Abstract
Purpose
This study aims to investigate changes in employment status among disease-free working-age cancer survivors (CSs) with late effects from diagnosis to their first meeting in the Late Effects Clinic (LEC) and investigate associated patient-reported outcomes of reduced employment status.
Methods
Retrospective analysis of a cohort of CSs followed in a LEC at a single institution from January, 2022, to March, 2023. Working-age CSs with no current evidence of active cancer were included in this study. CSs completed a baseline questionnaire (EORTC QLQ-SURV100) before their initial consultation. Reduced employment status was defined as transition from being in paid work at diagnosis to working fewer hours or not at all at the first visit. Multivariate linear regression analysis was used.
Results
A total of 119 CSs with diverse cancer types with a mean age of 51 years (range 26 to 70) were included in this study. Eighty percent were female. Of 93 CSs in paid work at diagnosis, 66 (71%) have reduced employment status. Reduced employment status was associated with lower role functioning score (β = −12.3, p = 0.046), higher loss of income score (β = 35.1, p = 0.001), and lower Global health status score (β = − 8.3, p = 0.05).
Conclusions
This study shows that the majority of CSs seen in the LEC have reduced employment status. This is associated with impaired quality of life.
Implications for cancer survivors
Identifying and treating late effects early in cancer survivorship are important to secure CSs’ labour market attachment and, thus, their financial and social well-being.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Due to early detection and improved treatment, the number of cancer survivors (CSs) has been increasing [1]. More than 370,000 (6%) Danes live with or have had cancer. About 60% of these people are of working age [2], and up to 50% of CSs experience late effects such as fatigue, cognitive impairment, sleep problems, and pain [3, 4]. These can affect the CS’s ability to return to their job to the same extent as before their diagnosis. Based on our clinical experience, many CSs are eager to return to work but experience that they have to make adjustments at work; they are not able to work the same hours and/or perform the same work tasks as before the diagnosis. Beyond the financial considerations, being part of the workforce is important for CSs’ psychological and social well-being because of its links to personal identity, self-esteem, life purpose, and social relationships [5]. Hence, there is a growing interest in patient-reported outcome (PRO) data to evaluate CSs’ health-related quality of life (HRQOL). HRQOL covers the subjective perceptions of the positive and negative aspects of CSs’ symptoms, including physical, emotional, social, and cognitive functions and, importantly, disease symptoms and side effects of treatment [6]. The European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group has developed an HRQOL assessment strategy that captures the full range of issues relevant to disease-free CSs resulting in the EORTC Quality of Life Cancer Survivorship Core Questionnaire (QLQ-SURV100) [7]. As the EORTC QLQ-SURV100 is a newly developed questionnaire, there is no published data yet available.
In January, 2021, the Region of Southern Denmark decided to establish four Late Effects Clinics (LECs). Primo 2022, the LEC of Odense University Hospital, Denmark, opened. The clinic’s purpose is to offer interdisciplinary help to CSs experiencing severe late effects with unmet needs within the existing framework.
Although many studies have investigated employment status and return to work in CSs, to the best of our knowledge, none has investigated the change in employment among CSs with complex late effects with unmet needs [8,9,10]. de Moor et al. suggest further research among understudied groups, underlining the relevancy of this study [8].
The main aim of this study was to investigate changes in employment status among disease-free working-age CSs with late effects and unmet needs from diagnosis to their first meeting in the LEC between January, 2022, and March, 2023. A secondary aim is to investigate the association between change in employment status and PRO-data (role functioning score, work score, loss of income score, and global health status score) measured by the EORTC QLQ-SURV100.
Methods
Study setting
The database containing data from all CSs seen in the LEC of Odense University Hospital, Denmark, between January, 2022, and March, 2023, was reviewed. Disease-free CSs with complex late effects after cancer treatment can be referred by their general practitioner or hospital departments, when beyond active treatment. Hence, they constitute only a small proportion of the population of CSs. CSs were requested to complete the Danish version of the EORTC QLQ-SURV100 at their first consultation in the LEC. The patient reporting is used as a dialogue tool in the clinical encounter. Based on this consultation, further investigations, referral to other relevant departments, or rehabilitation in the municipalities are initiated. The LEC also offers group-based interventions, individual nurse counselling, or psychological therapy. Informed written consent was obtained from all participants before completing the questionnaire.
Population
The exclusion criteria were (1) being retired at the first visit, (2) the latest evaluation was with relapse or new cancer, or (3) death. One hundred nineteen survivors attending the LEC were considered eligible.
