Abstract
Background
The gingivitis treatment protocols aim to stop the progression of inflammation and prevent the affliction of deeper periodontal tissues. Current research focuses on novel methods that can be applied with handheld and ultrasonic devices to increase the effectiveness of non-surgical periodontal treatment. Ozone has been shown to have a strong antimicrobial effect against bacteria that play a role in the etiology of gingival/periodontal diseases. Research evaluating the effects of ozone gas on the treatment of gingival tissues is limited.
Aim
We investigated the effects of ozone application during the scaling procedure on clinical parameters of gingivitis in smokers and non-smokers and to investigate the efficacy of ozone gas in periodontal treatment.
Methods
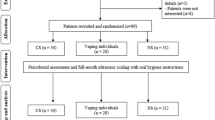
A total of 40 subjects, 27 males/13 females—20 smokers/20 non-smokers—with plaque-induced gingivitis, were selected. The patients underwent a single session of full-mouth supragingival and subgingival scaling. Gaseous ozone application was performed on a randomly selected maxillary quadrant. The other maxillary quadrant was designated as the control group receiving only initial periodontal treatment. Clinical parameters, such as PI, GI, GBTI, and PPD, were measured before and 1 week after treatment.
Results
Our study shows that ozone therapy significantly improves clinical parameters in smokers and non-smokers when applied in addition to periodontal therapy.
Conclusions
Additional studies comparing the effect of ozone therapy on smokers and non-smokers to the effects of oral mouthwashes may provide valuable contributions to the field.




Similar content being viewed by others
References
Kinane DF (1999) Periodontitis modified by systemic factors. Ann Periodontol 4(1):54–64. https://doi.org/10.1902/annals.1999.4.1.54
Lang NP, Bartold PM (2018) Periodontal health. J Clin Periodontol 45(S20):9–16. https://doi.org/10.1111/jcpe.12936
Mariotti A (1999) Dental plaque-induced gingival diseases. Ann Periodontol 4(1):7–19. https://doi.org/10.1902/annals.1999.4.1.7
Kinane DF, Attström R (2005) Advances in the pathogenesis of periodontitiss. Group B consensus report of the fifth European workshop in periodontology. J Clin Periodontol 32(6):130–131. https://doi.org/10.1111/j.1600-051x.2005.00823.x
Dye BA (2012) Global periodontal disease epidemiology. Periodontol 58(1):10–25. https://doi.org/10.1111/j.1600-0757.2011.00413.x
White DA, Tsakos G, Pitts NB, Fuller E, Douglas GVA, Murray JJ, Steele JG (2012) Adult dental health survey 2009: common oral health conditions and their impact on the population. Br Dent J 213(11):567–572. https://doi.org/10.1038/sj.bdj.2012.1088
Silva AMM, Newman HN, Oakley DA, O'Leary R (1998) Psychosocial factors, dental plaque levels and smoking in periodontitis patients. J Clin Periodontol 25(6):517–523
Ryder MI (2007) The influence of smoking on host responses in periodontal infections. Periodontol 2000(43):266–277. https://doi.org/10.1111/j.1600-0757.2006.00163.x
Nociti FH Jr, Casati MZ, Duarte PM (2015) Current perspective of the impact of smoking on the progression and treatment of periodontitis. Periodontol 67(1):187–210. https://doi.org/10.1111/prd.12063
Tunkel J, Heinecke A, Flemmig TF (2002) A systematic review of efficacy of machine-driven and manual subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol 29(S3):72–81. https://doi.org/10.1034/j.1600-051X.29.s3.4.x
Azarpazhooh A, Limeback H (2008) The application of ozone in dentistry: a systematic review of literature. J Dent 36(2):104–116. https://doi.org/10.1016/j.jdent.2007.11.008
Gupta G, Mansi B (2012) Ozone therapy in periodontics. J Med Life 5(1):59–67
Nagayoshi M, Fukuizumi T, Kitamura C, Yano J, Terashita M, Nishihara T (2004) Efficacy of ozone on survival and permeability of oral microorganisms. Oral Microbiol Immunol 19(4):240–246. https://doi.org/10.1111/j.1399-302X.2004.00146.x
Sunnen GV (1988) Ozone in medicine: overview and future directions. J Adv Med 1(3):159–174
Bocci V (1999) Biological and clinical effects of ozone. Has ozone therapy a future in medicine? Br J Biomed Sci 56(4):270–279
Seidler V, Linetskiy I, Hubálková H, Stanková H, Smucler R, Mazánek J (2008) Ozone and its usage in general medicine and dentistry. A review article. Prague Med Rep 109(1):5–13
