Abstract
Background
Liver fibrosis is the primary cause of liver cirrhosis and hepatocellular carcinoma and leads to considerable morbidity and mortality. Recent studies have shown that microRNAs are associated with fibrotic processes in liver disorders, but the exact role of miR-202 is still unclear, and its related mechanisms are not fully understood.
Aims
The aim of this research is to analyze the regarded regulation of miR-202 on HGF and its role in the pathological progress of liver fibrosis.
Methods
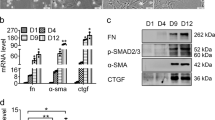
In the present study, qRT-PCR was used to detect the expression level of miR-202 in serum of patients with liver fibrosis and to compare its expression in patients with different pathological stages. HGF was predicted to be the target gene of miR-202 by TargetScan and was verified by Dual-luciferase reporter gene assay. qRT-PCR and western blot were used to detect the regulatory effect of mir-202 on the mRNA and protein of HGF; effect of miR-202 on the expression of fibrosis factors α-smooth muscle actin (α-SMA), FSP1, and collagen was detected; effect of miR-202 on liver fibrosis in mice was detected by establishing CCL4-induced mouse model.
Results
We found that the expression level of miR-202 in serum of patients with liver fibrosis was significantly higher than that of healthy people, and increased with the increase of fibrosis; miR-202 inhibited the expression level of mRNA and protein of HGF by combining with the 3’-UTR of HGF; the expression level of miR-202 significantly increased after hepatic stellate cells (HSC) were stimulated by AngII; the overexpression of miR-202 could up-regulate the expression of fibrotic factors α-SMA, FSP1, and collagen I. In addition, miR-202 up-regulated the expression of collagen I and collagen III in liver tissue of mice with liver fibrosis and promoted the progress of liver fibrosis.
Conclusions
miR-202 could negatively regulate the expression of target gene HGF, activated HSC, and increased the expression levels of various fibrosis factors, and the pathological process of liver fibrosis injury was promoted.





Similar content being viewed by others
References
Yang XZ, Gen AW, Xian JC, Xiao L (2018) Diagnostic value of various noninvasive indexes in the diagnosis of chronic hepatic fibrosis. Eur Rev Med Pharmacol Sci 22(2):479–485
Bilezikçi B, Haberal AN, Demirhan B (2016) Hepatocyte growth factor in patients with three different stages of chronic liver disease including hepatocellular carcinoma, cirrhosis and chronic hepatitis: an immunohistochemical study. 15(3):159
Ge L, Shi B, Song YE, Li Y, Wang S, Wang X (2015) Clinical value of real-time elastography quantitative parameters in evaluating the stage of liver fibrosis and cirrhosis. Exp Ther Med 10(3):983–990
Xinguang Y, Huixing Y, Linlin W, Wanxin W, Xiaojun W, Linghua Y (2016) RSPOs facilitated HSC activation and promoted hepatic fibrogenesis. Oncotarget. 7(39):63767–63778
Wu K, Ye C, Lin L et al (2016) Inhibiting miR-21 attenuates experimental hepatic fibrosis by suppressing both the ERK1 pathway in HSC and hepatocyte EMT. Clin Sci (Lond) 130(16):1469–1480
Tjomsland V, Aasrum M, Christoffersen T, Gladhaug IP (2017) Functional heterogeneity in tumor-derived human pancreatic stellate cells: differential expression of HGF and implications for mitogenic signaling and migration in pancreatic cancer cells. Oncotarget. 8(42):71672–71684
Hultberg A, Morello V, Huyghe L, de Jonge N, Blanchetot C, Hanssens V, de Boeck G, Silence K, Festjens E, Heukers R, Roux B, Lamballe F, Ginestier C, Charafe-Jauffret E, Maina F, Brouckaert P, Saunders M, Thibault A, Dreier T, de Haard H, Michieli P (2015) Depleting MET-expressing tumor cells by ADCC provides a therapeutic advantage over inhibiting HGF/MET signaling. Cancer Res 75(16):3373–3383
Fioroni I, Dell'Aquila E, Pantano F, Intagliata S, Caricato M, Vincenzi B, Coppola R, Santini D, Tonini G (2015) Role of c-mesenchymal-epithelial transition pathway in gastric cancer. Expert Opin Pharmacother 16(8):1195–1207
