Abstract
Purpose
Erectile function changes after prostate cancer (PCa) treatment are well documented, but less understood is the relative impact of prostate biopsy and active surveillance on sexual well-being. It is unknown whether potential negative impacts are exclusive to patients who have been treated for PCa, or whether the diagnosis itself or the experience of biopsy may also impact sexual well-being. Sexual satisfaction is an important yet understudied indicator of sexual well-being in this population. This study examines sexual satisfaction and its predictors across several comparison groups to explore relative impact.
Methods
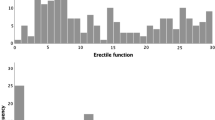
At baseline and 12 months, questionnaire data was collected in four samples: (1) following PCa treatment, (2) active surveillance, (3) negative prostate biopsy result, and (4) controls receiving no biopsy or treatment. Predictors assessed included group, erectile function, communication style, and partner involvement.
Results
Sexual satisfaction declined in the active treatment group, no changes were observed in active surveillance or non-PCa control, and improvements were observed in the biopsy group. Predictors of sexual satisfaction over and above erectile function included restrictive communication (i.e. protective buffering) and perceived partner involvement. For higher levels of erectile function, a higher perceived degree of partner involvement was protective of sexual satisfaction.
Conclusion
Sexual satisfaction is an important indicator of sexual well-being and is negatively impacted following PCa treatment, but not active surveillance or prostate biopsy.
Implications for Cancer Survivors
Communication and partner involvement are potentially modifiable factors to be considered for intervention and may promote sexual satisfaction following PCa treatment. Patients experiencing negative biopsy, who note lower sexual satisfaction may experience improved satisfaction with time, and those under active surveillance who worry about sexual satisfaction may find reassurance from these results.


Similar content being viewed by others
References
Mitchell KR, et al. What is sexual wellbeing and why does it matter for public health? The Lancet Public Health. 2021;6(8):e608–13.
Santos-Iglesias P, Byers ES, Moglia R. Sexual well-being of older men and women. Can J Hum Sex. 2016;25(2):86–98.
Santos-Iglesias P, Rana M, Walker LM. A systematic review of sexual satisfaction in prostate cancer patients. Sexual Med Rev. 2020;8(3):450–65.
Howlett K, et al. Changes in sexual function on mood and quality of life in patients undergoing radiation therapy for prostate cancer. Oncol Nurs Forum. 2010;37(1):E58-66.
Fujita K, et al. Serial prostate biopsies are associated with an increased risk of erectile dysfunction in men with prostate cancer on active surveillance. J Urol. 2009;182(6):2664–9.
Akbal C, et al. Erectile function in prostate cancer–free patients who underwent prostate saturation biopsy. Eur Urol. 2008;53(3):540–6.
Zisman A, et al. The impact of prostate biopsy on patient well-being: a prospective study of pain, anxiety and erectile dysfunction. J Urol. 2001;165(2):445–54.
Walker LM, Santos-Iglesias P. On the relationship between erectile function and sexual distress in men with prostate cancer. Arch Sex Behav. 2020;49:1575–88.
Lawrance K, Byers ES. Sexual satisfaction in long-term heterosexual relationships: the interpersonal exchange model of sexual satisfaction. Pers Relat. 1995;2:267–85.
Davison SL, et al. The relationship between self-reported sexual satisfaction and general well-being in women. J Sexual Med. 2009;6(10):2690–7.
Dundon CM, Rellini AH. More than sexual function: predictors of sexual satisfaction in a sample of women age 40–70. J Sex Med. 2010;7(2):896–904.
Henderson AW, Lehavot K, Simoni JM. Ecological models of sexual satisfaction among lesbian/bisexual and heterosexual women. Arch Sex Behav. 2009;38:50–65.
Flynn KE, et al. Sexual functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS®). Psychooncology. 2011;20(4):378–86.
Terrier JE, et al. Decrease in intercourse satisfaction in men who recover erections after radical prostatectomy. J Sexual Med. 2018;15(8):1133–9.
