Abstract
Abstract
Depression is a common disorder in patients with implantable cardioverter defibrillator (ICD). There are a variety of studies estimated the prevalence of depression in these patients. The present study aimed to investigate the prevalence of depression in patients with ICD.
Methods
In the present study, we conducted a systematic review of studies published in PubMed, Scopus, Web of Science (WoS), Medline, and EMBASE without any time filtration to obtain studies investigated the prevalence of depression in patients with ICD. Search terms consisted of “Implantable Cardioverter Defibrillator(s)” in combination with “depression,” “depressive,” “prevalence,” “implanted cardioverter,” “implantable,” and “implantable defibrillator.”
Results
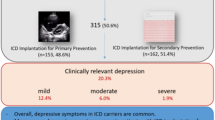
We identified 15 relevant studies, comprising data from 10,182 patients with ICD from whom 2400 (23.58%) (95% CI, 15.36–31.79) had depression. The results of the subgroup analysis showed that the prevalence of depression among middle-aged patients (28.58% with confidence interval of 95%, 21.51–35.65) was higher than elderly patients (22.23% with confidence interval of 95%, 11.21–33.24) and it was not significantly correlated with the mean age of samples (P = 0.255), sample size (P = 0.686), and the publication date (P = 0.784), although there was a significant correlation between the prevalence of depression and the quality of articles so that the prevalence was decreasing with an increase in the quality (P = 0.046).
Conclusion
Around 1 in 4 patients with ICD (23.58%) experiences depression progression after an ICD placement. This prevalence is comparable to that in the general population, and close to that of the patients with common chronic diseases.




Similar content being viewed by others
References
Mirbagher Ajorpaz N, Kafaei Atrian M (2014) The effect of self-care education on quality of life in unstable angina patients in Kashan Shahid Behashti Hospital, 2011. J Res Dev Nurs Midwifery 11(1):1–7
Mc Namara K, Alzubaidi H, Jackson JK (2019) Cardiovascular disease as a leading cause of death: how are pharmacists getting involved? Integr Pharm Res Pract 2019(8):1–11
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R (2018) Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation 137(12):e67–e492
Karunathilake SP, Ganegoda GU (2018, 2018) Secondary prevention of cardiovascular diseases and application of technology for early diagnosis. Biomed Res Int
Rakhshan M, Hassani P, Ashktorab T (2013) Lived experiences of cardiac pacemaker patients. J Qual Res Health Sci 2(1):33–45
Akel T, Lafferty J (2017) Implantable cardioverter defibrillators for primary prevention in patients with nonischemic cardiomyopathy: a systematic review and meta-analysis. Cardiovasc Ther 35(3):1–8
Ghavami Ghanbarabadi V, Jamali J, Heidari-Bakavoli A, Tayyebi M, Nazari Hyanlo H, Shakeri MT (2013) Factors influencing the status of appropriate and inappropriate shocks delivered by an implantable cardioverter defibrillator. J Birjand Univ Med Sci 20(1):94–101
Oshvandi K, Keshmiri K, Salavati M, Emkanjoo Z, Musavi S (2013) Effectiveness of education based on Orem’s self-care model in self-care activity of patients with implantable cardioverter defibrillators. J Hayat 19(3):47–55
Magyar-Russell G, Thombs BD, Cai JX, Baveja T, Kuhl EA, Singh PP, Barroso MMB, Arthurs E, Roseman M, Amin N (2011) The prevalence of anxiety and depression in adults with implantable cardioverter defibrillators: a systematic review. J Psychosom Res 71(4):223–231
Marcus FI, Zareba W, Calkins H, Towbin JA, Basso C, Bluemke DA, Estes NM, Picard MH, Sanborn D, Thiene G (2009) Arrhythmogenic right ventricular cardiomyopathy/dysplasia clinical presentation and diagnostic evaluation: results from the North American Multidisciplinary Study. Heart Rhythm 6(7):984–992
