Abstract
Purpose
To (1) identify the prevalence of sleep problems in cancer survivors across cancer types and survivorship durations compared to a normative population and (2) determine demographic, clinical, lifestyle, and psychosocial determinants.
Method
Cancer survivors diagnosed between 2008 and 2015 (N = 6736) and an age- and sex-matched normative cohort (n = 415) completed the single sleep item of the EORTC QLQ-C30: Have you had trouble sleeping? Participants who responded with “quite a bit”/ “very much” were categorized as poor sleepers. A hierarchical multinomial logistic regression was used to identify determinants of sleep problems.
Result
The prevalence of sleep problems was higher in cancer survivors (17%) compared to the normative population (11%) (p < 0.001), varied across cancer types (10–26%) and did not vary based on survivorship duration. The full model showed that survivors who were female (adjusted odds ratio (AOR) 2.26), overweight (AOR 1.50), had one (AOR 1.25) and ≥ 2 comorbidities (AOR 2.15), were former (AOR 1.30) and current (AOR 1.53) smokers and former alcohol drinkers (AOR 1.73), had a higher level of fatigue (AOR 1.05), anxiety (AOR 1.14), depression (AOR 1.11), and cognitive illness perceptions (AOR 1.02), had a higher odds for sleep problems. Higher education compared to lower education (AOR 0.67), having a partner (AOR 0.69), and obesity compared to normal BMI (AOR 0.86) were protective to sleep problems as well as high physical activity before adjusting for psychological factors (AOR 0.91).
Conclusion
Modifiable determinants of sleep problems include physical activity, fatigue, anxiety, depression, and illness perception.
Implications for Cancer Survivors
Sleep problems after cancer deserve clinical attention. They may be improved by addressing modifiable lifestyle factors: increasing physical activity, stop smoking, and reducing alcohol consumption. As fatigue, depression, and illness perception seem related to sleep problems, lifestyle improvements may also improve these outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep problems are a common problem in cancer survivors—individuals with a cancer diagnosis, extended treatment, and advanced cancer [1,2,3,4]. Sleep problems have been shown to be associated with increased distress, morbidity, reduced productivity (daytime functioning), and poor health-related quality of life (HRQoL) in cancer survivors [5,6,7].
The burden of sleep problems in cancer survivors is higher when compared to the general population affecting 20–70% of treated individuals [8,9,10,11,12] and varies across cancer types. Studies have demonstrated sleep problems in up to 17% of prostate cancer survivors, 47% of colorectal cancer survivors, 59% of ovarian cancer survivors, and 72% of endometrium cancer survivors [5, 13,14,15]. However, fewer studies have compared sleep problems among survivors of different cancer types, those being longer post diagnosis (> 5 years) and those receiving different types of cancer treatment [6, 8, 9]. Additionally, a limitation in many studies has been a small sample size when investigating the prevalence across cancer types [2, 14, 16], and only few studies included a matched normative population for comparison with the general population’s prevalence [4, 8, 9].
Various determinants have been associated with sleep problems in cancer survivors. Demographic factors included lower age, female sex, higher education, and not being able to work to be associated with sleep problems [1, 3, 6, 8, 9, 11, 14, 17,18,19,20]. Clinical factors included higher body mass index (BMI), cancer type and higher stage during diagnosis, type of treatment (chemotherapy and radiotherapy), shorter time since diagnosis, and the presence of comorbidities [5, 6, 8, 9, 14, 19, 20]. Lifestyle factors such as smoking, drinking alcohol, and not being physically active have shown to be significantly associated with sleep problems [8, 9, 18]. Lastly, various psychosocial factors including anxiety, depression, and fatigue have been negatively associated with sleep problems among cancer survivors [8, 9, 13, 14, 21,22,23]. Because literature shows that illness perception is associated with fatigue, anxiety, and depression among cancer survivors [24,25,26], it is also likely to be related to sleep problems.
Although these associations are well described, there is a lack of evidence that addresses all these determinants together with several types of cancer in one single study. Investigating both demographic and clinical data together with modifiable lifestyle and psychosocial factors will not only give an indication which cancer survivors are at risk of sleep problems, it will also give an indication for the development of interventions. Furthermore, it is important to assess all possible factors in a single study to address the effect of potential confounding.
This study aimed to assess the prevalence of sleep problems in cancer survivors compared to an age- and sex-matched normative population, among survivors with different cancer types (colon, rectum, prostate, ovarian, thyroid, endometrium, Hodgkin and non-Hodgkin lymphoma, chronic lymphocytic leukemia, melanoma, multiple myeloma, and basal/squamous cell carcinoma) and according survivorship duration post diagnosis. The second aim was to identify various demographic, clinical, lifestyle, and psychosocial determinants that were associated with sleep problems. The results from this study aim to increase insights into cancer survivors who have a higher risk of sleep problems to create awareness among medical professionals.
Methods
Study design
This study is a secondary quantitative data analysis of a cross-sectional population-based sample from the Patient Reported Outcome Following Initial treatment and Long-term Evaluation of Survivorship (PROFILES) registry in The Netherlands. PROFILES is a registry facilitating data collection on patient-reported outcomes from cancer survivors. Its main objectives are psychosocial risk and outcome assessment, understanding biological and behavioral factors associated with cancer treatment outcomes, and evaluating cancer survivors physical and psychological care needs [27]. Patients for this study were included between May 2008 and April 2015.