Main outcome variables
The main outcome was change in employment status from diagnosis to the first visit to the LEC. CSs reported their employment status at their first meeting, and information on their employment status at diagnosis and up to 1 year prior was collected from a chart audit. Employment status was categorised as paid work (full-time job, part-time job, flex job) and unemployed (disability pension, early retirement, and others (job training, jobseeker, sick leave, education, and unemployed without unemployment benefits)). Among CSs in paid work at diagnosis, change in employment status from diagnosis to the first visit was further explored. Change in employment status was dichotomised into reduced employment status (transition to fewer hours or not working at all) and maintained employment status (same employment status as before).
Sociodemographic data, such as gender (female/male), age at the first visit, cohabitation status (living with partner yes/no), children under 18 years (yes/no), and educational attainment (primary education, upper secondary/ vocational education, or higher (vocational)/university education) were obtained by specialists in the LEC at the first visit. Health-related variables, including cancer site, age at diagnosis, years since primary diagnosis, treatment modalities, years since primary treatment, and comorbidity (yes/no), were extracted from the medical records. Late effects were assessed by specialists within the field of late effects after cancer and its treatment at the first visit to the LEC. In a Danish context, late effects are defined as health problems that occur during treatment and become chronic or develop months or years after treatment has ended [11].
Tools and measures
The EORTC QLQ-SURV100 is based on the reliable and valid EORTC Quality of Life Core Questionnaire (QLQ-C30). The QLQ-SURV100 is a newly developed and partly validated questionnaire for disease-free CSs and is currently undergoing further validation [7]. The QLQ-SURV100 consists of 100 items, including a global health status/quality of life scale, thirteen functional scales, nine symptom scales, one symptom checklist assessing chronic side effects of cancer treatments, and twelve single items. This study focused on the scales and items of role functioning, work, loss of income, and global health status. The questions in the four scales and items are added in Supplementary File 1. The QLQ-SURV100 questions are rated on a scale from 1 (not at all) to 4 (very much). Except for the global health status items, where a scale from 1 (very poor) to 7 (excellent) is used. The time frame of the questions is “during the past week” for role functioning and global health status. For work and loss of income, the time frame is “since the diagnosis and treatment of your cancer.” The scoring approach for the QLQ-SURV100 is identical in principle for the QLQ-C30. The CSs’ responses are transformed into a standard score according to the official EORTC scoring manual. Missing items were handled as outlined in the scoring manual [12]. The score ranges from 0 to 100, with a higher score for a functional scale indicating a high level of functioning, a higher score for the global health status indicating a high quality of life, but a higher score for a symptom scale indicating a higher level of symptomatic problems.
Study data were extracted from the electronic medical records and double entered into the secure REDCap (Research Electronic Data Capture) [13, 14].
Statistical analysis
Descriptive statistics were used to summarise the sociodemographic and clinical characteristics of the participants. Univariate analyses including chi-square test, two-sample Wilcoxon rank-sum (Mann–Whitney) test, and two-sample t-test were performed to determine any differences in the population characteristics and the standard score of the four domains between the two groups maintained and reduced employment status. For the standard score of the four domains, multivariate linear regression models with the independent variables employment status, gender, cohabitation status, educational attainment, and fatigue were used. One-sample z-test was used to determine if the PRO-data scores differed from the nominative data from the Danish population and EORTC QLQ-C30 reference values [15, 16]. Differences were considered significant if the p-value was equal to or less than 0.05. Statistical analysis of the data was performed using STATA 17.
Results
Sociodemographic and clinical characteristics
One hundred sixty-five CSs were seen in the LEC between January, 2022, and March, 2023. Of the 165 CSs, 41 were excluded due to retirement, four due to relapse, and one because of death. The response rate of the QLQ-SURV was 99%. The mean age at first visit was 51 years (range 26 to 70). Sixty-five percent of the CSs had higher (vocational) or university education. The mean age at diagnosis was 46.5 years (range 19 to 65), and the mean time since primary diagnosis was 4.3 years (range 0 to 31). The full sample sociodemographic and clinical characteristics are presented in Table 1. No statistically significant differences in population characteristics were observed.