Frydensberg VS, Skovbakke SJ, Pedersen SS, Kok RN (2018) Body image concerns in patients with an implantable cardioverter defibrillator: a scoping review. Pacing Clin Electrophysiol 41(9):1235–1260
Tomzik J, Koltermann KC, Zabel M, Willich SN, Reinhold T (2015) Quality of life in patients with an implantable cardioverter defibrillator: a systematic review. Front Cardiovasc Med 2(34):1–11
Peregrinova L, Jordan J (2017) Psychotherapy for posttraumatic stress disorders among cardiac patients after implantable cardioverter defibrillator shocks. Feasibility and implementation of a psychocardiological therapy manual in inpatient cardiac rehabilitation. Heart Mind 1(1):42–55
McCrae CS, Roth AJ, Ford J, Crew EC, Conti JB, Berry RB, Sears SF (2016) Sleep, psychosocial functioning, and device-specific adjustment in patients with implantable cardioverter defibrillators (ICDs). Behav Sleep Med 14(1):49–66
Amiaz R, Asher E, Rozen G, Czerniak E, Glikson M, Weiser M (2016) Do implantable cardioverter defibrillators contribute to new depression or anxiety symptoms? A retrospective study. Int J Psychiatry Clin Pract 20(2):101–105
Habibović M, Denollet J, Pedersen SS, investigators W (2017) Posttraumatic stress and anxiety in patients with an implantable cardioverter defibrillator: trajectories and vulnerability factors. Pacing Clin Electrophysiol 40(7):817–823
Tzeis S, Kolb C, Baumert J, Reents T, Zrenner B, Deisenhofer I, Ronel J, Andrikopoulos G, LADWIG KH (2011) Effect of depression on mortality in implantable cardioverter defibrillator recipients—findings from the prospective LICAD study. Pacing Clin Electrophysiol 34(8):991–997
Ingles J, Sarina T, Kasparian N, Semsarian C (2013) Psychological wellbeing and posttraumatic stress associated with implantable cardioverter defibrillator therapy in young adults with genetic heart disease. Int J Cardiol 168(4):3779–3784. https://doi.org/10.1016/j.ijcard.2013.06.006
Mastenbroek MH, Versteeg H, Jordaens L, Theuns DA, Pedersen SS (2016) Ventricular tachyarrhythmias and mortality in implantable cardioverter defibrillator patients: impact of depression in the MIDAS cohort. How to improve implantable cardioverter defibrillator therapy. 76:85
Wong MF (2017) Factors associated with anxiety and depression among patients with implantable cardioverter defibrillator. J Clin Nurs 26(9–10):1328–1337. https://doi.org/10.1111/jocn.13637
Gostoli S, Bonomo M, Roncuzzi R, Biffi M, Boriani G, Rafanelli C (2016) Psychological correlates, allostatic overload and clinical course in patients with implantable cardioverter defibrillator (ICD). Int J Cardiol 220:360–364
Atwater BD, Daubert JP (2012) Implantable cardioverter defibrillators: risks accompany the life-saving benefits. Heart 98(10):764–772
Kamphuis HC, de Leeuw JR, Derksen R, Hauer RN, Winnubst JA (2003) Implantable cardioverter defibrillator recipients: quality of life in recipients with and without ICD shock delivery: a prospective study. Europace 5(4):381–389. https://doi.org/10.1016/s1099-5129(03)00078-3
Sebdani AM, Alamdary MP, Abdollahpour N (2017) Depression among patients undergoing hemodialysis; a narrative review. J Prev Epidemiol 3(1)
Harder T (2014) Some notes on critical appraisal of prevalence studies: comment on: “The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence”. Int J Health Policy Manag 3(5):289–290
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T (2013) Meta-analysis of prevalence. J Epidemiol Community Health 67(11):974–978
Farrugia MK, Kirsch AJ (2017) Application of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement to publications on endoscopic treatment for vesicoureteral reflux. J Pediatr Urol 13(3):320–325. https://doi.org/10.1016/j.jpurol.2017.02.005
Ades AE, Lu G, Higgins JP (2005) The interpretation of random-effects meta-analysis in decision models. Med Decis Making 25(6):646–654. https://doi.org/10.1177/0272989x05282643
