Abstract
Background
The practice of fasting from midnight prior to surgery is an outdated one.
Aims
The aim of this study was to assess the impact of an evidence-based protocol for reduced preoperative fasting on fasting times, patient safety, and comfort.
Methods
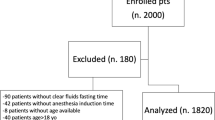
A non-randomised case–control study of preoperative fasting times among adult surgical patients undergoing elective procedures was conducted. Consecutive patients were allocated to a reduced preoperative fasting protocol allowing fluids and solids up to 2 and 6 h prior to anaesthesia, respectively (n = 21). These were compared to control patients identified from an historic study of preoperative fasting times who followed the traditional fast from midnight (n = 29). Fasting times and details of patients’ subjective comfort were collected using an interview-assisted questionnaire. Incidence of intraoperative aspirations was obtained from anaesthetic records.
Results
Significant reductions in fasting times for fluids (p = 0.000) and solids (p = 0.000) were achieved following implementation of the fasting protocol. Less preoperative thirst (0.000), headache (0.012) and nausea (0.015) were reported by those who had a shorter fast. Intraoperative aspiration did not occur in either group.
Conclusion
Implementation of this protocol for reduced preoperative fasting achieved an appreciable reduction in fasting times and enhanced patient comfort. Patient safety was not compromised. Further modifications of our protocols are necessary to meet the international best practice. We recommend its implementation across all surgical groups in our institution.
Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- GI:
-
Gastrointestinal
- ERAS:
-
Enhanced recovery after surgery
References
Lister J (1883) On anaesthetics, part III. In: Holmes’ system of surgery. vol 3, 3rd ed. Longmans Green and Company, London (Reprinted in: The collected papers of Joseph Lister (1979) Classics of Medicine Library, Birmingham, pp 171–172)
Brady MC, Kinn S, Stuart P, Ness V (2003) Preoperative fasting for adults to prevent perioperative complications. Cochrane Database of Systematic Reviews , Issue 4. Art. No.: CD004423. doi:10.1002/14651858.CD004423
De Auguilar-Nascimento JE, Borges Dock-Nascimento D (2010) Reducing preoperative fasting time: a trend based on evidence. World J Gastrointest Surg 2(3):57–60
De Aguilar-Nascimentio JE, Bicudo-Salomão A, Caporossi C, Silva RM, Santos TP (2008) Enhancing surgical recovery in Central-West Brazil: the ACERTO protocol results. Eur J Clin Nutr Metab 3:e78–e83
Schricker T (2001) The catabolic response to surgery: how can it be modified by the anesthesiologist? Can J Anesth 48(6):R1–R5
Diks J, Van Hoorn DEC, Nijveldt RJ et al (2005) Preoperative fasting: an outdated concept? J Parenter Enter Nutr 29:298–304
Søreide E, Fasting S, Raeder J (1997) New preoperative fasting guidelines in Norway. Acta Anaesthesiol Scand 41:799
Warner M, Caplan R, Epstein B et al (1999) Practise guidelines for preoperative fasting and the use of pharmacological agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures. A Report by the American Society of Anesthesiologists Task Force on Preoperative Fasting. Anesthesiology 90(3):896–905
Symposium Report. The shortened fluid fast and the Canadian Anaesthetists’s Society’s new guidelines for fasting in elective/emergency patients (1990). Can J Anest 37: 906
AAGBI safety guideline. Pre-operative assessment and the role of the anaesthetist (2010) The Association of Anaesthetists of Great Britain and Ireland. http://www.aagbi.org/publications/guidelines/docs/preoperativeass01.pdf. Accessed 11 Jan 2011
Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, Jauch KW, Kemen M, Hiesmayr JM, Horbach T, Kuse ER, Vestweber KH, DGEM (German Society for Nutritional Medicine) (2006) ESPEN guidelines on enteral nutrition: surgery including organ transplantation. Clin Nutr 25(2):224–244
Powell-Tuck J, Gosling P, Lobo DN et al (2009) British consensus guidelines on intravenous fluid therapy for adult surgical patients (GIFTASUP). http://www.bapen.org.uk/pdfs/bapen_pubs/giftasup.pdf. Accessed 8 Jan 2011
Fearon KC, Ljungqvist O, Von Meyenfeldt M et al (2005) Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 24:466–477
Lassen K, Soop M, Nygren J, Enhanced Recovery After Surgery (ERAS) Group et al (2009) Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg 144(10):961–969
Heyland D, Cahill N, Dhaliwal R (2010) Lost in (Knowledge) Translation! J Parenter Enteral Nutr 34(6):610–615
McConnell G, Cronin K, Smyth N, Andrews E, Keane F, Neary P (2008) An analysis of routine fasting practices in surgical patients. Abstracts of the 33rd Sir Peter Freyer Memorial Lecture and Surgical Symposium. Ir J Med Sci 177(S7):S204
Al Chalabi H, Kavanagh DO, Hassan L et al (2010) The benefit of an enhanced recovery programme following elective laparoscopic sigmoid colectomy. Int J Colorectal Dis 25(6):761–766
American Society of Anesthiologists (1963) New classification of physical status. Anesthesiology 24: 111
Fasting S, Søreide E, Raeder JC (1998) Changing preoperative fasting policies. Impact of a national consensus. Acta Anaesthesiol Scand 42(10):1188–1191
Maltby J, Lewis P, Martin A, Sutheriand LR (1991) Gastric fluid volume and pH in elective patients following unrestricted oral fluid until three hours before surgery. Can J Anaesth 38(4 Pt 1):425–429
Meisner M, Ernhofer U, Schmidt J (2008) Liberalisation of preoperative fasting guidelines: effects on patient comfort and clinical practicability during elective laparoscopic surgery of the lower abdomen. Zentralbl Chir 133(5):479–485
Kavanagh DO, Gibson D, Moran DC et al (2011) Short-term outcomes following laparoscopic resection for colon cancer. Int J Colorectal Dis 26(3):361–368
Acknowledgments
The authors wish to acknowledge the support of the theatre nurses and the nursing staff on Gogarty and Crampton Wards in the Adelaide and Meath Hospital Incorporating the National Childrens’ Hospital. Thank you to the surgical and anaesthetic teams for their participation in the study. Thank you to M. Roddy and S. Duggan for their expertise.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article was presented in the conference presentation of Irish Society of Gastroenterology (ISGE) Winter Meeting, Mullingar, Co., Westmeath on November 25th and 26th 2010.
Rights and permissions
About this article
Cite this article
Power, S., Kavanagh, D.O., McConnell, G. et al. Reducing preoperative fasting in elective adult surgical patients: a case–control study. Ir J Med Sci 181, 99–104 (2012). https://doi.org/10.1007/s11845-011-0765-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-011-0765-6