Employment status
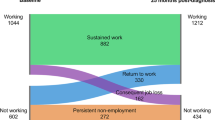
Among 119 CSs, 93 (78%) were in paid work at diagnosis and 26 (22%) were unemployed, including 11 (9%) receiving disability pension and 15 (13%) having other job statuses. At the first visit, 56 (47%) were in paid work and 63 (53%) were unemployed, including 21 (18%) receiving disability pension. The proportion of employment status at diagnosis and first visit to the LEC is shown in Fig. 1. Of 93 CSs in paid work at diagnosis, 27 (29%) have maintained employment status and 66 (71%) have reduced employment status. Among the 26 unemployed CSs at diagnosis, four (3%) had a negative change in employment status from other to disability pension. Seven (6%) of the CSs having other job statuses at diagnosis maintained this status. All the CSs receiving disability pension at diagnosis still held disability pension at the first visit. Four (3%) had a positive change in employment status from other to paid work, two got full-time jobs and two got part-time jobs.
The proportion of employment at diagnosis and first visit among 119 cancer survivors at working age from a Late Effects Clinic in Denmark from January, 2022, to March, 2023. Blue indicates paid work. Orange indicates unemployed. Other include job training, job seeker, sick leave, education, and unemployed without unemployment benefits
Patient-reported outcomes
In the bivariate analysis, those who had reduced employment status reported a lower role functioning score than CSs with maintained employment status (52.5 vs. 66.7, p = 0.012) and a higher loss of income score (55.9 vs. 4, p < 0.001) (Table 2). There was no significant difference in the work score or global health status score (Table 2).
In multivariate analysis, controlling for gender, cohabitation status, educational attainment, and fatigue, statistically significant effects between the groups (maintained vs. reduced employment status) were seen for role functioning score (β = −12.3, p = 0.046), loss of income score (β = 35.1, p = 0.001), and global health status score (β = − 8.3, p = 0.05). Fatigue was statistically significantly associated with lower role functioning score (β = 14.9, p = 0.021) and higher loss of income score (β = 21.4, p = 0.04). PRO-data associated with changes in employment status in multivariate analyses are shown in Table 3.
Compared to normative data from the general Danish population, the mean role functioning scores and the global health status scores for both those with maintained employment status (p < 0.001) and those with reduced employment status (p < 0.001) are significantly lower [15]. However, comparing the mean role functioning scores and the global health status scores with EORTC QLQ-C30 reference values, only those with reduced employment status have significantly lower scores (p < 0.001) [16].
Discussion
In this study, the majority of CSs within working age seen in the LEC had reduced employment status from diagnosis to the first visit (71%). Only 29% had maintained employment status. We found that reduced employment status was associated with a lower role functioning score, higher loss of income score, and lower global health status score. There was no significant difference in the work score.
Employment status
In this study, 78% were in paid work at diagnosis and 9% held disability pension, which corresponds well with the employment rate in the region of Southern Denmark aged 16–64. The general population’s average employment rate was 73% between 2008 and 2021 (range 70 to 77%, highest in 2021), and 7% received disability pension in 2021 [17, 18]. On the first visit to the LEC, 47% were in paid work and 18% held disability pension. Therefore, this study’s findings indicate that CSs with late effects and unmet needs have a higher risk of unemployment and disability pension than the general population.
A systematic review of 28 studies reported data about employment or return to work rates in cancer survivorship. Overall, on average, 63.5% of the participants (range 24–94%) managed to return to work depending on the period after cancer treatment [19].
Although these findings are not directly comparable due to different populations and healthcare systems, they all show that the majority of CSs maintain their employment status after their diagnosis and treatment. This is not in alignment with our findings. However, it may be argued that CSs referred to the LEC may be more affected by the number and complexity of their late effects than the average CS.
