2019;26(7):2254–62. https://doi.org/10.1245/s10434-019-07369-w.
Sinnamon AJ, Neuwirth MG, Bartlett EK, Zaheer S, Etherington MS, Xu X, et al. Predictors of false negative sentinel lymph node biopsy in trunk and extremity melanoma. J Surg Oncol. 2017;116(7):848–55. https://doi.org/10.1002/jso.24743.
Yushak M, Mehnert J, Luke J, Poklepovic A. Approaches to high-risk resected stage II and III melanoma. Am Soc Clin Oncol Educ Book. 2019;39:e207–e11. https://doi.org/10.1200/EDBK_239283.
NIH. Safety and efficacy of pembrolizumab compared to placebo in resected high-risk stage II melanoma (MK-3475-716/KEYNOTE-716). 2018. https://clinicaltrials.gov/ct2/show/NCT03553836. Accessed Oct 2020.
NIH. Adjuvant nivolumab treatment in stage II (IIA, IIB, IIC) high-risk melanoma (NivoMela). 2020.
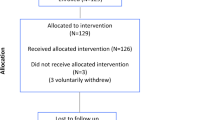
•• Faries MB, Thompson JF, Cochran AJ, Andtbacka RH, Mozzillo N, Zager JS, et al. Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med. 2017;376(23):2211–22. https://doi.org/10.1056/NEJMoa1613210. Fundamental study which demonstrated that completion lymph node dissection in patients with melanoma and a positive sentinel node biopsy did not improve survival over observation of the involved nodal basin.
Bamboat ZM, Konstantinidis IT, Kuk D, Ariyan CE, Brady MS, Coit DG. Observation after a positive sentinel lymph node biopsy in patients with melanoma. Ann Surg Oncol. 2014;21(9):3117–23. https://doi.org/10.1245/s10434-014-3758-7.
Lee DY, Lau BJ, Huynh KT, Flaherty DC, Lee JH, Stern SL, et al. Impact of completion lymph node dissection on patients with positive sentinel lymph node biopsy in melanoma. J Am Coll Surg. 2016;223(1):9–18. https://doi.org/10.1016/j.jamcollsurg.2016.01.045.
Wong SL, Morton DL, Thompson JF, Gershenwald JE, Leong SP, Reintgen DS, et al. Melanoma patients with positive sentinel nodes who did not undergo completion lymphadenectomy: a multi-institutional study. Ann Surg Oncol. 2006;13(6):809–16. https://doi.org/10.1245/ASO.2006.03.058.
Klemen ND, Han G, Leong SP, Kashani-Sabet M, Vetto J, White R, et al. Completion lymphadenectomy for a positive sentinel node biopsy in melanoma patients is not associated with a survival benefit. J Surg Oncol. 2019;119(8):1053–9. https://doi.org/10.1002/jso.25444.
Leiter U, Stadler R, Mauch C, Hohenberger W, Brockmeyer N, Berking C, et al. Complete lymph node dissection versus no dissection in patients with sentinel lymph node biopsy positive melanoma (DeCOG-SLT): a multicentre, randomised, phase 3 trial. Lancet Oncol. 2016;17(6):757–67. https://doi.org/10.1016/S1470-2045(16)00141-8.
Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23. https://doi.org/10.1056/NEJMoa1003466.
Eggermont AM, Chiarion-Sileni V, Grob JJ, Dummer R, Wolchok JD, Schmidt H, et al. Prolonged survival in stage III melanoma with ipilimumab adjuvant therapy. N Engl J Med. 2016;375(19):1845–55. https://doi.org/10.1056/NEJMoa1611299.
•• Weber J, Mandala M, Del Vecchio M, Gogas HJ, Arance AM, Cowey CL, et al. Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med. 2017;377(19):1824–35. https://doi.org/10.1056/NEJMoa1709030. Study demonstrated that adjuvant treatment with the anti-PD-1 agent nivolumab after resection of stage III or IV melanoma improved recurrence-free survival and led to the FDA approval of this agent as adjuvant therapy.
