Abstract
Purpose
Patients with a rare cancer face difficulties during their disease trajectory, such as delayed diagnosis and lack of expert care. However, little is known about their perceived quality of care (QoC) and quality of life (QoL) in the advanced disease stage. We aimed to assess the QoC and QoL as experienced by patients with advanced rare cancers compared to patients with advanced common cancers.
Methods
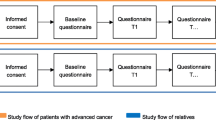
In this cross-sectional study, baseline data of patients with advanced cancer from the multicentre, longitudinal, observational eQuipe study were analysed. Multivariable linear regression analyses were conducted to assess differences in experienced QoC (continuity of care, continuity of information, and satisfaction with care) and QoL (functioning, symptoms, overall QoL, and social wellbeing) between advanced rare and common cancer patients.
Results
Of the 1087 included patients, 106 (9.8%) had a rare cancer type. In comparison to patients with advanced common cancers, patients with advanced rare cancers experienced significantly lower continuity of care (77.8 vs. 71.1 respectively, p = 0.011) and social functioning (78.8 vs. 72.6 respectively, p = 0.012). No differences were found regarding continuity of information, satisfaction with care, overall QoL, and social wellbeing.
Conclusions
Patients with advanced rare cancers experience less continuity of care, and the impact of the disease on social and family life seems higher compared to patients with advanced common cancers.
Implications for Cancer Survivors
To enhance the QoC and QoL of patients with advanced rare cancers, supportive care should mainly focus on improving continuity of care and patients’ social functioning.

Similar content being viewed by others
References
Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–87. https://doi.org/10.1016/j.ejca.2018.07.005.
Gatta G, Capocaccia R, Botta L, Mallone S, de Angelis R, Ardanaz E, et al. Burden and centralised treatment in Europe of rare tumours: results of RARECAREnet—a population-based study. Lancet Oncol. 2017;18(8):1022–39. https://doi.org/10.1016/S1470-2045(17)30445-X.
Gatta G, van der Zwan JM, Casali PG, Siesling S, Dei Tos AP, Kunkler I, et al. Rare cancers are not so rare: the rare cancer burden in Europe. Eur J Canc. 2011;47(17):2493–511. https://doi.org/10.1016/j.ejca.2011.08.008.
de Heus E, Duijts SFA, van der Zwan JM, Kapiteijn E, Nieveen van Dijkum EJM, van Herpen CML, et al. The gap between rare and common cancers still exists: results from a population-based study in the Netherlands. Eur J Canc. 2022;167:103–11. https://doi.org/10.1016/j.ejca.2022.03.001.
Ray-Coquard I, Pujade Lauraine E, le Cesne A, Pautier P, Vacher Lavenue MC, Trama A, et al. Improving treatment results with reference centres for rare cancers: where do we stand? Eur J Canc. 2017;77:90–8. https://doi.org/10.1016/j.ejca.2017.02.006.
DeSantis CE, Kramer JL, Jemal A. The burden of rare cancers in the United States. CA Cancer J Clin. 2017;67(4):261–72. https://doi.org/10.3322/caac.21400.
Drabbe C, Grünhagen DJ, van Houdt WJ, Braam PM, Soomers VLMN, van der Hage JA, et al. Diagnosed with a rare cancer: experiences of adult sarcoma survivors with the healthcare system—results from the SURVSARC Study. Cancers. 2021;13(4):679. https://doi.org/10.3390/cancers13040679.
Duijts SFA, van der Zwan JM. Rare cancers and cancer of unknown primary: here’s what you should know! Eur J Cancer Care. 2021;30(6):e13508. https://doi.org/10.1111/ecc.13508.
Pillai RK, Jayasree K. Rare cancers: challenges & issues. Indian J Med Res. 2017;145(1):17. https://doi.org/10.4103/ijmr.IJMR_915_14.
Loggers ET, Prigerson HG. The end-of-life experience of patients with rare cancers and their caregivers. Rare Tumors. 2014;6(1):5281. https://doi.org/10.4081/rt.2014.5281.
Blaauwgeers H, Ho V, Kwast A, van der Zwan JM. Kankerzorg in beeld - Zeldzame kanker. Utrecht: IKNL; 2018.
Soomers VLMN, van der Graaf WTA, Zaidi S, Kaal SEJ, Hayes AJ, Schreuder BHWB, et al. The route to diagnosis of sarcoma patients: results from an interview study in the Netherlands and the United Kingdom. PLoS One. 2020;15(12): e0243439. https://doi.org/10.1371/journal.pone.0243439.
Alessy SA, Alhajji M, Rawlinson J, Baker M, Davies EA. Factors influencing cancer patients’ experiences of care in the USA, United Kingdom, and Canada: a systematic review. eClinicalMedicine. 2022;47. https://doi.org/10.1016/j.eclinm.2022.101405.