Patient-reported outcomes
In this study, the mean role functioning score and global health status score for those with maintained employment status and for those with reduced employment status were significantly lower than in the general Danish population [15]. This indicates that the CSs seen in the LEC, regardless of employment status, perform worse and have a lower quality of life than individuals without a history of cancer. This is in line with findings from other studies [20, 21]. Compared with EORTC QLQ-C30 reference values for cancer patients, the scores found in this study are significantly lower than the mean role functioning score and global health status score for the CSs with reduced employment, but not for those with maintained employment [16], indicating that CSs with maintained employment status are more like the average cancer patient. However, reduced employment is correlated to limited role functioning and lower quality of life. This is consistent with the findings from a Dutch study, where CSs employed 5 years post-diagnosis had better quality-of-life outcomes compared to those not being employed [9]. Furthermore, in multivariate analysis, we found a significantly lower role functioning score for those with reduced employment status. This suggests that limited role functioning affects the CSs’ ability to return to their job to the same extent as before their diagnosis. This association is in accordance with a Danish study that found that the negative effect of cancer on employment is stronger if the pre-cancer occupation requires high levels of manual skills [22]. In this study, CSs are to a large extent affected by psychological late effects such as fatigue, cognitive impairment, and fear of recurrence. We found that fatigue was statistically significantly associated with lower role functioning score. This is consistent with prior findings [10, 21]. Furthermore, a large proportion of the CSs from the clinic are highly educated. This suggests that there may be a mismatch between individual capabilities and skill demands in the occupation after cancer, which could lead to unemployment. This could be due to late effects. Many CSs are not ready to join the labour market after treatment completion, and the pressure to do so may sustain or worsen the late effects and their ability to work. However, for others, work can have important psychosocial benefits by providing a sense of purpose, creating social connections, and a potential distraction from cancer-related concerns and thereby better management of their late effects.
To fully understand the association between late effects and reduced employment, further research is recommended to collect PRO-data and data on employment status at baseline and regularly with a long follow-up period. Furthermore, prospective studies are needed to assess whether reducing symptoms and improving functioning can improve the workability of CSs. More research is needed to investigate the follow-up data from the LEC.
The findings of this study suggest the need for policies promoting opportunities for more flexible adjustment to jobs where the requirements match the CSs’ abilities. Finally, an unresolved job situation may unnecessarily increase the CSs’ mental workload and cause economic instability.
In this study, CSs with reduced employment status reported a significantly higher loss of income score than CSs who maintained employment. Even though this is not surprising, the result demonstrates the importance of helping survivors back in the labour market, as loss of income has a negative impact on both an individual and societal level. Even in countries with universal health care, there can be additional patient-covered costs of appointments with specialists, medicines, and medical devices [23]. Reduced employment status and loss of income reduce the financial reserves required to meet the direct and indirect medical costs. In addition, CSs may reduce spending on these costs to limit the financial burden, which could result in poorer outcomes regarding late effects, thereby reducing workability.
There is no significant difference in the work score, which could be due to a lack of statistical power in the study.
There is no normative data for the work and loss of income scores, as they were not part of the EORTC QLQ-C30. As the EORTC QLQ-SURV100 is a newly developed questionnaire, there is no published data yet available. We expect more data to be published in the future, both nationally and internationally.
Strengths and limitations
This study is unique as it is the first from the novel LEC in the region of Southern Denmark. A major strength of this study is the use of real-world data including PRO instruments specifically developed for disease-free CSs, in combination with data from medical records. The medical records for each patient were thoroughly assessed and data was double entered. Furthermore, we had a response rate of 99%, which is extremely high. The high response rate may be due to the fact that the questionnaire was used as a dialogue tool in the clinic, which was motivational for the CSs. Moreover, the questionnaire was completed in connection with the first visit. Accordingly, clinicians were able to encourage completion. All eligible CSs accepted to participate in the study. Another strength of this study is the population of CSs with complex late effects with unmet needs, as employment status has not yet been investigated among this subgroup of CSs. However, this can also be considered a limitation, as the results are not representative of all CSs.
The small sample size is also a limitation. Hence, further studies with larger samples are needed to confirm our findings. Moreover, 80% of the CSs were female, and the results may not be generalisable to men. Previous studies show that women are more likely to seek healthcare, which could explain our results [24, 25]. In this study, over 50% of the included study participants were female breast cancer survivors. Yet, it is estimated in 2021 that 21% of CSs between 15 and 74 years have a history of breast cancer [2]. This demonstrates that this study’s makeup of cancer types is inconsistent with those in long-term cancer survivorship. In this study, 65% of the CSs had a higher education. In addition to gender differences, there is also reported educational differences in the use of health services, indicating social inequality [26, 27]. Compared to CSs with higher education, a greater proportion of CSs with short education are affected by high levels of symptoms and impaired functioning [28]. Therefore, we believe our results may apply to CSs in all educational groups and it underlines the need for this patient group to be referred to a LEC.
The results of this study reflect the Danish welfare model and the unique structures of the health care system, employment law, and culture. As Denmark has a well-developed, tax-financed welfare system, all Danish citizens have equal access to health care and are entitled to limited compensation for loss of income due to unemployment, disability, or illness. Hence, our results may not be generalisable to countries with different welfare systems.