Çalışır M, Talmac AC, Ege B, Poyraz Ö, Dumlupınar E (2019) The effect of ozone gas on IL-1β and IL-10 levels of gingival crevicular fluid in aggressive periodontitis patients. Ozone Sci Eng 41(6):571–578. https://doi.org/10.1080/01919512.2019.1575183
Uraz A, Karaduman B, Isler SÇ, Gönen S, Çetiner D (2019) Ozone application as adjunctive therapy in chronic periodontitis: clinical, microbiological and biochemical aspects. J Dent Sci 14(1):27–37. https://doi.org/10.1016/j.jds.2018.06.005
Silness J, Löe H (1964) Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135. https://doi.org/10.3109/00016356408993968
Löe H, Silness J (1963) Periodontal disease in pregnancy I. Prevalence and severity. Acta Odontol Scand 21:533–551. https://doi.org/10.3109/00016356309011240
Nowicki D, Vogel RI, Melcer S, Deasy MJ (1981) The gingival bleeding time index. J Periodontol 52(5):260–262. https://doi.org/10.1902/jop.1981.52.5.260
Van Der Weijden GA, Timmerman MF (2002) A systematic review on the clinical efficacy of subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol 29(S3):55–71. https://doi.org/10.1034/j.1600-051X.29.s3.3.x
Heitz-Mayfield LJ, Trombelli L, Heitz F et al (2002) A systematic review of the effect of surgical debridement vs. non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol 29(3):92–102. https://doi.org/10.1034/j.1600-051x.29.s3.5.x
Cline NV, Layman DL (1992) The effects of chlorhexidine on the attachment and growth of cultured human periodontal cells. J Periodontol 63(7):598–602. https://doi.org/10.1902/jop.1992.63.7.598
Mandel ID (1988) Chemotherapeutic agents for controlling plaque and gingivitis. J Clin Periodontol 15(8):488–498. https://doi.org/10.1111/j.1600-051X.1988.tb01020.x
Adamietz IA, Rahn R, Böttcher HD, Schäfer V, Reimer K, Fleischer W (1998) Prophylaxis with povidone-iodine against induction of oral mucositis by radiochemotherapy. Support Care Cancer 6(4):373–377. https://doi.org/10.1007/s005200050179
Dona BL, Gründemann LJ, Steinfort J et al (1998) The inhibitory effect of combining chlorhexidine and hydrogen peroxide on 3-day plaque accumulation. J Clin Periodontol 25(11):879–883. https://doi.org/10.1111/j.1600-051x.1998.tb02385.x
Arweiler NB, Netuschil L, Reich E (2001) Alcohol-free mouthrinse solutions to reduce supragingival plaque regrowth and vitality: a controlled clinical study. J Clin Periodontol 28(2):168–174. https://doi.org/10.1034/j.1600-051x.2001.028002168.x
Epstein JB, Jr Silverman S, Paggiarino DA et al (2001) Benzydamine HCl for prophylaxis of radiation-induced oral mucositis: results from a multicenter, randomized, double-blind, placebo-controlled clinical trial. Cancer 92(4):875–885. https://doi.org/10.1002/1097-0142(20010815)92:4<875::AID-CNCR1396>3.0.CO;2-1
Hasturk H, Nunn M, Warbington M, Dyke TEV (2004) Efficacy of a fluoridated hydrogen peroxide-based mouthrinse for the treatment of gingivitis: a randomized clinical trial. J Periodontol 75(1):57–65. https://doi.org/10.1902/jop.2004.75.1.57
Fine DH, Furgang D, Sinatra K, Charles C, McGuire A, Kumar LD (2005) In vivo antimicrobial effectiveness of an essential oil-containing mouth rinse 12 h after a single use and 14 days’ use. J Clin Periodontol 32(4):335–340. https://doi.org/10.1111/j.1600-051x.2005.00674.x
Witt J, Ramji N, Gibb R, Dunavent J, Flood J, Barnes J (2005) Antibacterial and antiplaque effects of a novel, alcohol-free oral rinse with cetylpyridinium chloride. J Contemp Dent Pract 6(1):1–9. https://doi.org/10.5005/jcdp-6-1-1
McCullough MJ, Farah CS (2008) The role of alcohol in oral carcinogenesis with particular reference to alcohol-containing mouthwashes. Aust Dent J 53(4):302–305. https://doi.org/10.1111/j.1834-7819.2008.00070.x
Jones CG (1997) Chlorhexidine: is it still the gold standard? Periodontol 2000(15):55–62. https://doi.org/10.1111/j.1600-0757.1997.tb00105.x
Gagari E, Kabani S (1995) Adverse effects of mouthwash use. A review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 80(4):432–439. https://doi.org/10.1016/S1079-2104(05)80337-3
Boyle P, Koechlin A, Autier P (2014) Mouthwash use and the prevention of plaque, gingivitis and caries. Oral Dis 20(S1):1–68. https://doi.org/10.1111/odi.12187
Dhingra K, Vandana KL (2011) Management of gingival inflammation in orthodontic patients with ozonated water irrigation–a pilot study. Int J Dent Hygiene 9(4):296–302. https://doi.org/10.1111/j.1601-5037.2011.00506.x