Yokota K, Uchi H, Uhara H, Yoshikawa S, Takenouchi T, Inozume T, et al. Adjuvant therapy with nivolumab versus ipilimumab after complete resection of stage III/IV melanoma: Japanese subgroup analysis from the phase 3 CheckMate 238 study. J Dermatol. 2019;46(12):1197–201. https://doi.org/10.1111/1346-8138.15103.
•• AMM E, Blank CU, Mandala M, Long GV, Atkinson V, Dalle S, et al. Adjuvant pembrolizumab versus placebo in resected stage III melanoma. N Engl J Med. 2018;378(19):1789–801. https://doi.org/10.1056/NEJMoa1802357. Study demonstrated that adjuvant treatment with the anti-PD-1 agent pembrolizumab after resection of stage III melanoma improved recurrence-free survival and led to the FDA approval of this agent as adjuvant therapy.
•• Long GV, Hauschild A, Santinami M, Atkinson V, Mandala M, Chiarion-Sileni V, et al. Adjuvant dabrafenib plus trametinib in stage III BRAF-mutated melanoma. N Engl J Med. 2017;377(19):1813–23. https://doi.org/10.1056/NEJMoa1708539. Study demonstrated that adjuvant treatment with targeted therapy using dabrafenib with trametinib after resection of stage III melanoma improved recurrence-free survival and led to the FDA approval of this agent as adjuvant therapy.
• Standage H, Hersh AR, Caughey A, Taylor M, Vetto J, Han D. What is the cost-effective treatment for melanoma patients with a positive sentinel node? Ann Surg Oncol. 2020. https://doi.org/10.1245/s10434-020-09137-7. First study to analyze the cost-effectiveness of the multiple treatment options for positive sentinel lymph node patients, including nodal observation, completion lymph node dissection, completion lymph node dissection with adjuvant pembrolizumab, and adjuvant pembrolizumab alone. This was also the first study to assess adjuvant systemic therapy alone for a positive sentinel lymph node biopsy without prior treatment with completion lymph node dissection. Although adjuvant pembrolizumab alone had the highest-quality adjusted life years, nodal observation was the only cost-effective treatment strategy for a positive sentinel lymph node, given the high cost of pembrolizumab.
Wright BE, Scheri RP, Ye X, Faries MB, Turner RR, Essner R, et al. Importance of sentinel lymph node biopsy in patients with thin melanoma. Arch Surg. 2008;143(9):892–9; discussion 9-900. https://doi.org/10.1001/archsurg.143.9.892.
Yonick DV, Ballo RM, Kahn E, Dahiya M, Yao K, Godellas C, et al. Predictors of positive sentinel lymph node in thin melanoma. Am J Surg. 2011;201(3):324–7; discussion 7-8. https://doi.org/10.1016/j.amjsurg.2010.09.011.
Murali R, Haydu LE, Quinn MJ, Saw RP, Shannon K, Spillane AJ, et al. Sentinel lymph node biopsy in patients with thin primary cutaneous melanoma. Ann Surg. 2012;255(1):128–33. https://doi.org/10.1097/SLA.0b013e3182306c72.
Mozzillo N, Pennacchioli E, Gandini S, Caraco C, Crispo A, Botti G, et al. Sentinel node biopsy in thin and thick melanoma. Ann Surg Oncol. 2013;20(8):2780–6. https://doi.org/10.1245/s10434-012-2826-0.
Venna SS, Thummala S, Nosrati M, Leong SP, Miller JR 3rd, Sagebiel RW, et al. Analysis of sentinel lymph node positivity in patients with thin primary melanoma. J Am Acad Dermatol. 2013;68(4):560–7. https://doi.org/10.1016/j.jaad.2012.08.045.