Campbell SM, Roland MO, Buetow SA. Defining quality of care. Soc Sci Med. 2000;51(11):1611–25. https://doi.org/10.1016/S0277-9536(00)00057-5.
de Vogel-Voogt E, van der Heide A, van Leeuwen AF, Visser AP, van der Rijt CCD, van der Maas PJ. Patient evaluation of end-of-life care. Palliat Med. 2007;21(3):243–8. https://doi.org/10.1177/0269216307077352.
van Roij J, de Zeeuw B, Zijlstra M, Claessens N, Raijmakers N, van de Poll-Franse L, et al. Shared perspectives of patients with advanced cancer and their informal caregivers on essential aspects of health care: a qualitative study. J Palliat Care. 2021. https://doi.org/10.1177/0825859721989524
de Heus E, Engelen V, Dingemans I, Richel C, Schrieks M, van der Zwan JM, et al. Differences in health care experiences between rare cancer and common cancer patients: results from a national cross-sectional survey. Orphanet J Rare Dis. 2021;16(1):249. https://doi.org/10.21203/rs.3.rs-122659/v1.
Feinberg Y, Law C, Singh S, Wright FC. Patient experiences of having a neuroendocrine tumour: a qualitative study. Eur J Oncol Nurs. 2013;17(5):541–5. https://doi.org/10.1016/j.ejon.2013.02.003.
Griffiths J, Willard C, Burgess A, Amir Z, Luker K. Meeting the ongoing needs of survivors of rarer cancer. Eur J Oncol Nurs. 2007;11(5):434–41. https://doi.org/10.1016/j.ejon.2007.09.004.
Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219. https://doi.org/10.1136/bmj.327.7425.1219.
Molster C, Urwin D, di Pietro L, Fookes M, Petrie D, van der Laan S, et al. Survey of healthcare experiences of Australian adults living with rare diseases. Orphanet J Rare Dis. 2016;11(1):1–12. https://doi.org/10.1186/s13023-016-0409-z.
Hannon B, Swami N, Krzyzanowska MK, Leighl N, Rodin G, Le LW, et al. Satisfaction with oncology care among patients with advanced cancer and their caregivers. Qual Life Res. 2013;22(9):2341–9. https://doi.org/10.1007/s11136-013-0371-3.
Engel M, Brinkman-Stoppelenburg A, Nieboer D, van der Heide A. Satisfaction with care of hospitalised patients with advanced cancer in the Netherlands. Eur J Cancer Care. 2018;27(5): e12874. https://doi.org/10.1111/ecc.12874.
Bogart KR, Irvin VL. Health-related quality of life among adults with diverse rare disorders. Orphanet J Rare Dis. 2017;12(1):177. https://doi.org/10.1186/s13023-017-0730-1.
Robinson KM, Christensen KB, Ottesen B, Krasnik A. Diagnostic delay, quality of life and patient satisfaction among women diagnosed with endometrial or ovarian cancer: a nationwide Danish study. Qual Life Res. 2012;21(9):1519–25. https://doi.org/10.1007/s11136-011-0077-3.
Hasegawa T, Goto N, Matsumoto N, Sasaki Y, Ishiguro T, Kuzuya N, et al. Prevalence of unmet needs and correlated factors in advanced-stage cancer patients receiving rehabilitation. Supp Care Cancer. 2016;24(11):4761–7. https://doi.org/10.1007/s00520-016-3327-7.
van Roij J, Brom L, Youssef-El Soud M, van de Poll-Franse L, Raijmakers NJH. Social consequences of advanced cancer in patients and their informal caregivers: a qualitative study. Support Care Cancer. 2019;27(4):1187. https://doi.org/10.1007/s00520-018-4437-1.
Siemens W, Schönsteiner SS, Orellana-Rios CL, Schaekel U, Kessler J, Eschbach C, et al. Severe symptoms and very low quality-of-life among outpatients newly diagnosed with advanced cancer: data from a multicenter cohort study. Support Care Cancer. 2020;28(11):5547–55. https://doi.org/10.1007/s00520-020-05388-y.
van Roij J, Raijmakers N, Ham L, van den Beuken-van EM, van den Borne B, Creemers GJ, et al. Quality of life and quality of care as experienced by patients with advanced cancer and their relatives: a multicentre observational cohort study (eQuiPe). Eur J Cancer. 2022;165:125–35. https://doi.org/10.1016/j.ejca.2022.01.039.
RARECARENet. Cancer List. Available from: https://www.rarecarenet.eu/rarecarenet/index.php/cancerlist. Accessed 15 March 2022
van Roij J, Zijlstra M, Ham L, Brom L, Fransen H, Vreugdenhil A, et al. Prospective cohort study of patients with advanced cancer and their relatives on the experienced quality of care and life (eQuiPe study): a study protocol. BMC Palliat Care. 2020;19(1):1–9. https://doi.org/10.1186/s12904-020-00642-w.
Claessen SJJ, Francke AL, Sixma HJ, de Veer AJE, Deliens L. Measuring patients’ experiences with palliative care: the Consumer Quality Index Palliative Care. BMJ Support Palliat Care. 2012;2(4):367–72. https://doi.org/10.1136/bmjspcare-2011-000055.