Study population and selection procedure
Cancer survivors were selected from the Netherlands Cancer Registry, which contains data of all newly diagnosed cancer patients in the Netherlands since 1989. Cancer survivors (N = 10,304) who were diagnosed between 2008 and 2015with endometrium cancer, colorectal cancer, Hodgkin and non-Hodgkin lymphomas, multiple myeloma, chronic lymphocytic leukemia, thyroid cancer, prostate cancer, ovarian and borderline ovarian cancer, basal/squamous cell carcinoma, and melanoma in selected hospitals were eligible [27, 28]. To adopt a generalized few across cancers, we selected as wide a variety of tumor types as possible such as common tumor types and rare tumor types, solid tumors and hematologic tumors, and tumors that occur only in men or women vs. tumors that occur in both. These cancer survivors were asked to participate in the study by an invitation letter from their former/treating physician. Participants signed the informed consent forms and completed the questionnaires (digital or by paper and pencil) [27]. Inclusion criteria were the capability of reading and writing the Dutch language and completing self-reported questionnaires without extensive assistance [27]. People who died or emigrated before the start of the studies were excluded (according to data from the hospital of diagnosis and the Dutch municipal record database) [28]. Non-participation in the study had no consequence on the treatment or any follow-up care, and there was no risk/harm to the participants [27]. Ethical approval was obtained from a local certified medical ethics committee.
The PROFILES registry also contained a reference cohort of adult individuals (N = 1557) from the general Dutch population [27]. This data was generated by CentERdata (www.centerdata.nl), a Dutch research institute, and comes from the LISS panel which is part of CentERdata NL (https://www.centerdata.nl/liss-panel). The LISS panel aims to provide a good representation of the Dutch population for research purposes. The panel is probability based and uses the sample of households from the population register of Statistics Netherlands (CBS). Respondents were asked whether they have had cancer in the past, and if so, they were removed from the dataset. On an annual basis, the participants of this CentERpanel were asked to complete various questionnaires similar to the ones used in PROFILES [27]. Participants from this reference cohort were matched overall and with each cancer type on age and sex to create normative populations.
Measurement instruments
Sleep problems (outcome)
Sleep problems were measured using a single item of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ)-C30: “During the past week—Have you had trouble sleeping?” Participants could answer by selecting one of the four options: not at all, a little, quite a bit, and very much. For the analyses, answers were recoded into three categories: survivors with no sleep problems (people who did not have any trouble sleeping), moderate sleep problems (people who had little trouble sleeping), and many sleep problems (people who had quite a bit and very much trouble sleeping) [29]. This aligned with the threshold for clinical cut off that was identified in the literature by Giesinger et al. [30, 31], differentiating between poor vs. good/moderate sleep quality. Furthermore, the EORTC QLQ-C30 is a well-validated and reliable questionnaire to assess HRQoL [32]. The single sleep item of the EORTC QLQ-C30 appeared in previous research as a sufficient measure to study sleep at group level, and we found in a previous study that the sleep item was highly correlated (r = 0.71) with the total score of the Pittsburgh Sleep Quality Index (PSQI) [33, 34].
Determinants of sleep quality
The determinants of interest in this study were the variables from the literature that have previously shown to be associated with sleep problems [1,2,3, 5, 6, 8, 9, 14, 15, 18].
Demographic
Demographic factors included age, sex, marital status, level of education, and working status. The variable sex was categorized as male and female. Marital status was categorized as having a partner (married or cohabiting) and not having a partner (divorced/separated/widowed/never married/never cohabited). Level of education was categorized as low (less than high school), secondary (high school or vocational), and high (bachelor’s or master’s education). Current working status was categorized as yes or no.
Clinical
Data for cancer type, stage (tumor, node, metastasis (TNM) except for lymphomas, multiple myeloma (MM), and chronic lymphocytic leukemia (CLL)), primary treatment (surgery, radiotherapy, chemotherapy, and systemic and hormonal therapy), time since diagnosis (< 2, ≥ 2 to < 3, ≥ 3 to < 5, and ≥ 5 years), and comorbidities (0, 1, ≥ 2 comorbidities)) were obtained from the Netherlands Cancer Registry.
Lifestyle
Data on smoking (no, former, yes), alcohol use (no, former, yes), physical activity (hours of moderate to vigorous physical activity (MVPA) per week), and body height and weight (body mass index (BMI), kg/m2) were self-reported. Physical activity was recorded using the European Perspective Investigation of Cancer, EPIC physical activity questionnaire wherein MVPA was derived using metabolic equivalents (MET), the ratio of a person’s resting metabolic rate compared to the metabolic rate during a specific activity. A MET score of 1 represents the amount of energy used at rest while a score of 3–6 is categorized as moderate and any activity above 6 MET as vigorous physical activity [35]. For the analyses, we categorized MVPA/week into tertiles (MVPA/week 0–6 = lowest, 6.01–12.05 = middle, and 12.6––49 = highest).
