Abstract
Aim
The aim of this audit was to assess the effect of new guidelines on virtual triage referrals to an Irish eye emergency department (EED) during the COVID-19 pandemic.
Methods
A retrospective phone triage referral and clinical note audit was performed to assess outcomes of phone triaging in October. Guidelines for phone triage were formulated with particular regard to what conditions should be seen in EED, treated over the phone or sent straight to outpatients clinic or minor procedures. A prospective phone triage referral and case note audit was then done to assess outcomes after introduction of the guidelines in November.
Results
A total of 1700 patients were referred to the eye emergency department, 861 in October and 839 in November. A total of 577 patients were triaged for in-person EED review in November, compared to 692 prior to implementation of guidelines (p < 0.05). The number of patients referred straight to outpatients (p < 0.05) and treated over the phone (p < 0.05) was also significantly increased. Ultimately, the number of conditions unnecessarily triaged to EED, as per the guidelines implemented, was significantly reduced (p < 0.05).
Conclusion
This audit addressed the need to reduce footfall during the COVID-19 pandemic, identified suitable avenues of referrals for certain conditions, and demonstrated that these guidelines significantly reduced the number of patients presenting to EED with conditions amenable to phone review or clinic follow-up.
Similar content being viewed by others
Introduction
Severe acute respiratory syndrome coronavirus 2 (COVID-19) has had a profound impact on the delivery of healthcare across all sectors and disciplines of medicine and surgery. Its implications upon ophthalmology, one of the busiest outpatient services in Ireland and worldwide, have been wide-ranging. Ophthalmology is a high-risk specialty with large clinic volumes and close-proximity examinations [1]. Managing patients in a safe, effective, and timely way to avoid delays in treatment and subsequent morbidity in the acute waves of the pandemic resulted in rapid expansion of telemedicine services [2]. Telemedicine was not an entirely new concept in ophthalmology with up to 50% of UK-based eye departments utilising virtual glaucoma clinics in 2018 [3]. However, it had a rapidly expanded role in response to the pandemic and in particular in acute eye services.
The Mater Misericordiae University Hospital’s dedicated eye emergency department (EED) services a catchment of over 1 million people. Since the onset of the COVID-19 pandemic, all patients referred to the Mater EED have been triaged virtually before coming to the EED. This consists of a phone call between an ophthalmologist or ophthalmic-trained nurse and the patient and/or referrer with the option of sending photos for review of external or anterior segment pathologies. A detailed referral form is then completed and uploaded to the EED database.
The aim of this audit was to assess the effect of new standardised guidelines on virtual triage referrals to an Irish eye emergency department (EED) during the COVID-19 pandemic in an attempt to streamline the process and reduce unnecessary footfall. The implementation of an efficient and effective telemedicine referral could have applications beyond the pandemic in improving resource allocation and planning of future eye service provisions.
Methods
The first phase of the audit involved a retrospective review of all phone triage referral forms from October 2021. In cases where the patient was following virtual triage referred into the EED for face to face consultation, the clinical notes from each consultation were also assessed. An electronic database was established to record a pre-determined, standardised set of data for each unique patient referral. This included patient demographics (age, gender, and location), diagnosis, and referral outcomes. It was documented whether the patient was brought to EED and, if so, how many visits to the EED they had and whether they were subsequently referred to the outpatients department (OPD). It was also noted if patients were treated over the phone or referred directly to OPD or for a minor procedure. Patients were excluded if the patient had been seen in the previous month to limit reviews and focus solely on new presentations.
Formulation + implementation of the guidelines
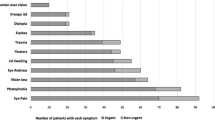
Phone triaging was initiated at the onset of the pandemic with EED guidelines on conditions available in conjunction with whole departmental changes in light of the pandemic. To improve the triaging process as part of the audit cycle, streamlined guidelines were formulated in collaboration with the ophthalmology sub-specialties to identify appropriate referral pathways for different conditions. This involved the creation of a clear one-page referral chart which was to be displayed in all clinical rooms. Conditions requiring review in EED are found in Fig. 1 and conditions amenable to outpatients’ referral are found in Fig. 2. This list is non-exhaustive and certain conditions amenable for outpatients, such as cataracts or posterior capsular opacification, were triaged based on severity and impact on functioning in addition to the detail of the referral. The hospital’s catchment area was also clearly displayed in the referral chart.
The guidelines were introduced on 1st November. The guidelines were presented at handover that morning, in addition to widespread display in the EED. Weekly reminders were sent to all involved in phone triaging to encourage the correct use of the guidelines. In any case where the recommended triage outcome was unclear, senior decision-makers could assist. To minimise Hawthorne’s phenomenon, a form of bias whereby the subjects are aware that their actions are being observed, the doctors and nurses staffing the EED were kept unaware that a study was taking place.
