Abstract
Introduction
To examine the added diagnostic value of emergent contrast enhanced CT head (CECTH) in patients who present to the emergency department (ED) with acute non-traumatic symptoms referable to the brain, and to assess the financial implications of CECTH in the emergent setting.
Materials and methods
We queried healthcare data for head CTs ordered by our ED between January 2008 and December 2010. Those who presented to the ED with non-traumatic neurologic disturbances were included. All traumatic head injury cases were excluded. Two board certified radiologists with fellowship training who were blinded to patient history and physical findings, independently reviewed all non-contrast computed tomography of the head (NCTH) and CECTH images. CECTH’s were read following abnormal NCTH’s, and findings were recorded as normal or abnormal.
Results
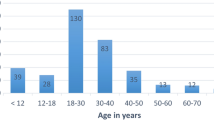
In our investigation, 379 patients—210 (55 %) females and 169 (45 %) males—met the inclusion criteria. Common indications for head CT included: headache 183 (48 %); dizziness 73 (19 %); altered mental status 49 (13 %); and seizure 38 (10 %). The mean age of study subjects was 47 (±29) years. Two hundred sixty-one (69 %) of all patients scanned showed no abnormality. One hundred eighteen (31 %) of 379 patients had abnormal scans. We encountered 1 abnormal CECTH on which NCTH was normal. Cost of CECTH was $465 and NCTH was $385.
Conclusion
Head CT in ED non-traumatic neurological presentations with CECTH is not generally indicated and represents a calculable cost savings in the management of these patients.
Similar content being viewed by others
References
af Geijerstam JL, Oredsson S, Britton M, Investigators OS (2006) Medical outcome after immediate computed tomography or admission for observation in patients with mild head injury: randomised controlled trial. BMJ 333(7566):465
Wood LP, Parisi M, Finch IJ (1990) Value of contrast enhanced CT scanning in the non-trauma emergency room patient. Neuroradiology 32(4):261–264
Demaerel P, Buelens C, Wilms G, Baert AL (1998) Cranial CT revisited: do we really need contrast enhancement? Eur Radiol 8(8):1447–1451
Fakhran S, Alhilali L, Branstetter BF (2013) Yield of CT angiography and contrast-enhanced MR imaging in patients with dizziness. AJNR Am J Neuroradiol 34(5):1077–1081
Demaerel P, Wilms G, Baert AL (1995) Is contrast enhancement in cranial computed tomography necessary? Lancet 345(8946):389
Elicker BM, Cypel YS, Weinreb JC (2006) IV contrast administration for CT: a survey of practices for the screening and prevention of contrast nephropathy. AJR Am J Roentgenol 186(6):1651–1658
Davenport MS, Khalatbari S, Cohan RH, Dillman JR, Myles JD, Ellis JH (2013) Contrast material-induced nephrotoxicity and intravenous low-osmolality iodinated contrast material: risk stratification by using estimated glomerular filtration rate. Radiology 268(3):719–728
Horowitz SH (2007) The diagnostic workup of patients with neuropathic pain. Med Clin North Am 91(1):21–30
Kunkel RS (1979) Evaluating the headache patient: history and workup. Headache 19(3):122–126
Mebust D (2013) Image diagnosis: headache and an isolated oculomotor nerve palsy. Perm J. 17(3):e120
Savji N, Rockman CB, Skolnick AH, Guo Y, Adelman MA, Riles T et al (2013) Association between advanced age and vascular disease in different arterial territories: a population database of over 3.6 million subjects. J Am Coll Cardiol 61(16):1736–1743
Aragon-Ching JB, Zujewski J (2007) CNS metastasis: an old problem in a new guise. Clin Cancer Res 13(6):1644–1647
Reinus WR, Zwemer FL (1994) Clinical prediction of emergency cranial computed tomography results. Ann Emerg Med 23(6):1271–1278
Rothrock SG, Buchanan C, Green SM, Bullard T, Falk JL, Langen M (1997) Cranial computed tomography in the emergency evaluation of adult patients without a recent history of head trauma: a prospective analysis. Acad Emerg Med 4(7):654–661
Hill RG, Sears LM, Melanson SW (2013) 4000 Clicks: a productivity analysis of electronic medical records in a community hospital ED. Am J Emerg Med 31(11):1591–1594
Trzeciak S, Rivers EP (2003) Emergency department overcrowding in the United States: an emerging threat to patient safety and public health. Emerg Med J 20(5):402–405
Affleck A, Parks P, Drummond A, Rowe BH, Ovens HJ (2013) Emergency department overcrowding and access block. CJEM 15(6):359–370
de Araujo P, Khraiche M, Tukan A (2013) Does overcrowding and health insurance type impact patient outcomes in emergency departments? Health Econ Rev 3(1):25
Shuaib W, Tiwana MH (2014) Interdepartmental communication. Ir J Med Sci 183(1):151–152
Masdeu JC, Drayer BP, Anderson RE, Braffman B, Davis PC, Deck MD et al (2000) Atraumatic isolated headache–when to image. American College of Radiology. ACR appropriateness criteria. Radiology 215(Suppl):487–493
Shuaib W, Khosa F (2013) Voicing reason. J Radiol Radiat Ther 1:1003
Sarwar A, Ding A, Slanetz PJ (2013) Getting involved in organized medicine–a remedy for the current health care crisis? Acad Radiol 20(4):519–520
Shuaib W, Vijayasarathi A, Tiwana MH, Johnson JO, Maddu KK, Khosa F (2014) The diagnostic utility of rib series in assessing rib fractures. Emerg Radiol 21(2):159–164
Shuaib W, Khan AA, Mehta AS, Vijayasarathi A, Hidalgo J (2014) Utility of CT angiography in cervical spine trauma: analysis of radiation and cost. Int J Cancer Ther Oncol 2(4):02043. doi:10.14319/ijcto.0204.3
Smith-Bindman R, Lipson J, Marcus R, Kim K, Mahesh M, Gould R, Berrington de Gonzalez A, Miglioretti DL (2009) Radiation dose associated with attributable risk of 327 cancer. Arch Intern Med 169(22):2078–2086
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
F. Khosa: American Roentgen Ray Society Scholar (2013–2015).
Rights and permissions
About this article
Cite this article
Shuaib, W., Tiwana, M.H., Chokshi, F.H. et al. Utility of CT head in the acute setting: value of contrast and non-contrast studies. Ir J Med Sci 184, 631–635 (2015). https://doi.org/10.1007/s11845-014-1191-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-014-1191-3