Psychosocial
Fatigue was assessed using the Fatigue Assessment Scale (FAS). The FAS is a 10-item scale that evaluates chronic fatigue as a unidimensional construct. The items are directed towards the usual feeling of the participant about how fatigue affects their functioning. All ten items are scored on a 5-point scale never/sometimes/regularly/often/always. The total score is the sum score of all items ranging from 10 to 50; a total score of ≥ 22 indicates fatigue [36]. The FAS has shown high reliability, content validity, and internal consistency (Cronbach’s α = 0.87), in the Dutch population [37].
Anxiety and depression were assessed using the Hospital Anxiety and Depression scale (HADS). The HADS is a 14-item self-reported questionnaire frequently used in oncology and other physical health settings to screen participants’ emotional distress. Participants answer questions about anxiety and depressive symptoms (seven items each) on a scale of 0–3. A higher score is associated with a higher level of anxiety and depression (0–7 = normal, 8–10 = borderline anxiety or depressive symptoms) [38]. The cutoff sum score of ≥ 15 on the full scale has shown a sensitivity of 80%, a specificity of 76%, and a positive predictive value of 41% when compared to the general health questionnaire (GHQ 28) and Rotterdam symptom checklist (RSCL) [39].
Illness perception was measured using the Brief illness perception questionnaire (BIPQ). The BIPQ is an eight-item self-reported questionnaire used to measure cognitive (5 items; consequence, timeline, personal control, treatment control, and identity) and emotional representations (2 items; concern and emotion) of the illness and illness comprehensibility (1 item). All items are scored on a 1–10 linear point scale with higher scores indicating a negative perception [40]. The scale has shown good concurrent and predictive validity with a good ability to access changes over time [40].
Statistical analysis
The demographic, clinical, lifestyle, and psychosocial characteristics of the total population, norm population, and non-respondents were described using means and standard deviations (SD) for normally distributed and medians and interquartile ranges (IQR) for non-normally distributed continuous determinants. Data for categorical variables were presented as frequencies and percentages (presented in Table 4). The sample size that answered the EORTC QLQ-C30 sleep question (Q11) was used to match with the normative population. We matched the normative population with overall cancer survivors based on age and sex, after removing participants who have had cancer. Cancer survivors and normative population samples were grouped into a strata of gender (male, female) and age categories (≤ 45, > 45 to ≤ 50, > 50 to ≤ 55, > 55 to ≤ 60, > 60 to ≤ 65, > 65 to ≤ 70 and > 70), and matched per stratum according to the most limiting ratio of 1:13. This resulted in a sub sample of 415 age- and sex-matched participants from the normative population.
To answer the first research question on the prevalence of sleep problems, the proportion of participants (frequencies and percentage) having no, moderate, and many sleep problems was described for the cancer survivors and for the normative population, separately for the total cancer population and per cancer type (presented in Table 1).
To answer the second research question on the determinants of sleep problems, we first descriptively assessed differences in demographic, clinical, lifestyle, and psychosocial characteristics of survivors with no, moderate, and many sleep problems. Differences in these characteristics between sleep problem groups were assessed using analysis of variance (ANOVA) and Pearson chi square for continuous and categorical variables respectively (presented in Table 2).
Univariable analyses (N = 3979) were conducted to identify which determinants were associated with moderate and many sleep problems. Subsequently, in a hierarchical multinomial logistic regression, four nested models were analyzed including blocks of determinants that were significant in the univariable analyses (N = 3979). Multiple imputation was used to impute data on participants who had missing data on any of the determinants [41].This assured that the same patients were analyzed in each step of the hierarchical regression analysis. The underlying assumptions for a multinomial regression were checked and not violated. The following blocks were entered consecutively: demographic (age, sex, education, working, and marital status), clinical (BMI, cancer type, cancer stage, primary treatment, time since diagnosis, and number of comorbidities), lifestyle (smoking, alcohol, and physical activity), and psychosocial determinants (fatigue, anxiety and depression, and illness perception). The order in which the different blocks were entered in the hierarchical regression analysis was based on the fact that we first entered sociodemographic background variables, then the clinical background variables, then lifestyle (determinants that are modifiable), and ultimately, the psychosocial variables that are most closely related to the outcome and may thus be interpreted as an outcome cluster. These were entered as the final step because one would otherwise over-adjust. The results were reported as adjusted odds ratios (AOR) with 95% CI accompanied by McFadden’s pseudo R2 values for all models [42], to understand the explained variability and improvement from the null model to the fitted model (presented in Table 3). The descriptive and univariate multinomial logistic regression analyses were done using Statistical Analysis Software (SAS) version 9.4 and while the hierarchical logistic regression analyses were done using STATA version 17 since SAS did not report pseudo R2 for each model separately. Statistical significance was denoted by a p-value of ≤ 0.05 for two-sided tests.
Results
Study population
Of the 10,304 invited cancer survivors, 6917 responded (67%) of whom 6736 (65%) responded to the sleep question (Fig. 1). Based on these 6736 cancer survivors, a total of 415 normative individuals that matched on age and sex were extracted from the pool of 1557 individuals. The mean age of the normative population, cancer survivors who responded to the sleep question (respondents), and non-respondents was 66 years, while non-respondents were more often women (54%) compared to respondents (46%; Table 4). More than half of the respondents had secondary education (61%), were retired (78%), and were married (77%). The largest included cancer group was colorectal cancer (38%), and more than half of the respondents had surgery as their primary treatment (56%).