Pothula SP, Xu Z, Goldstein D, Biankin AV, Pirola RC, Wilson JS, Apte MV (2016) Hepatocyte growth factor inhibition: a novel therapeutic approach in pancreatic cancer. Br J Cancer 114(3):269–280
Eulalio A, Huntzinger E, Izaurralde E (2008) Getting to the root of miRNA-mediated gene silencing. Cell. 132(1):9–14
Bruhn O, Drerup K, Kaehler M, Haenisch S, RöDer C, Cascorbi I (2016) Length variants of the ABCB1 3'-UTR and loss of miRNA binding sites: possible consequences in regulation and pharmacotherapy resistance. Pharmacogenomics. 17(4):327–340
Sun M, Ding J, Li D, Yang G, Cheng Z, Zhu Q (2017) NUDT21 regulates 3'-UTR length and microRNA-mediated gene silencing in hepatocellular carcinoma. Cancer Lett 410:158
Zhou L, Liu S, Han M et al (2018) miR-185 inhibits fibrogenic activation of hepatic stellate cells and prevents liver fibrosis. Mol Ther Nucleic Acids 10(C):91–102
Lu L, Wang J, Lu H, Zhang G, Liu Y, Wang J, Zhang Y, Shang H, Ji H, Chen X, Duan Y, Li Y (2015) MicroRNA-130a and -130b enhance activation of hepatic stellate cells by suppressing PPARγ expression: a rat fibrosis model study. Biochem Biophys Res Commun 465(3):387–393
Liss KH, Finck BN (2017) PPARs and nonalcoholic fatty liver disease. Biochimie. 136:65–74
Ishak K, Baptista A, Bianchi L et al (1995) Histological grading and staging of hepatitis. J Hepatol 22(7):696
Wang CH, Wey KC, Mo LR, Chang KK, Lin RC, Kuo JJ (2015) Current trends and recent advances in diagnosis, therapy, and prevention of hepatocellular carcinoma. Asian Pac J Cancer Prev 16(9):3595–3604
Ahmed A, Wong RJ, Harrison SA (2015) Nonalcoholic fatty liver disease review: diagnosis, treatment, and outcomes. Clin Gastroenterol Hepatol 13(12):2062–2070
Younossi Z, Henry L (2016) Contribution of alcoholic and nonalcoholic fatty liver disease to the burden of liver-related morbidity and mortality. Gastroenterology. 150(8):1778–1785
Guo L, Zhao Y, Yang S, Zhang H, Chen F (2014) An integrated analysis of miRNA, lncRNA, and mRNA expression profiles. Biomed Res Int 2014:345605
Angrand PO, Vennin C, Bourhis XL, Adriaenssens E (2015) The role of long non-coding RNAs in genome formatting and expression. Front Genet 6:165
Barman B, Bhattacharyya SN (2015) mRNA targeting to endoplasmic reticulum precedes ago protein interaction and MicroRNA (miRNA)-mediated translation repression in mammalian cells. J Biol Chem 290(41):24650–24656
Yu F, Jiang Z, Chen B, Dong P, Zheng J (2017) NEAT1 accelerates the progression of liver fibrosis via regulation of microRNA-122 and Kruppel-like factor 6. J Mol Med 95(11):1–12
Yu F, Lu Z, Huang K, Wang X, Xu Z, Chen B, Dong P, Zheng J (2016) MicroRNA-17-5p-activated Wnt/β-catenin pathway contributes to the progression of liver fibrosis. Oncotarget. 7(1):81–93
Crocco P, Montesanto A, Passarino G, Rose G (2016) Polymorphisms falling within putative miRNA target sites in the 3'UTR region of SIRT2 and DRD2 genes are correlated with human longevity. J Gerontol A Biol Sci Med Sci 71(5):586–592
Rao R, Nagarkatti P, Nagarkatti M (2015) Role of miRNA in the regulation of inflammatory genes in staphylococcal enterotoxin B-induced acute inflammatory lung injury and mortality. Toxicol Sci 144(2):284–297
Ergun S, Oztuzcu S (2014) Computational analysis of 3'UTR region of CASP3 with respect to miRSNPs and SNPs in targetting miRNAs. Comput Biol Chem 53PB:235–241
Knox B, Wang Y, Rogers LJ, Xuan J, Yu D, Guan H, Chen J, Shi T, Ning B, Kadlubar SA (2018) A functional SNP in the 3'-UTR of TAP2 gene interacts with microRNA hsa-miR-1270 to suppress the gene expression. Environ Mol Mutagen 59(2):134–143
Papageorgiou I, Court MH (2017) Identification and validation of the microRNA response elements in the 3'-untranslated region of the UDP glucuronosyltransferase (UGT) 2B7 and 2B15 genes by a functional genomics approach. Biochem Pharmacol 146:199–213