Audit cycle + statistical analysis
The audit was repeated in November following the roll-out of the new guidelines. The same methodology was followed. All referrals over the 2-month period were judged by two independent reviewers in comparison to the gold standard guidelines. Referrals for in-person reviews in EED deemed to be unnecessary or from outside the catchment area were noted as ‘unnecessary in-person reviews’. All categorical outcomes were analysed using Pearson’s chi-squared test (χ2). Outcomes with a p-value of < 0.05 were considered statistically significant.
Results
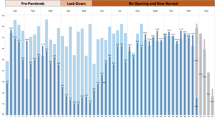
In total, 1700 patients were referred to the eye emergency department over the 2-month period, 861 in October and 839 in November. The mean age profile (53 years old in October vs 52 years old in November) and gender breakdown (50.2% male in October vs 53.3% in November) were similar in both cohorts. Slightly fewer referrals were received from outside of the hospital’s catchment area in November (7.0% in October vs 5.2% in November). The patient demographics can be found in Table 1.
Following the implementation of the guidelines, the number of patients triaged into the EED for in-person review decreased significantly from 692 in October to 577 in November (p < 0.00001). The number of in-person reviews per total patients triaged also decreased significantly, from 0.993 per referral in October to 0.86 in November (p < 0.00001). The new guidelines specifically stated the EED’s catchment areas and patient brought into the department from outside the catchment also decreased from 52 (6%) in October to 32 (3.8%) in November (p = 0.075).
There was a significant increase in the number of patients referred straight to OPD following the creation of clear referral pathways—104 (12.4%) in November, up from just 51 (5.9%) in October (p < 0.00001). Additionally, there was a significant increase in the number of patients who were successfully treated over the phone without requiring an in-person review, 141 (16.8%) in November compared to 104 (12.1%) in October (p = 0.006). There was no significant difference in the numbers referred straight for a minor procedure, 14 (1.6%) in October versus 17 (2.0%) in November (p = 0.54). Ultimately, the number of unnecessary in-person reviews made in bringing patients into the EED unnecessarily as compared to the gold standard guidelines was reduced from 240 (27.9%) in October to 101 (12.0%) in November (p < 0.00001). All outcomes of the audit cycle are found in Table 2.
Discussion/conclusion
Ophthalmology practices have undergone significant change in the COVID-19 pandemic era. It is a particularly high-risk specialty owing to a number of factors including high-volume clinics, close proximity to examine patients, the use of reusable pieces of equipment, and contact with potentially contagious ocular secretions [4, 5]. Slit lamp examination places the ophthalmologist less than 20 cm away from a patient, far from the recommended 1 m social distancing, as such ophthalmologists have suffered high rates of COVID-19 infection [6, 7]. Breazzano et al. found that ophthalmology was one of the specialties with the highest proportion of confirmed COVID-19 cases across all residency programmes in New York [8]. Younger ophthalmologists, who provide the backbone to any EED, were noted to have higher rates of infection [9]. Conjunctivitis, a common presenting symptom to any walk-in EED, is found in approximately 1% of COVID-positive patients and may be the only sign in early disease putting ophthalmologists at further risk [10]. In light of this, we recognised the importance of reducing footfall within the EED during the pandemic. Initially, during the acute phase of the first wave of the pandemic, this was manageable considering the reduced numbers attending healthcare or community optometry settings. However, we aimed to create a model that would be sustainable going forward, during the pandemic and beyond, and improve efficiency and resource allocation within the department. Through the implementation of standardised telemedicine guidelines, we were able to reduce the numbers of in-person EED reviews, from 692 to 577 per month, allowing for more timely assessment of ocular emergencies and more efficient re-direction to OPD where necessary.
Telemedicine, which is the use of digital means to provide healthcare remotely, was first described within ophthalmology in 1999 by HK Li [11]. It sprung to the forefront in March 2020 at the onset of the pandemic as a means to provide ongoing care without risk of disease transmission. This was adopted in the Mater Misericordiae University Hospital’s EED to encompass virtual or phone triaging of referrals. Whilst proving to be effective in the first wave of COVID-19 to triage truly time-sensitive emergencies, over the following year, it became an administrative burden with little reduction of numbers presenting to EED. Upon implementation of our referral guidelines, easily read and widely displayed, we were able to show a reduction in unnecessary or inappropriate presentations to the EED, from 240 in October to 101 in November. As it is an emergency service, it is important that the system does not become overwhelmed and allows for rapid access and treatment of time-sensitive emergencies. Locally agreed protocols allow for better streamlined referrals to clinic and minor operations. The goal of an emergency department should ultimately be to improve outcomes, and in certain conditions which do not require immediate management, more focused follow-up in specialist clinics offer optimal outcomes without unnecessary visits to the EED.