Prevalence of sleep problems compared to the normative population
The prevalence of sleep problems was higher in cancer survivors (17%, n = 1140) than in the normative population (11%, n = 46; Table 1) when matched based on all types of cancer survivors. When matched specifically based on each cancer type survivors of colorectal ovarian (highest), thyroid, Hodgkin’s lymphoma, non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, multiple myeloma, and basal/squamous cell carcinoma cancer survivors reported higher prevalence of sleep problems compared to the matched normative population. The prevalence of sleep problems did not differ in survivors being longer post diagnosis.
Determinants of sleep problems
The univariate analysis showed that demographic factors (sex, education, work, and having a partner), clinical factors (BMI, comorbidity), lifestyle factors (smoking, alcohol, and physical activity), and psychosocial factors (fatigue, anxiety, depressive symptoms, and illness perceptions) were associated with moderate and/or poor sleep (Table 2).
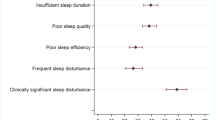
In the hierarchical regression, the full model (Table 3) showed that female cancer survivors (adjusted odds ratio (AOR) 2.26, 95% CI 2.06; 2.48) when compared to males, cancer survivors who had one comorbidity (AOR 1.25, 95% CI 1.10;1.41) and two or more comorbidities (AOR 2.15, 95% CI 1.92; 2.40) compared to cancer survivors with no comorbidity, cancer survivors who were former (AOR 1.30, 95% CI 1.18; 1.43), and current smokers (AOR 1.53, 95% CI 1.35;,1.75) compared to cancer survivors who never smoked, cancer survivors who were former alcohol drinkers (AOR 1.73, 95% CI 1.50; 1.99) compared to cancer survivors who did not drink alcohol, cancer survivors with fatigue (AOR 1.05, 95% CI 1.05; 1.06), anxiety (AOR 1.14, 95% CI 1.12; 1.16), depression (AOR 1.11, 95% CI 1.10; 1.13), and higher cognitive illness perception (AOR 1.02, 95% CI 1.02; 1.03) had a higher odds for sleep problems regardless of the included demographic factors. Whereas, cancer survivors with higher education (AOR 0.67, 95% CI 0.58; 0.76) compared to low education, cancer survivors having a partner (AOR 0.69, 95% CI 0.63; 0.75) compared to having no partner and cancer survivors who were obese (AOR 0.86, 95% CI 0.76; 0.97) compared to normal BMI showed to have a lower odds for sleep problems (Table 3). Working status and physical activity were not significantly associated with sleep problems when taking other covariables into account. However, in model 3 (with lifestyle determinants), cancer survivors with highest levels of physical activity compared to lowest levels of physical activity had a lower odds for sleep problems (AOR 0.91, 95% CI 0.83; 0.98). The full model showed a maximum change in R2 when compared to the previous models. This model showed a pseudo R2 of 0.21 compared to 0.05 for the starting model with only demographic determinants.
Discussion
In this study, we found that the proportion of survivors with sleep problems was higher in cancer survivors when compared to the normative population. The prevalence of survivors with sleep problems differed across cancer types, with the highest prevalence in ovarian cancer survivors. The literature suggests that ovarian cancer survivors may feel stressed due to the high recurrence rate in combination with non-specific alarming symptoms (bloated or uncomfortable feeling a the abdomen) which may cause higher distress and post diagnosis biological changes leading to sleep problems [23]. The prevalence of sleep problems among cancer survivors in our study was lower when compared to previous studies that focused on single cancer types [8, 9, 14]. To the best of our knowledge, our study is one of the few that compares the prevalence of sleep problems in cancer survivors of various types with an age- and sex-matched normative population. A lower prevalence of sleep problems in our study could be attributed to the absence of breast cancer survivors in our study population which is one of the most frequent and researched type of cancer with higher numbers of survivors with sleep problems [43,44,45].