WHOQOL Group. Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Qual Life Res. 1993;2(2):1531–59.
Deho F, et al. Anatomical radical retropubic prostatectomy in patients with a preexisting three-piece inflatable prosthesis: a series of case reports. J Sex Med. 2009;6(2):578–83.
Dubbelman YD, Wildhagen MF, Dohle GR. Penile vascular evaluation and sexual function before and after radical retropubic prostatectomy: 5-year follow-up. Int J Androl. 2008;31(5):483–9.
Perez MA, Skinner EC, Meyerowitz BE. Sexuality and intimacy following radical prostatectomy: patient and partner perspectives. Health Psychol. 2002;21(3):288–93.
Beckendorf V, et al. Changes in sexual function after radiotherapy treatment of prostate cancer. Br J Urol. 1996;77(1):118–23.
van der Wielen GJ, van Putten WLJ, Incrocci L. Sexual function after three-dimensional conformal radiotherapy for prostate cancer: results from a dose-escalation trial. Int J Radiat Oncol Biol Phys. 2007;68(2):479–84.
Matsushima M, et al. A prospective longitudinal survey of erectile dysfunction in patients with localized prostate cancer treated with permanent prostate brachytherapy. J Urol. 2013;189(3):1014–8.
Siglin J, et al. Time of decline in sexual function after external beam radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys. 2010;76(1):31–5.
Martin Hald G, et al. Scandinavian prostate cancer patients’ sexual problems and satisfaction with their sex life following anti-cancer treatment. Sexual Med. 2018;6(3):210–6.
Schover LR, et al. Defining sexual outcomes after treatment for localized prostate carcinoma. Cancer. 2002;95(8):1773–85.
Garos S, Kluck A, Aronoff D. Prostate cancer patients and their partners: differences in satisfaction indices and psychological variables. J Sexual Med. 2007;4(5):1394–403.
Nelson CJ, et al. Determinants of sexual satisfaction in men with prostate cancer. J Sex Med. 2007;4(5):1422–7.
Chambers SK, et al. Couple distress after localised prostate cancer. Support Care Cancer. 2013;21(11):2967–76.
Crump RT, et al. Using the Movember Foundation’s GAP3 cohort to measure the effect of active surveillance on patient-reported urinary and sexual function-a retrospective study in low-risk prostate cancer patients. Transl Androl Urol. 2021;10(6):2719–27.
Kamali K, et al. Impact of prostate needle biopsy on erectile function: a prospective study. Urologia. 2019;86(3):145–7.
Naccarato AM, et al. Psychotherapy and phosphodiesterase-5 inhibitor in early rehabilitation after radical prostatectomy: a prospective randomised controlled trial. Andrologia. 2016;48(10):1183–7.
Rossi MS, et al. Erectile function recovery after nerve-sparing radical prostatectomy for prostate cancer: is back to baseline status enough for patient satisfaction? J Sexual Med. 2016;13(4):669–78.
Wootten AC, et al. An online psychological intervention can improve the sexual satisfaction of men following treatment for localized prostate cancer: outcomes of a Randomised Controlled Trial evaluating My Road Ahead. Psychooncology. 2017;26(7):975–81.
Badr H, Taylor CL. Sexual dysfunction and spousal communication in couples coping with prostate cancer. Psychooncology. 2009;18(7):735–46.
Letts C, Tamlyn K, Byers ES. Exploring the impact of prostate cancer on men’s sexual well-being. J Psychosoc Oncol. 2010;28(5):490–510.
Arrington MI. “I don’t want to be an artificial man”: narrative reconstruction of sexuality among prostate cancer survivors. Sex Cult. 2003;7(2):30–58.
Wittmann D, et al. Exploring the role of the partner in couples’ sexual recovery after surgery for prostate cancer. Support Care Cancer. 2014;22(9):2509–15.
MacNeil S, Byers ES. Dyadic assessment of sexual self-disclosure and sexual satisfaction in heterosexual dating couples. J Soc Pers Relat. 2005;22:169–81.