Pedersen SS, Andersen CM, Denollet J, Habibovic M (2018) Depressive symptoms in patients with an implantable cardioverter defibrillator: does treatment expectations play a role? Gen Hosp Psychiatry 51:10–14. https://doi.org/10.1016/j.genhosppsych.2017.12.002
Thylen I, Dekker RL, Jaarsma T, Stromberg A, Moser DK (2014) Characteristics associated with anxiety, depressive symptoms, and quality-of-life in a large cohort of implantable cardioverter defibrillator recipients. J Psychosom Res 77(2):122–127. https://doi.org/10.1016/j.jpsychores.2014.05.007
Shalaby AA, Brumberg GE, Pointer L, Bekelman DB, Rumsfeld JS, Yang Y, Pellegrini CN, Heidenreich PA, Keung E, Massie BM, Varosy PD (2014) Depression and outcome among veterans with implantable cardioverter defibrillators with or without cardiac resynchronization therapy capability. Pacing Clin Electrophysiol 37(8):994–1001. https://doi.org/10.1111/pace.12361
Mastenbroek MH, Versteeg H, Jordaens L, Theuns DA, Pedersen SS (2014) Ventricular tachyarrhythmias and mortality in patients with an implantable cardioverter defibrillator: impact of depression in the MIDAS cohort. Psychosom Med 76(1):58–65
Pedersen SS, Hoogwegt MT, Jordaens L, Theuns DA (2011) Relation of symptomatic heart failure and psychological status to persistent depression in patients with implantable cardioverter-defibrillator. Am J Cardiol 108(1):69–74. https://doi.org/10.1016/j.amjcard.2011.02.344
Suzuki T, Shiga T, Kuwahara K, Kobayashi S, Suzuki S, Nishimura K, Suzuki A, Ejima K, Manaka T, Shoda M, Ishigooka J, Kasanuki H, Hagiwara N (2010) Prevalence and persistence of depression in patients with implantable cardioverter defibrillator: a 2-year longitudinal study. Pacing Clin Electrophysiol 33(12):1455–1461. https://doi.org/10.1111/j.1540-8159.2010.02887.x
Luyster FS, Hughes JW, Gunstad J (2009) Depression and anxiety symptoms are associated with reduced dietary adherence in heart failure patients treated with an implantable cardioverter defibrillator. J Cardiovasc Nurs 24(1):10–17. https://doi.org/10.1097/01.Jcn.0000317469.63886.24
Johansen JB, Pedersen SS, Spindler H, Andersen K, Nielsen JC, Mortensen PT (2008) Symptomatic heart failure is the most important clinical correlate of impaired quality of life, anxiety, and depression in implantable cardioverter-defibrillator patients: a single-centre, cross-sectional study in 610 patients. Europace 10(5):545–551. https://doi.org/10.1093/europace/eun073
Undavia M, Goldstein NE, Cohen P, Sinthawanarong K, Singson M, Bhutani D, Munson T, Gomes JA, Fischer A, Mehta D (2008) Impact of implantable cardioverter-defibrillator recalls on patients' anxiety, depression, and quality of life. Pacing Clin Electrophysiol 31(11):1411–1418. https://doi.org/10.1111/j.1540-8159.2008.01204.x
Bilge AK, Ozben B, Demircan S, Cinar M, Yilmaz E, Adalet K (2006) Depression and anxiety status of patients with implantable cardioverter defibrillator and precipitating factors. Pacing Clin Electrophysiol 29(6):619–626. https://doi.org/10.1111/j.1540-8159.2006.00409.x
Luyster FS, Hughes JW, Waechter D, Josephson R (2006) Resource loss predicts depression and anxiety among patients treated with an implantable cardioverter defibrillator. Psychosom Med 68(5):794–800. https://doi.org/10.1097/01.psy.0000227722.92307.35
Pedersen SS, van Domburg RT, Theuns DA, Jordaens L, Erdman RA (2005) Concerns about the implantable cardioverter defibrillator: a determinant of anxiety and depressive symptoms independent of experienced shocks. Am Heart J 149(4):664–669. https://doi.org/10.1016/j.ahj.2004.06.031