We found several demographic factors such as female sex, lower education, and not having a partner, having a higher odds of experiencing sleep problems. These findings align with some previous studies, which also indicated phenomenon related to higher level of anxiety and fear of cancer progression in female cancer survivors associated with more sleep problems [1, 3, 6, 8, 15]. However, survivors with higher education and survivors who had a partner had a lower odds for sleep problems. These findings align with previous research attributing health literacy and engagement in interventions to improve sleep quality such as mind–body medicine among higher educated cancer survivors and the role of social support in patients with a partner on positive sleep outcomes [1, 15]. Additionally, we identified clinical factors BMI and presence of comorbidities as significant determinants of sleep problems. Consistent with the existing literature survivors with one or more comorbidities had a higher odds for sleep problems which may be attributed to various systemic complaints, symptoms, and drug interactions disturbing an uninterrupted sleep [3, 20]. In contrast to previous studies, we found no association between primary treatment and sleep problems [46]. Previous studies showed that cancer survivors who underwent chemotherapy as primary treatment had a higher odds for sleep problems [14, 17]. A reason that primary treatment was not associated with sleep problems in our study might be that other determinants which are strongly associated with sleep problems (e.g., psychosocial factors) confound the association between primary treatments and sleep problems. A second reason might be that treatment in a diverse cancer population might be heterogeneous. For instance, chemotherapy might include different agents and different regiments across cancer types. Furthermore, in our analyses, we could not adjust for sleep medication because these data were not available. Considering lifestyle factors and consistent with previous research, we found current smoking cancer survivors and both former smoking and former alcohol drinking cancer survivors to have a higher odds for sleep problems. Furthermore, cancer survivors who experienced fatigue were anxious and or depressive, and had threatening cognitive illness perception also had a higher odds for sleep problems which was similar to findings from previous studies that suggested hormonal imbalances following treatment, treatment side effects, and psychological distress contribute to sleep problems [9, 13, 15]. Psychological distress presenting as anxiety and or depression due to fear of death, recurrence, and poor prognosis may impact sleep quality [4, 8, 9, 21]. The psychosocial determinants, particularly fatigue, anxiety, depression, and illness perception contributed significantly to the variability in sleep quality among cancer survivors. Survivors with highest MVPA scores for physical activity had a lower odds for sleep problems compared to survivors with lowest MVPA scores before adjusting for psychosocial variables, which may be plausible as physical activity is also influencing for instance, anxiety, fatigue, depression, and illness perception.
The pseudo-R2 was very small indicating that there are more or more important determinants of sleep problems for which we have no data and thus could not include in the model (e.g., sleep medication).
There were several strengths of this study. First, the large sample size, that included various types of cancers and determinants, gave us enough statistical power to investigate differences across cancer types. Second, the inclusion of an age- and sex-matched normative population as a comparison group allowed for a fair comparison between each cancer type and the normative population. Third, a notable strength was the use of registry-based diagnosis ensuring verified, up to date and accurate clinical data. Few previous studies have employed such robust data collection methods on clinical variables.
However, there were also certain limitations to our study. First, the cross-sectional design does not allow drawing conclusions on the causality between sleep problems, fatigue, anxiety, depression, and illness perception—significant determinants in the final model. We cannot assert that higher fatigue, anxiety, and/or depression causes sleep problems, as the reverse relation could also be the case. Moreover, these symptoms are known to cluster and might be interrelated in a more complex manner than can be identified even with longitudinal data. Second, we did not have data of survivors of all cancer types (e.g., no lung and breast cancer), various domains of sleep quality, and the use of sleep medication among cancer survivors. This might have attenuated the current prevalence and point estimates of sleep problems when compared to good sleepers. Studies have shown a prevalence of sleep problems of up to 56% in lung cancer survivors and 38% in breast cancer survivors [43, 47]. The absence of these cancer types in our analysis might explain the lower overall prevalence of sleep problems in the present study. Additionally, since no data about sleep medication was available, it is possible that cancer survivors with sleep problems using sleep medication reported not experiencing trouble sleeping. Another limitation might be that the data were collected between May 2008 and April 2015. However, the problem of sleep problems after cancer is still as prevalent today as it was then. As the included determinants of sleep problems are largely unrelated to changes in healthcare and treatment, we believe that the results of our study is still of great value to this field of research. Furthermore, we used the sleep quality scale of the EORTC QLQ-C30, a scale only consisting of a single-item. Although a single-item measure in calculating prevalence estimates likely limits the accuracy, earlier studies showed that the sleep item of the EORTC QLQ-C30 was highly correlated (r = 0.71) with the total score of the Pittsburgh Sleep Quality Index (PSQI), a multiple-item questionnaire [33, 34]. We also used a unidimensional measure of fatigue that may have led to an underestimation of the prevalence of fatigue, which may dilute the effect size. Moreover, it hampers the ability to assess the impact of different dimensions of fatigue. Lastly, the reliance on self-reported data could have potentially biased the estimates of certain determinants. We attempted to overcome over- and underestimation by categorizing physical activity and BMI.
The clinical implications of this study suggest that early screening for sleep problems by healthcare professionals in clinical settings is warranted. Patients can be supported by focusing on improving various modifiable lifestyle factors after cancer treatment that might help to prevent or diminish sleep problems. These factors include increasing physical activity and decreasing smoking and alcohol consumption. As fatigue, depression, and illness perception seems related, it might be possible that increasing physical activity also has a positive effect on these psychological factors besides sleep problems. Patients can be referred to interventions that address psychological factors such as cognitive behavioral therapies, Mindfulness-Based Stress Reduction Programs, or yoga [4, 11, 48, 49]. Research implications include future prospective cohort studies with other cancer types, exploring domains of sleep quality and investigating the effects of the interventions that address sleep problems.
In conclusion, cancer survivors exhibit a higher prevalence of sleep problems compared to a normative population, with the highest prevalence in ovarian cancer survivors. Female cancer survivors, cancer survivors who do not have higher education, cancer survivors without a partner, with comorbidities, former and current smokers, former alcohol drinkers, cancer survivors having low physical activity levels, high fatigue levels, elevated anxiety, depression, and cognitive illness perception levels were more prone to have sleep problems. Notably, psychosocial determinants add to the variability in sleep problems of cancer survivors. Health care professionals need to be aware of the high prevalence of sleep problems in cancer survivors and should pay attention to these problems during follow-up visits even years after diagnosis.