Implications for clinical practice
In the consultation with the survivors in the clinic, clinicians routinely discuss survivors’ employment status and their ability to work. They explore the physical and cognitive effects of cancer or its treatment, which may limit the survivor’s ability to work. If needed, the LEC assisted by the oncology social workers collaborate with the municipalities to create an individually adapted plan for returning to work at an appropriate pace.
Traditionally, the workplace and the municipal job centre are key actors in helping CSs return to work in Denmark. The role of the job centre is to assist job seekers in their job search, including aiming to reduce reimbursement costs when possible. People who receive unemployment benefits must attend the job centre, and cancer patients may feel pressured to return to the labour market before they are ready [29]. Thus, there is a need for programs tailored to CSs’ circumstances. If the state of health and course of treatment are not considered in cross-sector collaboration, the employment effort may become counterproductive. Therefore, healthcare professionals must identify the CSs’ needs through systematic assessment early in cancer survivorship care, and if possible help remedy late effects or refer the CSs to specialists who can inform them about the existing challenges, opportunities, and offers [4]. Additionally, clinicians should encourage discussion with CSs and their employer to understand workplace options and modifications to their previous role potentially with the help of social workers [4]. Moreover, there is a need to increase referrals for males and CSs with lower education, reducing gender and social inequality. To address this inequality, there is a need to identify CSs with unmet needs, especially among those with few health skills and few resources, through systematic screening of impaired functioning during cancer follow-up [28].
Knowledge of the clinic’s existence must be spread among referring clinicians and general practitioners through more information from the oncology departments and LECs and strengthened cross-sector cooperation.
Conclusion
This study is the first to present EORTC QLQ-SURV100 data on employment status among CSs with late effects and unmet needs. Three-quarters of CSs within working age seen in the LEC have reduced employment status. This is associated with a lower role functioning score, higher loss of income score, and lower global health status score. Identifying and treating late effects early in cancer survivorship are important to secure CSs’ attachment to the labour market, ensuring their financial and social well-being and reducing the societal socioeconomic burden.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request. The QLQ-SURV100 can be requested on the website of the EORTC QLG: EORTC Quality of Life Website https://qol.eortc.org/.
References
Lundberg FE, et al. Trends in cancer survival in the Nordic countries 1990–2016: the NORDCAN survival studies. Acta Oncol. 2020;59(11):1266–74. https://doi.org/10.1080/0284186X.2020.1822544.
The Danish Health Data Authority, The Cancer Registry, New cancer cases 2021. [cited 2023 23. May]; Available from: https://sundhedsdatastyrelsen.dk/da/find-tal-og-analyser/tal-og-analyser/sygdomme-og-behandlinger/kraeft/kraeft_nyetilfaelde_aarsrapport.
Klonoff-Cohen H, Polavarapu M. Existence of late-effects instruments for cancer survivors: a systematic review. PLoS One. 2020;15(2):e0229222. https://doi.org/10.1371/journal.pone.0229222.
Emery J, et al. Management of common clinical problems experienced by survivors of cancer. Lancet. 2022;399(10334):1537–50. https://doi.org/10.1016/S0140-6736(22)00242-2.
Peteet JR. Cancer and the meaning of work. Gen Hosp Psychiatry. 2000;22(3):200–5. https://doi.org/10.1016/s0163-8343(00)00076-1.
EORTC, Quality of Life. 2023. Available from: https://qol.eortc.org/quality-of-life/.
van Leeuwen M, et al. Phase III study of the European Organisation for Research and Treatment of Cancer Quality of Life cancer survivorship core questionnaire. J Cancer Surviv. 2023;17(4):1111–30. https://doi.org/10.1007/s11764-021-01160-1.
de Moor JS, et al. Employment outcomes among cancer survivors in the United States: implications for cancer care delivery. J Natl Cancer Inst. 2021;113(5):641–4. https://doi.org/10.1093/jnci/djaa084.
Tamminga SJ, et al. Long-term employment status and quality of life after cancer: A longitudinal prospective cohort study from diagnosis up to and including 5 years post diagnosis. Work. 2020;66(4):901–7. https://doi.org/10.3233/WOR-203234.
Bøhn SH, et al. Work status changes and associated factors in a nationwide sample of Norwegian long-term breast cancer survivors. J Cancer Surviv; 2022. https://doi.org/10.1007/s11764-022-01202-2.