Whang W, Albert CM, Sears SF, Lampert R, Conti JB, Wang PJ, Singh JP, Ruskin JN, Muller JE, Mittleman MA, Investigators TS (2005) Depression as a predictor for appropriate shocks among patients with implantable cardioverter-defibrillators - results from the Triggers of Ventricular Arrhythmias (TOVA) study. J Am Coll Cardiol 45(7):1090–1095. https://doi.org/10.1016/j.jacc.2004.12.053
Kramer T, Als L, Garralda ME (2015) Challenges to primary care in diagnosing and managing depression in children and young people. BMJ 350
Krebber A, Buffart L, Kleijn G, Riepma I, De Bree R, Leemans C, Becker A, Brug J, Van Straten A, Cuijpers P (2014) Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psycho-Oncology 23(2):121–130
Kim HJ, Park E, Storr CL, Tran K, Juon H-S (2015) Depression among Asian-American adults in the community: systematic review and meta-analysis. PLoS One 10(6):e0127760
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC (2018) Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep 8(1):2861
World Health Organization (2017) Depression and other common mental disorders: global health estimates. World Health Organization
Read JR, Sharpe L, Modini M, Dear BF (2017) Multimorbidity and depression: a systematic review and meta-analysis. J Affect Disord 221:36–46
Ghaemmohamadi MS, Behzadifar M, Ghashghaee A, Mousavinejad N, Ebadi F, Shahri SSS, Seyedin H, Behzadifar M, Bragazzi NL (2018) Prevalence of depression in cardiovascular patients in Iran: a systematic review and meta-analysis from 2000 to 2017. J Affect Disord 227:149–155
Yanping R, Hui Y, Browning C, Thomas S, Meiyan L (2014) Prevalence of depression in coronary heart disease in China: a systematic review and meta-analysis. LWW
Williams R, Murray A (2015) Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil 96(1):133–140
Palmer S, Vecchio M, Craig JC, Tonelli M, Johnson DW, Nicolucci A, Pellegrini F, Saglimbene V, Logroscino G, Fishbane S (2013) Prevalence of depression in chronic kidney disease: systematic review and meta-analysis of observational studies. Kidney Int 84(1):179–191
Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A (2016) Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Psychoneuroendocrinology 70:70–84
Qin X, Wang S, Hsieh C-R (2018) The prevalence of depression and depressive symptoms among adults in China: estimation based on a National Household Survey. China Econ Rev 51:271–282
Linardakis M, Papadaki A, Smpokos E, Micheli K, Vozikaki M, Philalithis A (2015) Peer reviewed: association of behavioral risk factors for chronic diseases with physical and mental health in European adults aged 50 years or older, 2004–2005. Prev Chronic Dis 12
Voinov B, Richie WD, Bailey RK (2013) Depression and chronic diseases: it is time for a synergistic mental health and primary care approach. Prim Care Companion CNS Disord 15(2)
De Hert M, Detraux J, Vancampfort D (2018) The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin Neurosci 20(1):31–40
Vaccarino V, Badimon L, Bremner JD, Cenko E, Cubedo J, Dorobantu M, Duncker DJ, Koller A, Manfrini O, Milicic D (2019) Depression and coronary heart disease: 2018 ESC position paper of the working group of coronary pathophysiology and microcirculation developed under the auspices of the ESC Committee for Practice Guidelines. Eur Heart J
Carney RM, Freedland KE (2017) Depression and coronary heart disease. Nat Rev Cardiol 14(3):145–155
Sears SF, Hauf JD, Kirian K, Hazelton G, Conti JB (2011) Posttraumatic stress and the implantable cardioverter-defibrillator patient what the electrophysiologist needs to know. Circ Arrhythm Electrophysiol 4(2):242–250. https://doi.org/10.1161/CIRCEP.110.957670
Thylen I, Moser DK, Stromberg A, Dekker RA, Chung ML (2016) Concerns about implantable cardioverter-defibrillator shocks mediate the relationship between actual shocks and psychological distress. Europace 18(6):828–835. https://doi.org/10.1093/europace/euv220