Data availability
After publication, de-identified individual participant data and syntax files will be shared upon request, for scientific purposes, after approval of the proposal, with a signed data access agreement and with investigator support. Contact information can be found at the PROFILES registry webpage: https://www.profilesregistry.nl/contact/.
References
Voiss P, Höxtermann MD, Dobos G, Cramer H. Cancer, sleep problems, and mind-body medicine use: results of the 2017 National Health Interview Survey. Cancer. 2019;125:4490–7. https://doi.org/10.1002/cncr.32469.
Daniel LC, Aggarwal R, Schwartz LA. Sleep in adolescents and young adults in the year after cancer treatment. J Adolesc Young Adult Oncol. 2017;6:560–7. https://doi.org/10.1089/jayao.2017.0006.
Hammersen F, Lewin P, Gebauer J, Kreitschmann-Andermahr I, Brabant G, Katalinic A, et al. Sleep quality and health-related quality of life among long-term survivors of (non-) Hodgkin lymphoma in Germany. PLoS ONE. 2017;12: e0187673. https://doi.org/10.1371/journal.pone.0187673.
Fiorentino L, Ancoli-Israel S. Sleep dysfunction in patients with cancer. Curr Treat Options Neurol. 2007;9:337–46.
Nock NL, Dimitropoulos A, Zanotti KM, Waggoner S, Nagel C, Golubic M, et al. Sleep, quality of life and depression in endometrial cancer survivors with obesity seeking weight loss. Support Care Cancer. 2020;28:2311–9. https://doi.org/10.1007/s00520-019-05051-1.
Fleming L, Gillespie S, Espie CA. The development and impact of insomnia on cancer survivors: a qualitative analysis. Psychooncology. 2010;19:991–6. https://doi.org/10.1002/pon.1652.
Clanton NR, Klosky JL, Li C, Jain N, Srivastava DK, Mulrooney D, et al. Fatigue, vitality, sleep and neurocognitive functioning in adult survivors of childhood cancer: a report from the childhood cancer survivor study. Cancer. 2011;117:2559–68. https://doi.org/10.1002/cncr.25797.
Strollo SE, Fallon EA, Gapstur SM, Smith TG. Cancer-related problems, sleep quality, and sleep disturbance among long-term cancer survivors at 9-years post diagnosis. Sleep Med. 2020;65:177–85. https://doi.org/10.1016/j.sleep.2019.10.008.
Humpel N, Iverson DC. Sleep quality, fatigue and physical activity following a cancer diagnosis. Eur J Cancer Care. 2010;19:761–8. https://doi.org/10.1111/j.1365-2354.2009.01126.x.
Chan J, Ng DWL, Liao Q, Fielding R, Soong I, Chan KKL, et al. Trajectories of sleep disturbance in cancer survivors during the first 2 years post-treatment. Sleep 2023;46:zsad052. https://doi.org/10.1093/sleep/zsad052.
Al Maqbali M, Al Sinani M, Alsayed A, Gleason AM. Prevalence of sleep disturbance in patients with cancer: a systematic review and meta-analysis. Clin Nurs Res. 2022;31:1107–23. https://doi.org/10.1177/10547738221092146.
Hofmeister D, Schulte T, Mehnert-Theuerkauf A, Geue K, Zenger M, Esser P, et al. The association between sleep problems and general quality of life in cancer patients and in the general population. Front Psychol. 2022;13: 960029. https://doi.org/10.3389/fpsyg.2022.960029.
Legg M, Meertens RM, van Roekel E, Breukink SO, Janssen ML, Keulen ETP, et al. The association between sleep quality and fatigue in colorectal cancer survivors up until two years after treatment: a cross-sectional and longitudinal analysis. Cancers (Basel). 2022;14:1527. https://doi.org/10.3390/cancers14061527.
Tuyan İlhan T, Uçar MG, Gül A, Saymaz İlhan T, Yavaş G, Çelik Ç. Sleep quality of endometrial cancer survivors and the effect of treatments. Turk J Obstet Gynecol. 2017;14:243–8. https://doi.org/10.4274/tjod.59265.
Webber K, Carolus E, Mileshkin L, Sommeijer D, McAlpine J, Bladgen S, et al. OVQUEST – life after the diagnosis and treatment of ovarian cancer - an international survey of symptoms and concerns in ovarian cancer survivors. Gynecol Oncol. 2019;155:126–34. https://doi.org/10.1016/j.ygyno.2019.08.009.
Goswami S, Mongelli M, J Peipert B, Helenowski I, Yount SE, Sturgeon C. Benchmarking health-related quality of life in thyroid cancer versus other cancers and United States normative data. Surgery 2018;164:986–92. https://doi.org/10.1016/j.surg.2018.06.042.
Daniel LC, Wang M, Mulrooney DA, Srivastava D, Schwartz LA, Edelstein K, et al. Sleep, emotional distress, and physical health in survivors of childhood cancer: a report from the childhood cancer survivor study. Psychooncology. 2019;28:903–12. https://doi.org/10.1002/pon.5040.
van Walree IC, Hamaker ME, van de Poll-Franse LV, Vos MC, Boll D, van Huis-Tanja LH, et al. Older ovarian cancer survivors report lower long-term health-related quality of life than younger survivors: a study from the population-based profiles registry. Gynecol Oncol. 2019;153:391–8. https://doi.org/10.1016/j.ygyno.2019.02.001.