Many presentations to acute eye services are non-urgent and can be effectively and efficiently managed in the community with support from hospital-based ophthalmologists. We were able to successfully manage more patients over the phone, 141 patients in November compared to 104 in October. One study from Moorfields found that 30.6% of patients presenting to their EED were non-acute with a further 37% being considered suitable for review in a community optometrist of GP [12]. More patients managed in the community allow for better allocation of hospital resources, in particular staffing, in a public system with pressing demands.
Moorfields unveiled their ‘Attend Anywhere’ video consultation platform during the initial wave of COVID. In a review of 331 patients assessed, they found that 78.6% did not need in-person eye emergency review [13]. It is important to bear in mind that this was during the acute phase of COVID whereby all but extremely urgent presentations were deferred. Of note, they found that overall patient satisfaction with the service was 4.9 out of 5.0 with a mean consultant time of 12 min and mean wait time of 6 min, down from a mean of 2 h and 8 min for an in-person visit. High patient satisfaction and engagement with telemedicine have been echoed by a number of ophthalmology departments [14,15,16].
Telemedicine is particularly important today as COVID has changed our social habits, even as we emerge into a new phase of the pandemic. There is a cohort of patients who will remain hesitant to return to large waiting areas and over-crowded clinics. Several studies have shown a decrease in patients presenting with urgent ophthalmic conditions such as one Australian study that reported a 16% decrease in EED presentations per day compared to a corresponding period a year prior [17]. These results were even more drastic in Moorfields who reported a 60% decrease in presentations from the 15th March to the 15th April 2020 compared to the year prior. Delays in patients seeking acute ophthalmic care can have major implications on morbidity with one Scottish study finding a decrease in the proportion of retinal detachments that are macula-on at presentation from 44.2% in the pre-COVID period to 34.9% following COVID-19 [18]. Whilst the number attending emergency departments is returning to normal, it is important to be mindful of the cohort of patients who are apprehensive about a return to such environments and in whom delayed presentations must be considered.
On the other hand, there is another generation that have grown accustomed to a virtual form of day to day living. By extension, this may be applied to the delivery of healthcare to provide more efficient and accessible care. The applications are endless and extend beyond acute eye care. A paper by Sommer et al. reviewed 90 papers analysing telemedicine in the COVID-19 era [2]. They discuss the management of acute and chronic conditions through remote care and propose that greater utilisation of community optometry facilities for anterior segment and fundus photos allow greater capacity for hospital ophthalmologists to screen for and monitor disease. This combined with artificial intelligence could be a very powerful tool to improve the workflow of patients being referred to outpatient clinics. At-home ancillary testing, of visual acuity and intra-ocular pressures for example, may also aid virtual triaging in future [19].
Our virtual triaging system for EED consisted of phone calls to patients and/or referrers. Whilst a video format was considered, it relies on heavily on strong internet capability and may prove difficult to use for some elderly patients who require the service. It is also important to realise that video consultation is not a strong examination tool, only offering assessment of some periorbital and anterior segment pathologies. This problem has been circumvented in our department by offering patients or their relatives and guardians the option to email in higher-quality images of such findings for assessment by a triaging ophthalmologist.
The limitations of the study include the potential for bias. Whilst all measures were taken to avoid disclosure of the study, a clear drive to improve referral pathways may have led to some degree of Hawthorne’s phenomenon. Furthermore, this clinical audit involved over 1700 unique referrals, but acknowledging the varied and random nature of presentations to an eye emergency department, a larger study over a longer period may give a more accurate representation of the effectiveness of virtual triaging.
This audit attempted to address the need to reduce footfall during the COVID-19 pandemic. In doing so, we were able to identify suitable avenues of referrals for certain conditions and demonstrate that these guidelines significantly reduced the number of patients presenting to EED with conditions otherwise amenable to phone review or clinic follow-up. The use of telemedicine for triaging has applications beyond the pandemic and we intend to examine the effectiveness of adopting a hybrid model of in-person and virtual management of some chronic ocular conditions in our outpatients clinic.