MacNeil S, Byers ES. Role of sexual self-disclosure in the sexual satisfaction of long-term heterosexual couples. J Sex Res. 2009;46:1–12.
Manne SL, et al. Protective buffering and psychological distress among couples coping with breast cancer: the moderating role of relationship satisfaction. J Fam Psychol. 2007;21(3):380–8.
Kroemeke A, Sobczyk-Kruszelnicka M. Protective buffering and individual and relational adjustment following hematopoietic stem cell transplantation: a dyadic daily-diary study. Front Psychol. 2019;10:2195.
Lawrance K, Byers ES, Cohen JN, et al. Interpersonal exchange model of sexual satisfaction questionnaire. In: Fisher TD, et al., editors. Handbook of sexuality-related measures. New York, NY: Routledge; 2011. p. 525–30.
Rosen R, et al. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30.
Manne SL, et al. Hiding worries from one’s spouse: protective buffering among cancer patients and their spouses. Cancer Res Ther Control. 1999;8:175–88.
Casler K, Bickel L, Hackett E. Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face-to-face behavioral testing. Comput Hum Behav. 2013;29:2156–60.
Cohen J, Statistical power analysis for the behavioral sciences. 2nd ed. 1988, Mahwah, NJ: Erlbaum.
Hox JJ, Multilevel analysis. Techniques and applications. 2nd ed. 2010, New York, NY: Routledge.
Pinheiro J, et al., nlme: linear and nonlinear mixed effects models. 2018.
Katz DA, et al. Health perceptions in patients who undergo screening and workup for prostate cancer. Urology. 2007;69(2):215–20.
Cupach WR, Metts S. Sexuality and communication in close relationships. In: McKinney K, Sprecher S, editors. Sexuality in close relationships. Hillsdale, NJ: Lawrence Erlbaum; 1991. p. 93–110.
La France BH. Predicting sexual satisfaction in interpersonal relationships. South Commun J. 2010;75:195–214.
Merwin KE, Rosen NO. Perceived partner responsiveness moderates the associations between sexual talk and sexual and relationship well-being in individuals in long-term relationships. J Sex Res. 2020;57(3):351–64.
Ussher JM, et al. Renegotiating sex and intimacy after cancer: resisting the coital imperative. Cancer Nurs. 2013;36(6):454–62.
Walker LM, Wassersug RJ, Robinson JW. Psychosocial perspectives on sexual recovery after prostate cancer treatment. Nat Rev Urol. 2015;12(3):167–76.
Wittmann D, et al. The psychosocial aspects of sexual recovery after prostate cancer treatment. Int J Impot Res. 2009;21(2):99–106.
Gillespie BJ. Correlates of sexual frequency and sexual satisfaction among partnered older adults. J Sex Marital Ther. 2017;43(5):403–23.
Funding
Funding was provided for this study by a Rising Star independent investigator grant from Movember and Prostate Cancer Canada (now the Canadian Cancer Society) Grant # RS2015-03.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design, data collection and analysis, and design and writing of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Research Ethics Board approval was obtained for this study from the Research Ethics Board of Alberta – Cancer Committee.
Consent to participate
All participants provided informed consent.
Consent for publication
Consent to publish was obtained.
Competing interests
Dr. Lauren Walker’s work is supported unrestricted educational grants for the Androgen Deprivation Therapy Educational Program (www.LifeonADT.com). These grants are administered by the Prostate Cancer Centre in Calgary, Alberta for the Canadian Program (by Tolmar, Astellas, Novartis, Pfizer) and by the European Association of Urology for the Europe Programme (Bayer, Astellas).
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Walker, L.M., Santos-Iglesias, P. Sexual satisfaction in prostate cancer: a multi-group comparison study of treated patients, patients under active surveillance, patients with negative biopsy, and controls. J Cancer Surviv (2023). https://doi.org/10.1007/s11764-023-01420-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-023-01420-2