Abstract
Objectives
Currently in Ireland, there is a lack of uniformity regarding the method in which the consent process is routinely documented. The purpose of this study was to evaluate the standard consent forms used in elective orthopaedic hospitals in Ireland. In addition, this paper explores the relevant guidelines from the UK and Ireland relating to consent documentation.
Methods
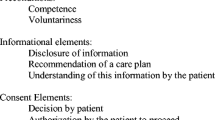
Standard consent forms used in the 24 public hospitals that perform elective orthopaedic surgery were analysed and compared, based on the inclusion or exclusion of 22 unique consent-related items or statements selected by the authors. In addition, each form was analysed for format, word count, and readability.
Results
Within 24 hospitals with elective orthopaedic surgery, there were 21 unique consent forms being used. There was a mean inclusion of 9.5 of the 22 unique items per form with a standard deviation of 5.1 (range 2–18), indicating a wide discrepancy. For each unique consent-related item in the analysis, the mean rate of inclusion was 43.4% (SD 26.7%). The mean Flesch Reading Ease Score was 43.3. The format varied from 1 to 4 pages, with a word count of 109 to 1041 (mean 414.7).
Conclusion
The findings demonstrate a lack of uniformity of both format and content amongst the consent forms currently being used in elective orthopaedic hospitals in Ireland. This paper supports the use of a nationally standardised consent documentation method in order to improve the efficiency of the consent process and ensure greater protection against litigation.



Similar content being viewed by others
References
Atrey A, Gupte CM, Corbett SA (2010) Review of successful litigation against English health trusts in the treatment of adults with orthopaedic pathology: clinical governance lessons learned. J Bone Joint Surg Am 92(18):e36
Bhattacharyya T, Yeon H, Harris MB (2005) The medical-legal aspects of informed consent in orthopaedic surgery. J Bone Joint Surg Am 87(11):2395–2400
Skene L, Smallwood R (2002) Informed consent: lessons from Australia. BMJ (Clin Res Ed) 324(7328):39–41
Tarantino U, Giai Via A, Macri E, Eramo A, Marino V, Marsella LT (2013) Professional liability in orthopaedics and traumatology in Italy. Clin Orthop Relat Res 471(10):3349–3357
Beresford-Cleary NJ, Halliday J, Breusch SJ, Biant LC (2011) Consent process for elective total hip and knee arthroplasty. J Orthop Surg (Hong Kong) 19(3):274–278
Murphy K, Shafiq A, Corrigan MA, Redmond HP (2011) A descriptive study of consent documentation. Ir Med J 104(8):238–240
National Consent Policy (2014), http://www.hse.ie/eng/about/Who/qualityandpatientsafety/National_Consent_Policy (last accessed 01/02/17)
Reference Guide to Consent for Examination or Treatment (Second Edition), Department of Health UK, https://www.gov.uk/government/publications/reference-guide-to-consent-for-examination-or-treatment-second-edition (last accessed 01/02/17)
Khan IH, Jamil W, Lynn SM, Khan OH, Markland K, Giddins G (2012) Analysis of NHSLA claims in orthopedic surgery. Orthopedics 35(5):e726–e731
Foy MA (2015) Informed consent: where are we in 2015? Bone Joint J 97-b(9):1159–1161
Montgomery v Lanarkshire Health Board (2015). UKSC 11 (On appeal from (2013) CSIH 3; (2010) CSIH 104)
Bolam v Friern Hospital Management Committee (1957). 1 WLR 582, 587
Guide to Professional Conduct and Ethics for Medical Practitioners 8th Edition (2016), Irish Medical Council, https://www.medicalcouncil.ie/News-and-Publications/Reports/Guide-to-Professional-Conduct-and-Ethics-8th-Edition-2016-.pdf (last accessed 01/02/17)
National policy and procedure for safe surgery, http://www.hse.ie/eng/about/Who/qualityandpatientsafety/safepatientcare/Safe_Surgery (last accessed 01/02/17)
Consent: patients and doctors making decisions together, General Medical Council, http://www.gmc-uk.org/guidance/ethical_guidance/consent_guidance_index.asp (last accessed 01/02/17)
Clarke K, O'Loughlin P, Cashman J (2015) Standardized Consent: The Effect of Information Sheets on Information Retention. J Patient Saf. https://doi.org/10.1097/PTS.0000000000000230
Ibrahim T, Ong SM, Taylor GJ (2004) The new consent form: is it any better? Ann R Coll Surg Engl 86(3):206–209
Shurnas PS, Coughlin MJ (2003) Recall of the risks of forefoot surgery after informed consent. Foot Ankle Int 24(12):904–908
Crepeau AE, McKinney BI, Fox-Ryvicker M, Castelli J, Penna J, Wang ED (2011) Prospective evaluation of patient comprehension of informed consent. J Bone Joint Surg Am 93(19):e114 (1–7)
Lemaire R (2006) Informed consent–a contemporary myth? J Bone Joint Surg Br Vol 88(1):2–7
Saigal R, Clark AJ, Scheer JK, Smith JS, Bess S, Mummaneni PV, McCarthy IM, Hart RA, Kebaish KM, Klineberg EO, Deviren V, Schwab F, Shaffrey CI, Ames CP (2015) Adult spinal deformity patients recall fewer than 50% of the risks discussed in the informed consent process preoperatively and the recall rate worsens significantly in the postoperative period. Spine 40(14):1079–1085
Robinson G, Merav A (1976) Informed consent: recall by patients tested postoperatively. Ann Thorac Surg 22(3):209–212
Mussa MA, Sweed TA, Khan A (2014) Informed consent documentation for total hip and knee replacement using generic forms with blank spaces. J Orthop Surg (Hong Kong) 22(2):214-217
Singh S, Mayahi R (2004) Consent in orthopaedic surgery. Ann R Coll Surg Engl 86(5):339–341
Jeyaseelan L, Ward J, Papanna M, Sundararajan S (2010) Quality of consent form completion in orthopaedics: are we just going through the motions? J Med Ethics 36(7):407–408
Kheiran A, Banerjee P, Stott P (2014) Consenting operative orthopaedic trauma patients: challenges and solutions. ISRN Surgery 2014:354239
Isherwood J, Dean B, Pandit H (2013) Documenting informed consent in elective hip replacement surgery: a simple change in practice. Br J Hosp Med (Lond) 74(4):224-227
Barritt AW, Clark L, Teoh V, Cohen AM, Gibb PA (2010) Assessing the adequacy of procedure-specific consent forms in orthopaedic surgery against current methods of operative consent. Ann R Coll Surg Engl 92(3):246–249 quiz 2p following 9
Atrey A, Leslie I, Carvell J, Gupte C, Shepperd JA, Powell J et al (2008) Standardised consent forms on the website of the British Orthopaedic Association. J Bone Joint Surg Br Vol 90(4):422–423
Chatterton V. Gerson (1981) QB 432
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Robert Kenyon declares that he has no conflict of interest.
Author Eoghan Pomeroy declares that he has no conflict of interest.
Author Robert Yeo declares that he has no conflict of interest.
Author James Cashman declares that he has no conflict of interest.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Kenyon, R.M., Pomeroy, E., Yeo, R. et al. Consent documentation for elective orthopaedic surgery. Ir J Med Sci 188, 861–866 (2019). https://doi.org/10.1007/s11845-018-1929-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-018-1929-4