References
Safadi K, Kruger JM, Chowers I et al (2020) Ophthalmology practice during the COVID-19 pandemic. BMJ Open Ophthalmol 5:e000487. https://doi.org/10.1136/bmjophth-2020-000487
Sommer AC, Blumenthal EZ (2020) Telemedicine in ophthalmology in view of the emerging COVID-19 outbreak. Graefes Arch Clin Exp Ophthalmol 258:2341–2352. https://doi.org/10.1007/s00417-020-04879-2
Gunn PJG, Marks JR, Au L et al (2018) Acceptability and use of glaucoma virtual clinics in the UK: a national survey of clinical leads. BMJ Open Ophthalmol 3:e000127. https://doi.org/10.1136/bmjophth-2017-000127
Danesh-Meyer HV, McGhee CNJ (2021) Implications of COVID-19 for ophthalmologists. Am J Ophthalmol 223:108–118. https://doi.org/10.1016/j.ajo.2020.09.027
Qing H, Li Z, Yang Z et al (2020) The possibility of COVID-19 transmission from eye to nose. Acta Ophthalmol 98:e388. https://doi.org/10.1111/aos.14412
Khatri A, Kharel M, Chaurasiya BD et al (2021) COVID-19 and ophthalmology: an underappreciated occupational hazard. Infect Control Hosp Epidemiol 42:789–790. https://doi.org/10.1017/ice.2020.344
Wan KH, Lin TPH, Ko CN, Lam DSC (2020) Impact of COVID-19 on ophthalmology and future practice of medicine. Asia Pac J Ophthalmol (Phila) 9:279–280. https://doi.org/10.1097/APO.0000000000000305
Breazzano MP, Shen J, Abdelhakim AH et al (2020) New York City COVID-19 resident physician exposure during exponential phase of pandemic. J Clin Invest 130:4726–4733. https://doi.org/10.1172/JCI139587
Esmat SM, Aboulfotouh MR, Ezzelarab MH et al (2021) The role of infection control measures in ophthalmology: do they prevent COVID-19 infection among ophthalmologists in Egypt? A survey-based study. Clin Ophthalmol 15:4347–4355. https://doi.org/10.2147/OPTH.S334252
Wu P, Duan F, Luo C et al (2020) Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol 138:575–578. https://doi.org/10.1001/jamaophthalmol.2020.1291
Li HK (1999) Telemedicine and ophthalmology. Surv Ophthalmol 44:61–72. https://doi.org/10.1016/s0039-6257(99)00059-4
Smith HB, Daniel CS, Verma S et al (2013) Eye casualty services in London Eye (Lond) 27:320–328. https://doi.org/10.1038/eye.2012.297
Kilduff CL, Thomas AA, Dugdill J et al (2020) Creating the Moorfields’ virtual eye casualty: video consultations to provide emergency teleophthalmology care during and beyond the COVID-19 pandemic. BMJ Health Care Inform 27(3). https://doi.org/10.1136/bmjhci-2020-100179
Gerbutavicius R, Brandlhuber U, Gluck S et al (2021) Evaluation of patient satisfaction with an ophthalmology video consultation during the COVID-19 pandemic. Ophthalmologe 118:89–95. https://doi.org/10.1007/s00347-020-01286-0
Roan VD, Sun KJ, Valentim CCS et al (2021) Patient satisfaction in the era of COVID-19: virtual visit vs. in-person visit satisfaction. Optom Vis Sci https://doi.org/10.1097/OPX.0000000000001843
Host BK, Turner AW, Muir J et al (2018) Real-time teleophthalmology video consultation: an analysis of patient satisfaction in rural Western Australia. Clin Exp Optom 101:129–134. https://doi.org/10.1111/cxo.12535
Kam AW, Gunasekaran N, Chaudhry SG et al (2021) Reduction in ophthalmic presentations to australian emergency departments during the COVID-19 period: are we seeing the full picture? Clin Ophthalmol 15:341–346. https://doi.org/10.2147/OPTH.S289467
Shams F, El-Abiary M, Goudie C, Yorston D (2021) Effects of lockdown on retinal detachment incidence in Scotland. Eye (Lond) 35:1279–1280. https://doi.org/10.1038/s41433-020-1029-3
Saleem SM, Pasquale LR, Sidoti PA, Tsai JC (2020) Virtual ophthalmology: telemedicine in a COVID-19 era. Am J Ophthalmol 216:237–242. https://doi.org/10.1016/j.ajo.2020.04.029
Author information
Authors and Affiliations
Contributions
A departmental committee was involved in formulating the initial guidelines at the onset of the pandemic. E.O.N and D.J.H devised the study concept, design, and streamlined guidelines. D.J.H. and S.N. undertook independent data collection from eye emergency department records; D.J.H. wrote the initial draft of the manuscript; E.O.N and S.N. reviewed and made edits to the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hurley, D.J., Neary, S. & O’Neill, E. Virtual triaging in an eye emergency department during the COVID-19 pandemic. Ir J Med Sci 192, 1953–1957 (2023). https://doi.org/10.1007/s11845-022-03160-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03160-1