Hayakumo S, Arakawa S, Mano Y, Izumi Y (2013) Clinical and microbiological effects of ozone nano-bubble water irrigation as an adjunct to mechanical subgingival debridement in periodontitis patients in a randomized controlled trial. Clin Oral Investig 17(2):379–388. https://doi.org/10.1007/s00784-012-0711-7
Skurska A, Pietruska MD, Paniczko-Drȩzek A et al (2010) Evaluation of the influence of ozonotherapy on the clinical parameters and MMP levels in patients with chronic and aggressive periodontitis. Adv Med Sci 55(2):297–307. https://doi.org/10.2478/v10039-010-0048-x
Montevecchi M, Dorigo A, Cricca M, Checchi L (2013) Comparison of the antibacterial activity of an ozonated oil with chlorhexidine digluconate and povidone-iodine. A disk diffusion test. New Microbiol 36(3):289–302
Huth KC, Saugel B, Jakob FM, Cappello C, Quirling M, Paschos E, Ern K, Hickel R, Brand K (2007) Effect of aqueous ozone on the NF-KB system. J Dent Res 86(5):451–456. https://doi.org/10.1177/154405910708600512
Kshitish D, Laxman VK (2010) The use of ozonated water and 0.2% chlorhexidine in the treatment of periodontitis patients: a clinical and microbiologic study. Indian J Dent Res 21(3):341–348. https://doi.org/10.4103/0970-9290.70796
Patel PV, Patel A, Kumar S, Holmes JC (2012) Effect of subgingival application of topical ozonated olive oil in the treatment of chronic periodontitis: a randomized, controlled, double blind, clinical and microbiological study. Minerva Stomatol 61(9):381–398
Indurkar MS, Verma R (2016) Effect of ozonated oil and chlorhexidine gel on plaque induced gingivitis: a randomized control clinical trial. J Indian Soc Periodontol 20(1):32–35. https://doi.org/10.4103/0972-124X.170806
Ebensberger U, Pohl Y, Filippi A (2002) PCNA-expression of cementoblasts and fibroblasts on the root surface after extraoral rinsing for decontamination. Dent Traumatol 18(5):262–265. https://doi.org/10.1034/j.1600-9657.2002.00087.x
Ramzy MI, Gomaa HE, Mostafa MI et al (2005) Management of aggressive periodontitis using ozonized water. Egypt Med J NRCenter 6(1):229–245
Huth KC, Quirling M, Lenzke S, Paschos E, Kamereck K, Brand K, Hickel R, Ilie N (2011) Effectiveness of ozone against periodontal pathogenic microorganisms. Eur J Oral Sci 119(3):204–210. https://doi.org/10.1111/j.1600-0722.2011.00825.x
Dodwad V, Gupta S, Kumar K et al (2011) Changing paradigm in pocket therapy - ozone vs conventional irrigation. Int J Public Health Dent 2(2):7–12
Mallampalli A, Guntupalli KK (2004) Smoking and systemic disease. Med Clin North Am 88(6):1431–1451. https://doi.org/10.1016/j.mcna.2004.07.001
Winn DM (2001) Tobacco use and oral disease. J Dent Educ 65(4):306–312
Johnson GK, Guthmiller JM (2007) The impact of cigarette smoking on periodontal disease and treatment. Periodontol 2000(44):178–194. https://doi.org/10.1111/j.1600-0757.2007.00212.x
Tomar SL, Asma S (2000) Smoking-attributable periodontitis in the United States: findings from NHANES III. National Health and Nutrition Examination Survey. J Periodontol 71(5):743–751. https://doi.org/10.1902/jop.2000.71.5.743
Hyman JJ, Reid BC (2003) Epidemiologic risk factors for periodontal attachment loss among adults in the United States. J Clin Periodontol 30(3):230–237. https://doi.org/10.1034/j.1600-051X.2003.00157.x
Bergström J (2004) Tobacco smoking and chronic destructive periodontal disease. Odontology 92(1):1–8. https://doi.org/10.1007/s10266-004-0043-4
Torrungruang K, Nisapakultorn K, Sutdhibhisal S, Tamsailom S, Rojanasomsith K, Vanichjakvong O, Prapakamol S, Premsirinirund T, Pusiri T, Jaratkulangkoon O, Kusump S, Rajatanavin R (2005) The effect of cigarette smoking on the severity of periodontal disease among older Thai adults. J Periodontol 76(4):566–572. https://doi.org/10.1902/jop.2005.76.4.566
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol of this randomized, controlled, and double-blind study was approved by the Adıyaman University Biomedical Research Ethics Committee with approval number 2016/5-9. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Talmaç, A.C., Çalişir, M. Efficacy of gaseous ozone in smoking and non-smoking gingivitis patients. Ir J Med Sci 190, 325–333 (2021). https://doi.org/10.1007/s11845-020-02271-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02271-x