Seo J, Choi B, Kim S, Lee H, Oh D (2017) The relationship between multiple chronic diseases and depressive symptoms among middle-aged and elderly populations: results of a 2009 Korean community health survey of 156,747 participants. BMC Public Health 17(1):844
O’Donnell S, Rusu C, Hawker GA, Bernatsky S, McRae L, Canizares M, MacKay C, Badley EM (2015) Arthritis has an impact on the daily lives of Canadians young and old: results from a population-based survey. BMC Musculoskelet Disord 16(1):230
Berry CE, Han MK, Thompson B, Limper AH, Martinez FJ, Schwarz MI, Sciurba FC, Criner GJ, Wise RA (2015) Older adults with chronic lung disease report less limitation compared with younger adults with similar lung function impairment. Ann Am Thorac Soc 12(1):21–26
Laudański K, Nowak Z, Niemczyk S (2013) Age-related differences in the quality of life in end-stage renal disease in patients enrolled in hemodialysis or continuous peritoneal dialysis. Med Sci Monitor 19:378
Bisschop MI, Kriegsman DM, Deeg DJ, Beekman AT, van Tilburg W (2004) The longitudinal relation between chronic diseases and depression in older persons in the community: the Longitudinal Aging Study Amsterdam. J Clin Epidemiol 57(2):187–194
Egede LE, Zheng D, Simpson K (2002) Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 25(3):464–470
Egede LE (2004) Effects of depression on work loss and disability bed days in individuals with diabetes. Diabetes Care 27(7):1751–1753
Egede LE (2004) Diabetes, major depression, and functional disability among US adults. Diabetes Care 27(2):421–428
Holzer BM, Siebenhuener K, Bopp M, Minder CE (2017) Evidence-based design recommendations for prevalence studies on multimorbidity: improving comparability of estimates. Popul Health Metrics 15(1):9
Kassebaum N, Smith A, Bernabé E, Fleming T, Reynolds A, Vos T, Murray C, Marcenes W, Collaborators GOH (2017) Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990–2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res 96(4):380–387
Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, De Girolamo G, De Graaf R, Demyttenaere K, Hu C, Iwata N (2011) Cross-national epidemiology of DSM-IV major depressive episode. BMC Med 9(1):90
Rai D, Zitko P, Jones K, Lynch J, Araya R (2013) Country-and individual-level socioeconomic determinants of depression: multilevel cross-national comparison. Br J Psychiatry 202(3):195–203
Pacheco JPG, Silveira JB, Ferreira RPC, Lo K, Schineider JR, Giacomin HTA, San Tam WW (2019) Gender inequality and depression among medical students: a global meta-regression analysis. J Psychiatr Res 111:36–43
Trivedi MH, Wisniewski SR, Nierenberg AA, Gaynes BN, Warden D, Morris MDW, Luther JF, Farabaugh A, Cook I, Rush AJ (2010) Health-related quality of life in depression: a STAR* D report. Ann Clin Psychiatry 22(1):43–55
Mayor S (2015) Persistent depression doubles stroke risk despite treatment, study finds. BMJ 350:h2611
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception or design of the work: Mohammadreza Razavi, Khodayar Oshvandi, and Mahnaz Khatiban. Acquisition, analysis, or interpretation of data for the work: Mohammadreza Razavi and Reza Ghanei Gheshlagh. Drafting the work or revising it critically for important intellectual content: Mohammadreza Razavi, Khodayar Oshvandi, and Mahnaz Khatiban. Final approval of the version to be published: Mohammadreza Razavi, Khodayar Oshvandi, and Mahnaz Khatiban. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: Mohammadreza Razavi, Khodayar Oshvandi, Mahnaz Khatiban, and Reza Ghanei Gheshlagh.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oshvandi, K., Khatiban, M., Ghanei Gheshlagh, R. et al. The prevalence of depression in patients living with implantable cardioverter defibrillator: a systematic review and meta-analysis. Ir J Med Sci 189, 1243–1252 (2020). https://doi.org/10.1007/s11845-020-02208-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-020-02208-4