Carrara D, Bernini M, Bacca A, Rugani I, Duranti E, Virdis A, Ghiadoni L, Taddei S, Bernini G (2014) Cholecalciferol administration blunts the systemic renin-angiotensin system in essential hypertensives with hypovitaminosis D. J Renin-Angiotensin-Aldosterone Syst 15(1):82–87
Roderburg C, Urban GW, Bettermann K, Vucur M, Zimmermann H, Schmidt S, Janssen J, Koppe C, Knolle P, Castoldi M, Tacke F, Trautwein C, Luedde T (2011) Micro-RNA profiling reveals a role for miR-29 in human and murine liver fibrosis. Hepatology. 53(1):209–218
Baroni GS, D'Ambrosio L, Curto P et al (2010) Interferon gamma decreases hepatic stellate cell activation and extracellular matrix deposition in rat liver fibrosis. Hepatology. 23(5):1189–1199
Abergel A, Sapin V, Dif N, Chassard C, Darcha C, Marcand-Sauvant J, Gaillard-Martinie B, Rock E, Dechelotte P, Sauvant P (2006) Growth arrest and decrease of alpha-SMA and type I collagen expression by palmitic acid in the rat hepatic stellate cell line PAV-1. Dig Dis Sci 51(5):986–995
Zhang DS, Li YY, Chen XJ, Li YJ, Liu ZY, Xie WJ, Sun ZL (2015) BCL2 promotor methylation and miR-15a/16-1 upregulation is associated with sanguinarine-induced apoptotic death in rat HSC-T6 cells. J Pharmacol Sci 127(1):135–144
Kariya A, Furusawa Y, Yunoki T, Kondo T, Tabuchi Y (2014) A microRNA-27a mimic sensitizes human oral squamous cell carcinoma HSC-4 cells to hyperthermia through downregulation of Hsp110 and Hsp90. Int J Mol Med 34(1):334–340
Venugopal SK, Jiang J, Kim TH et al (2010) Liver fibrosis causes downregulation of miRNA-150 and miRNA-194 in hepatic stellate cells, and their overexpression causes decreased stellate cell activation. Am J Physiol Gastrointest Liver Physiol 298(1):101–106
Ogawa T, Enomoto M, Fujii H, Sekiya Y, Yoshizato K, Ikeda K, Kawada N (2012) MicroRNA-221/222 upregulation indicates the activation of stellate cells and the progression of liver fibrosis. Gut. 61(11):1600–1609
Kagami S (2012) Involvement of glomerular renin-angiotensin system (RAS) activation in the development and progression of glomerular injury. Clin Exp Nephrol 16(2):214–220
Arteel GE (2004) "HOPE" for the liver? Mechanistic insight into the role of the renin-angiotensin system in hepatic fibrosis. Hepatology. 40(1):263–265
Finot F, Masson R, Desmots F et al (2012) Combined stimulation with the tumor necrosis factor α and the epidermal growth factor promotes the proliferation of hepatocytes in rat liver cultured slices. Int J Hepatol 2012:785786
Kong LM, Liao CG, Fei F, Guo X, Xing JL, Chen ZN (2010) Transcription factor Sp1 regulates expression of cancer-associated molecule CD147 in human lung cancer. Cancer Sci 101(6):1463–1470
Cram EJ, Liu BD, Bjeldanes LF, Firestone GL (2001) Indole-3-carbinol inhibits CDK6 expression in human MCF-7 breast cancer cells by disrupting Sp1 transcription factor interactions with a composite element in the CDK6 gene promoter. J Biol Chem 276(25):22332–22340
Lemberger UJ, Penz-Österreicher M, Brenner D, Trauner M, Österreicher CH (2014) P167 lack of FSP1/S100A4 attenuates liver fibrosis in mice. J Hepatol 60(1):S122–S122
Yokoyama K, Kimoto K, Itoh Y, Nakatsuka K, Matsuo N, Yoshioka H, Kubota T (2012) The PI3K/Akt pathway mediates the expression of type I collagen induced by TGF-β2 in human retinal pigment epithelial cells. Graefes Arch Clin Exp Ophthalmol 250(1):15–23
Wang BB, Cheng JY, Gao HH, Zhang Y, Chen ZN, Bian H (2010) Hepatic stellate cells in inflammation-fibrosis-carcinoma axis. Anat Rec (Hoboken) 293(9):1492–1496
Funding
This work was supported by AIDS and viral hepatitis and other major infectious disease prevention and control, National Science and technology major projects, and sub topics new target research on anti HBV treatment (2012ZX10002006-003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Niu, X., Nong, S., Gong, J. et al. Research on promoting liver fibrosis injury by the targeted regulation of miR-202 for HGF to activate HSC. Ir J Med Sci 189, 1295–1304 (2020). https://doi.org/10.1007/s11845-020-02210-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02210-w