Maurichi A, Miceli R, Camerini T, Mariani L, Patuzzo R, Ruggeri R, et al. Prediction of survival in patients with thin melanoma: results from a multi-institution study. J Clin Oncol. 2014;32(23):2479–85. https://doi.org/10.1200/JCO.2013.54.2340.
Mitteldorf C, Bertsch HP, Jung K, Thoms KM, Schon MP, Tronnier M, et al. Sentinel node biopsy improves prognostic stratification in patients with thin (pT1) melanomas and an additional risk factor. Ann Surg Oncol. 2014;21(7):2252–8. https://doi.org/10.1245/s10434-014-3641-6.
Durham AB, Schwartz JL, Lowe L, Zhao L, Johnson AG, Harms KL, et al. The natural history of thin melanoma and the utility of sentinel lymph node biopsy. J Surg Oncol. 2017;116(8):1185–92. https://doi.org/10.1002/jso.24765.
Piazzalunga D, Ceresoli M, Allievi N, Ribero S, Quaglino P, Di Lorenzo S, et al. Can sentinel node biopsy be safely omitted in thin melanoma? Risk factor analysis of 1272 multicenter prospective cases. Eur J Surg Oncol. 2019;45(5):820–4. https://doi.org/10.1016/j.ejso.2018.11.022.
Santos FMD, Silva FCD, Pedron J, Furian RD, Fortes C, Bonamigo RR. Association between tumor-infiltrating lymphocytes and sentinel lymph node positivity in thin melanoma. An Bras Dermatol. 2019;94(1):47–51. https://doi.org/10.1590/abd1806-4841.20197414.
Tejera-Vaquerizo A, Ribero S, Puig S, Boada A, Paradela S, Moreno-Ramirez D, et al. Survival analysis and sentinel lymph node status in thin cutaneous melanoma: a multicenter observational study. Cancer Med. 2019;8(9):4235–44. https://doi.org/10.1002/cam4.2358.
Kocsis A, Karsko L, Kurgyis Z, Besenyi Z, Pavics L, Dosa-Racz E, et al. Is it necessary to perform sentinel lymph node biopsy in thin melanoma? A retrospective single center analysis. Pathol Oncol Res. 2020;26(3):1861–8. https://doi.org/10.1007/s12253-019-00769-z.
White I, Fortino J, Curti B, Vetto J. Clinical impact of sentinel lymph node biopsy in patients with thick (>4 mm) melanomas. Am J Surg. 2014;207(5):702–7; discussion 7. https://doi.org/10.1016/j.amjsurg.2013.12.022.
Yamamoto M, Fisher KJ, Wong JY, Koscso JM, Konstantinovic MA, Govsyeyev N, et al. Sentinel lymph node biopsy is indicated for patients with thick clinically lymph node-negative melanoma. Cancer. 2015;121(10):1628–36. https://doi.org/10.1002/cncr.29239.
Bello DM, Han G, Jackson L, Bulloch K, Ariyan S, Narayan D, et al. The prognostic significance of sentinel lymph node status for patients with thick melanoma. Ann Surg Oncol. 2016;23(Suppl 5):938–45. https://doi.org/10.1245/s10434-016-5502-y.
Boada A, Tejera-Vaquerizo A, Ribero S, Puig S, Moreno-Ramirez D, Quaglino P, et al. Factors associated with sentinel lymph node status and prognostic role of completion lymph node dissection for thick melanoma. Eur J Surg Oncol. 2020;46(2):263–71. https://doi.org/10.1016/j.ejso.2019.09.189.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Steven Morrison declares that he has no conflict of interest. Dale Han declares that he has no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Skin Cancer
Rights and permissions
About this article
Cite this article
Morrison, S., Han, D. Re-evaluation of Sentinel Lymph Node Biopsy for Melanoma. Curr. Treat. Options in Oncol. 22, 22 (2021). https://doi.org/10.1007/s11864-021-00819-2
Accepted:
Published:
DOI: https://doi.org/10.1007/s11864-021-00819-2