Abstract
Purpose
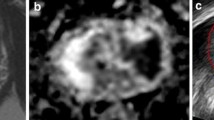
Multiparametric MRI and the transperineal approach have become standard in the diagnostic pathway for suspected prostate cancer. Targeting of MRI lesions is performed at most centers, but the routine use of systematic cores is controversial. We aim to assess the value of obtaining systematic cores in patients undergoing cognitive fusion targeted double-freehand transperineal prostate biopsy.
Materials and methods
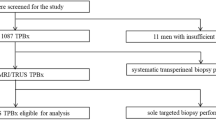
Patients who underwent a cognitive fusion, freehand TPB at a single tertiary urology service (Perth, Australia) between November 2020 and November 2021 were retrospectively reviewed. Patients were included if they were biopsy naive and had a clinical suspicion of prostate cancer, based on their mpMRI results. Both targeted and systematic cores were taken at the time of their biopsy.
Results
One hundred forty patients suited the selection criteria. Clinically significant cancer was identified in 63% of patients. Of those that had clinically significant cancer, the target lesion identified 91% of the disease, missing 9% of patients whom the target biopsy detected non-clinically significant cancer but was identified in the systematic cores. Higher PI-RADS category patients were also found to be associated with an increasing likelihood of identifying clinically significant cancer within the target.
Conclusions
In patients with PI-RADS 3 and higher, the target biopsy can miss up to 9% of clinically significant cancer. Systematic cores can add value as they can also change management by identifying a high-risk disease where only intermediate cancer was identified in the target. A combination of targeted and systematic cores is still required to detect cancer.

Similar content being viewed by others
Data Availability
Data is available on request.
References
Filson CP, Natarajan S, Margolis DJ et al (2016) Prostate cancer detection with magnetic resonance-ultrasound fusion biopsy: the role of systematic and targeted biopsies. Cancer 122(6):884–892
Ekwueme K, Simpson H, Zakhour H, Parr NJ (2013) Transperineal template-guided saturation biopsy using a modified technique: outcome of 270 cases requiring repeat prostate biopsy. BJU Int 111(8):E365–E373
Hansen N, Patruno G, Wadhwa K et al (2016) Magnetic resonance and ultrasound image fusion supported transperineal prostate biopsy using the Ginsburg protocol: technique, learning points, and biopsy results. Eur Urol 70(2):332–340
Kasivisvanathan V, Rannikko AS, Borghi M et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378(19):1767–1777
Ahmed HU, Bosaily AE-S, Brown LC et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389(10071):815–22
Siddiqui MM, Rais-Bahrami S, Turkbey B et al (2015) Comparison of MR/ultrasound fusion–guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 313(4):390–397
NICE Guidance (2019) Prostate cancer: diagnosis and management. BJU Int 124:9–26
Mottet N, Bellmunt J, Bolla M et al (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Euro Urol 71(4):618–29
Bjurlin MA, Carroll PR, Eggener S et al (2020) Update of the standard operating procedure on the use of multiparametric magnetic resonance imaging for the diagnosis, staging and management of prostate cancer. J Urol 203(4):706–712
Rouvière O, Puech P, Renard-Penna R et al (2019) Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): a prospective, multicentre, paired diagnostic study. Lancet Oncol 20(1):100–109
Elkhoury FF, Felker ER, Kwan L et al (2019) Comparison of targeted vs systematic prostate biopsy in men who are biopsy naive: the prospective assessment of image registration in the diagnosis of prostate cancer (PAIREDCAP) study. JAMA Surg 154(9):811–818
Neale A, Stroman L, Kum F et al (2020) Targeted and systematic cognitive freehand-guided transperineal biopsy: is there still a role for systematic biopsy? BJU Int 126(2):280–285
Ahdoot M, Wilbur AR, Reese SE et al (2020) MRI-targeted, systematic, and combined biopsy for prostate cancer diagnosis. N Engl J Med 382(10):917–928
Madej A, Wilkosz J, Różański W, Lipiński M (2012) Complication rates after prostate biopsy according to the number of sampled cores. Cent European J Urol 65(3):116
Song G, Ruan M, Wang H et al (2020) How many targeted biopsy cores are needed for clinically significant prostate cancer detection during transperineal magnetic resonance imaging ultrasound fusion biopsy? J Urol 204(6):1202–1208
Lu A, Amirkhiz KG, Nguyen K et al (2018) MP77-07 How many cores are needed to detect clinically significant prostate cancer on targeted MRI-ultrasound fusion biopsy? J Urol 199(4S):e1029–e1030
Sonmez G, Demirtas T, Tombul ST et al (2020) What is the ideal number of biopsy cores per lesion in targeted prostate biopsy? Prostate International 8(3):112–115
Kenigsberg AP, Renson A, Rosenkrantz AB et al (2018) Optimizing the number of cores targeted during prostate magnetic resonance imaging fusion target biopsy. Eur Urol Oncol 1(5):418–425
Hu Z, Wang J, Sun D et al (2019) How many cores does systematic prostate biopsy need?: a large-sample retrospective analysis. J Ultrasound Med 38(6):1491–1499
Schaufler C, Daigle R, Singhaviranon S et al (2022) How many cores are enough? Optimizing the transperineal prostate biopsy template. Urologic Oncology: Seminars and Original Investigations Elsevier. https://www.sciencedirect.com/science/article/abs/pii/S1078143921005469
Berg S, Tully KH, von Landenberg N et al (2021) How many cores should be sampled during systematic prostate biopsy in case of negative multiparametric magnetic resonance imaging? Analysis of 274 Men with Clinical Suspicion of Prostate Cancer. Urol Int 1–6. https://karger.com/uin/article-abstract/106/9/914/827182/How-Many-Cores-Should-Be-Sampled-during-Systematic?redirectedFrom=fulltext
Author information
Authors and Affiliations
Contributions
M. Barns: data collection, data analysis, and manuscript editing. O. Barratt: data collection. M. Chau: project development, data collection, data analysis, and manuscript writing/editing. M. Kuan: data collection and manuscript editing. K. McDermott: data collection and manuscript editing. P. Teloken: project development, data collection, and manuscript editing.
Corresponding author
Ethics declarations
Ethical approval
Ethical approval for this study was obtained from Sir Charles Gairdner Hospital (GEKO ID: 42421). Informed consent was not sought for the present study because of its retrospective nature, requiring only the review of database. All information and data was de-identified. The IRB waived the requirements for informed consent due to the retrospective nature.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chau, M., Barns, M., Barratt, O. et al. Are systematic prostate biopsy still necessary in biopsy naive men?. Ir J Med Sci (2024). https://doi.org/10.1007/s11845-024-03637-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11845-024-03637-1