Zhao C, Grubbs A, Barber EL. Sleep and gynecological cancer outcomes: opportunities to improve quality of life and survival. International Journal of Gynecologic Cancer 2022;32. https://doi.org/10.1136/ijgc-2022-003404.
Aronsen S, Conway R, Lally P, Roberts A, Croker H, Beeken RJ, et al. Determinants of sleep quality in 5835 individuals living with and beyond breast, prostate, and colorectal cancer: a cross-sectional survey. J Cancer Surviv. 2022;16:1489–501. https://doi.org/10.1007/s11764-021-01127-2.
Abebe E, Giru BW, Boka A. Sleep quality and associated factors among adult cancer patients on treatments at Tikur Anbessa Specialized Hospital Oncology Unit, Addis Ababa, Ethiopia, 2021. Cancer Control. 2023;30:10732748231160128. https://doi.org/10.1177/10732748231160129.
Rodriguez-Gonzalez A, Velasco-Durantez V, Martin-Abreu C, Cruz-Castellanos P, Hernandez R, Gil-Raga M, et al. Fatigue, emotional distress, and illness uncertainty in patients with metastatic cancer: results from the Prospective NEOETIC_SEOM study. Curr Oncol. 2022;29:9722–32. https://doi.org/10.3390/curroncol29120763.
Clevenger L, Schrepf A, DeGeest K, Bender D, Goodheart M, Ahmed A, et al. Sleep disturbance, distress, and quality of life in ovarian cancer patients during the first year after diagnosis. Cancer. 2013;119:3234–41. https://doi.org/10.1002/cncr.28188.
Jabbarian LJ, Rietjens JAC, Mols F, Oude Groeniger J, van der Heide A, Korfage IJ. Untangling the relationship between negative illness perceptions and worse quality of life in patients with advanced cancer—a study from the population-based PROFILES registry. Support Care Cancer. 2021;29:6411–9. https://doi.org/10.1007/s00520-021-06179-9.
Schoormans D, Jansen M, Mols F, Oerlemans S. Negative illness perceptions are related to more fatigue among haematological cancer survivors: a PROFILES study. Acta Oncol. 2020;59:959–66. https://doi.org/10.1080/0284186X.2020.1759823.
Schoormans D, Wijnberg L, Haak H, Husson O, Mols F. Negative illness perceptions are related to poorer health-related quality of life among thyroid cancer survivors: results from the PROFILES registry. Head Neck. 2020;42:2533–41. https://doi.org/10.1002/hed.26290.
van de Poll-Franse LV, Horevoorts N, van Eenbergen M, Denollet J, Roukema JA, Aaronson NK, et al. The Patient Reported Outcomes Following Initial treatment and Long term Evaluation of Survivorship registry: scope, rationale and design of an infrastructure for the study of physical and psychosocial outcomes in cancer survivorship cohorts. Eur J Cancer. 2011;47:2188–94. https://doi.org/10.1016/j.ejca.2011.04.034.
de Rooij BH, Ezendam NPM, Mols F, Vissers PAJ, Thong MSY, Vlooswijk CCP, et al. Cancer survivors not participating in observational patient-reported outcome studies have a lower survival compared to participants: the population-based PROFILES registry. Qual Life Res. 2018;27:3313–24. https://doi.org/10.1007/s11136-018-1979-0.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76. https://doi.org/10.1093/jnci/85.5.365.
Giesinger JM, Loth FLC, Aaronson NK, Arraras JI, Caocci G, Efficace F, et al. Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research. J Clin Epidemiol. 2020;118:1–8. https://doi.org/10.1016/j.jclinepi.2019.10.003.
Fayers PM, Aaronson N, Bjordal K, Groenvold M, Curran D, Bottomley A, et al. EORTC QLQ-C30 scoring manual: this manual is intended to assist users with scoring procedures for the QLQ-C30 version 3 and earlier, and the QLQ supplementary modules. Brussels: EORTC; 2001.
Groenvold M, Klee MC, Sprangers MAG, Aaronson NK. Validation of the EORTC QLQ-C30 quality of life questionnaire through combined qualitative and quantitative assessment of patient-observer agreement. J Clin Epidemiol. 1997;50:441–50. https://doi.org/10.1016/S0895-4356(96)00428-3.
de Winter J, Ezendam NPM, Bours MJL, Winkels RM, Weijenberg MP, Kampman E, et al. Is sleep associated with BMI, waist circumference, and diet among long-term colorectal cancer survivors? Results from the population-based PROFILES registry. Support Care Cancer. 2021. https://doi.org/10.1007/s00520-021-06393-5.
Hofmeister D, Schulte T, Hinz A. Sleep problems in cancer patients: a comparison between the Jenkins Sleep Scale and the single-item sleep scale of the EORTC QLQ-C30. Sleep Med. 2020;71:59–65. https://doi.org/10.1016/j.sleep.2019.12.033.