Kjær, T., Karlsen, R., Dalton, S., Levinsen, A. K., Johansen, C., Adersen, K., Vidensopsamling på senfølger efter kræft hos voksne. 2017. [cited 2023 12. September]; Available from: https://www.cancer.dk/fagfolk/rapporter/vidensopsamling-pa-senfoelger-efter-kraeft-hos-voksne/.
Fayers PM, Aaronson NK, Bjordal K, Grønvold M, Curran D, Bottomley A. EORTC QLQ-C30 Scoring Manual. 3rd ed. Brussels: European Organisation for Research and Treatment of Cancer; 2001.
Harris PA, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
Harris PA, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Nolte S, et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur J Cancer. 2019;107:153–63. https://doi.org/10.1016/j.ejca.2018.11.024.
Scott NW, Fayers P, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, Gundy C, et al. EORTC QLQ-C30 Reference Values. Brussels: European Organisation for Research and Treatment of Cancer; 2008.
Statistics Denmark, StatBank Denmark, RAS200: Activity and employment rates (end November) by frequency, sex, ancestry, age, region and time. 2023. Available from: https://statistikbanken.dk/RAS200.
Statistics Denmark, StatBank Denmark, PEN113: Disability pensioner by recipients, type of benefits, sex, age, region and time. 2023. Available from: https://www.statistikbanken.dk/PEN113.
Mehnert A. Employment and work-related issues in cancer survivors. Crit Rev Oncol Hematol. 2011;77(2):109–30. https://doi.org/10.1016/j.critrevonc.2010.01.004.
Firkins J, et al. Quality of life in “chronic” cancer survivors: a meta-analysis. J Cancer Surviv. 2020;14(4):504–17. https://doi.org/10.1007/s11764-020-00869-9.
Götze H, et al. Comorbid conditions and health-related quality of life in long-term cancer survivors-associations with demographic and medical characteristics. J Cancer Surviv. 2018;12(5):712–20. https://doi.org/10.1007/s11764-018-0708-6.
Heinesen E, Imai S, Maruyama S. Employment, job skills and occupational mobility of cancer survivors. J Health Econ. 2018;58:151–75. https://doi.org/10.1016/j.jhealeco.2018.01.006.
Alzehr A, et al. The economic impact of cancer diagnosis to individuals and their families: a systematic review. Support Care Cancer. 2022;30(8):6385–404. https://doi.org/10.1007/s00520-022-06913-x.
Thompson AE, et al. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. 2016;17:38. https://doi.org/10.1186/s12875-016-0440-0.
Bertakis KD, et al. Gender differences in the utilization of health care services. J Fam Pract. 2000;49(2):147–52.
Lerhmann-Lerche CS, et al. Educational level and first-time PSA testing in general practice. Scand J Urol. 2019;53(5):275–81. https://doi.org/10.1080/21681805.2019.1681503.
Balasubramaniam K, et al. Gynecological cancer alarm symptoms: is contact with specialist care associated with lifestyle and socioeconomic status? A population-based study. Acta Obstet Gynecol Scand. 2016;95(9):976–83. https://doi.org/10.1111/aogs.12927.
Levinsen AKG, et al. Social inequality in cancer survivorship: educational differences in health-related quality of life among 27,857 cancer survivors in Denmark. Cancer Med. 2023;12(19):20150–62. https://doi.org/10.1002/cam4.6596.
The Danish Cancer Society. Cancer patients' needs and experiences with the healthcare system in the follow-up and after-care process, The Danish Cancer Society's barometer survey, 2019. [cited 2023 12. September]; Available from: https://www.cancer.dk/fagfolk/rapporter/kraeftpatienters-behov-og-oplevelser-med-sundhedsvaesenet-i-opfoelgnings-og-efterforloebet-2019/.
Acknowledgements
We would like to thank the cancer survivors for their willingness to participate in this study. We also thank Sören Möller for his statistical advice.
Funding
Open access funding provided by University Library of Southern Denmark
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Data collections were performed by Annette Sicko Skovgaards, Thea Otto Mattsson, and Lærke Kjær Tolstrup. Analyses were performed by Annette Sicko Skovgaards. The first draft of the manuscript was written by Annette Sicko Skovgaards, and all authors commented on previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Data Protection Agency Odense University Hospital (16.11.2021 Journal nr. 21/61098).
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 17 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Skovgaards, A.S., Mattsson, T.O. & Tolstrup, L.K. Employment status among cancer survivors in a Late Effects Clinic in Denmark. J Cancer Surviv (2023). https://doi.org/10.1007/s11764-023-01496-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-023-01496-w