MVPA for Good Health | ActiGraph n.d. https://actigraphcorp.com/newsletters/mvpa-for-good-health/ (accessed July 26, 2021).
Fatigue Assessment Scale n.d. https://www.wasog.org/educational-material/fatigue-assessment-scale.html (accessed July 27, 2021).
Michielsen HJ, De Vries J, Van Heck GL, Van de Vijver FJR, Sijtsma K. Examination of the dimensionality of fatigue: the construction of the Fatigue Assessment Scale (FAS). Eur J Psychol Assess. 2004;20:39–48. https://doi.org/10.1027/1015-5759.20.1.39.
Stern AF. The Hospital Anxiety and Depression Scale. Occup Med. 2014;64:393–4. https://doi.org/10.1093/occmed/kqu024.
Ibbotson T, Maguire P, Selby P, Priestman T, Wallace L. Screening for anxiety and depression in cancer patients: the effects of disease and treatment. Eur J Cancer. 1994;30:37–40. https://doi.org/10.1016/S0959-8049(05)80015-2.
Thong MSY, Kaptein AA, Vissers PAJ, Vreugdenhil G, van de Poll-Franse LV. Illness perceptions are associated with mortality among 1552 colorectal cancer survivors: a study from the population-based PROFILES registry. J Cancer Surviv. 2016;10:898–905. https://doi.org/10.1007/s11764-016-0536-5.
Kang H. The prevention and handling of the missing data. Korean J Anesthesiol. 2013;64:402–6. https://doi.org/10.4097/kjae.2013.64.5.402.
FAQ: what are pseudo R-squareds? n.d. https://stats.oarc.ucla.edu/other/mult-pkg/faq/general/faq-what-are-pseudo-r-squareds/ (accessed August 3, 2022).
Lowery-Allison AE, Passik SD, Cribbet MR, Reinsel RA, O’Sullivan B, Norton L, et al. Sleep problems in breast cancer survivors 1–10 years posttreatment. Palliat Support Care. 2018;16:325–34. https://doi.org/10.1017/S1478951517000311.
Quality of life in “chronic” cancer survivors: a meta-analysis | SpringerLink n.d. https://link-springer-com.ezproxy.ub.unimaas.nl/article/https://doi.org/10.1007/s11764-020-00869-9 (accessed July 12, 2021).
Mols F, Vingerhoets AJJM, Coebergh JW, van de Poll-Franse LV. Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer. 2005;41:2613–9. https://doi.org/10.1016/j.ejca.2005.05.017.
Wang J, Zhou B-Y, Lian C-L, Zhou P, Lin H-J, Wu S-G. Evaluation of subjective sleep disturbances in cancer patients: a cross-sectional study in a radiotherapy department. Frontiers in Psychiatry 2021;12.
Gooneratne NS, Dean GE, Rogers AE, Nkwuo JE, Coyne JC, Kaiser LR. Sleep and quality of life in long-term lung cancer survivors. Lung Cancer. 2007;58:403–10. https://doi.org/10.1016/j.lungcan.2007.07.011.
Lin P-J, Kleckner IR, Loh KP, Inglis JE, Peppone LJ, Janelsins MC, et al. Influence of yoga on cancer-related fatigue and on mediational relationships between changes in sleep and cancer-related fatigue: a nationwide, multicenter randomized controlled trial of yoga in cancer survivors. Integr Cancer Ther. 2019;18:1534735419855134. https://doi.org/10.1177/1534735419855134.
Garland SN, Xie SX, DuHamel K, Bao T, Li Q, Barg FK, et al. Acupuncture versus cognitive behavioral therapy for insomnia in cancer survivors: a randomized clinical trial. J Natl Cancer Inst. 2019;111:1323–31. https://doi.org/10.1093/jnci/djz050.
Acknowledgements
The authors thank the registration teams of the Netherlands Comprehensive Cancer Organisation for the collection of data for the Netherlands Cancer Registry and members of the PROFILES registry for the collection of the patient-reported outcomes data. We are very grateful for the participation of all patients and doctors in the study.
Funding
The studies were funded via an investment grant from the Dutch Research Council (NWO) (480–08-009) and a VENI grant from the Dutch Research Council (NWO) (451–10–041).
Author information
Authors and Affiliations
Contributions
Charles David: data analysis, writing and editing.
Dr. Sandra Beijer: conceptualization data analysis, review, and editing.
Dr. Floortje Mols: data collection, data cleaning, review, and editing.
Dr. Simone Oerlemans: data collection, data cleaning, review, and editing.
Dr. Olga Husson: data collection, data cleaning, review, and editing.
Prof. Dr. Matty Weijenberg: review and editing.
Dr. Nicole Ezendam: conceptualization, data collection, data cleaning, data analysis, review, and editing.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval was obtained for all cohorts separately from a local certified medical ethics committee. This study was performed in accordance with the principles of the Declaration of Helsinki and the Medical Research Involving Human Subjects Act (WMO). The data were protected following the GDPR law.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
David, C., Beijer, S., Mols, F. et al. Prevalence and determinants of sleep problems in cancer survivors compared to a normative population: a PROFILES registry study. J Cancer Surviv (2024). https://doi.org/10.1007/s11764-024-01641-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-024-01641-z