Brédart A, Bottomley A, Blazeby JM, Conroy T, Coens C, D’Haese S, et al. An international prospective study of the EORTC cancer in-patient satisfaction with care measure (EORTC IN-PATSAT32). Eur J Cancer. 2005;41(14):2120–31. https://doi.org/10.1016/j.ejca.2005.04.041.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76. https://doi.org/10.1093/jnci/85.5.365.
Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A, et al. The EORTC QLQ-C30 scoring manual. 3rd ed. Brussels: European Organisation for Research and Treatment of Cancer; 2001.
Giesinger JM, Kieffer JM, Fayers PM, Groenvold M, Petersen MA, Scott NW, et al. Replication and validation of higher order models demonstrated that a summary score for the EORTC QLQ-C30 is robust. J Clin Epidemiol. 2016;69:79–88. https://doi.org/10.1016/j.jclinepi.2015.08.007.
Efficace F, Cottone F, Sommer K, Kieffer J, Aaronson N, Fayers P, et al. Validation of the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 summary score in patients with hematologic malignancies. Value Health. 2019;22(11):1303–10. https://doi.org/10.1016/j.jval.2019.06.004.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–9. https://doi.org/10.1200/JCO.1993.11.3.570.
Luckett T, King MT, Butow PN, Oguchi M, Rankin N, Price MA, et al. Choosing between the EORTC QLQ-C30 and FACT-G for measuring health-related quality of life in cancer clinical research: issues, evidence and recommendations. Ann Oncol. 2011;22(10):2179–90. https://doi.org/10.1093/annonc/mdq721.
OECD, Eurostat, UNESCO Institute for Statistics. ISCED. Operational Manual: Guidelines for Classifying National Education Programmes and Related Qualifications. Paris: OECD Publishing; 2011. p. 2015.
Newton JC, O’Connor M, Saunders C, Ali S, Nowak AK, Halkett GKB. “Who can I ring? Where can I go?” Living with advanced cancer whilst navigating the health system: a qualitative study. Support Care Cancer. 2022;30(8):6817–26. https://doi.org/10.1007/s00520-022-07107-1.
Oosterveld-Vlug MG, Custers B, Hofstede J, Donker GA, Rijken PM, Korevaar JC, et al. What are essential elements of high-quality palliative care at home? An interview study among patients and relatives faced with advanced cancer. BMC Palliat Care. 2019;18(1):1–10. https://doi.org/10.1186/s12904-019-0485-7.
Lewis RA, Neal RD, Hendry M, France B, Williams NH, Russell D, et al. Patients’ and healthcare professionals’ views of cancer follow-up: systematic review. Br J Gen Pract. 2009;59(564):533–40. https://doi.org/10.3399/bjgp09X453576.
Haggerty JL, Roberge D, Freeman GK, Beaulieu C. Experienced continuity of care when patients see multiple clinicians: a qualitative metasummary. Ann Fam Med. 2013;11(3):262–71. https://doi.org/10.1370/afm.1499.
Jackson J, MacKean G, Cooke T, Lahtinen M. Patient and provider experiences with relationship, information, and management continuity. Patient Exp J. 2017;4(3):38–47. https://doi.org/10.35680/2372-0247.1192.
NFK. Sociale steun, begrip en nazorg bij kanker: wat is jouw ervaring? 2021. [Internet].
Rodríguez AM, Mayo NE, Gagnon B. Independent contributors to overall quality of life in people with advanced cancer. Br J Cancer. 2013;108(9):1790–800. https://doi.org/10.1038/bjc.2013.146.
Scott NW, Fayers PM, Aaronson NK, Bottomly A, de Graeff A, Groenvold M, et al. EORTC QLQ-C30 Reference Values. Brussels; 2008.
Raijmakers NJH, Zijlstra M, van Roij J, Husson O, Oerlemans S, van de Poll-Franse LV. Health-related quality of life among cancer patients in their last year of life: results from the PROFILES registry. Support Care Cancer. 2018;26(10):3397–404. https://doi.org/10.1007/s00520-018-4181-6.
Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211. https://doi.org/10.2147/JMDH.S104807.
Fadnes LT, Taube A, Tylleskär T. How to identify information bias due to self-reporting in epidemiological research. Int J Epidemiol. 2009;7(2):1–21.
Bedard G, Zeng L, Zhang L, Lauzon N, Holden L, Tsao M, et al. Minimal important differences in the EORTC QLQ-C30 in patients with advanced cancer. Asia Pac J Clin Oncol. 2014;10(2):109–17. https://doi.org/10.1111/ajco.12070.
Cocks K, King MT, Velikova G, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for determination of sample size and interpretation of the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. J Clin Oncol. 2011;29(1):89–96. https://doi.org/10.1200/JCO.2010.28.0107.
van der Plas AGM, Vissers KC, Francke AL, Donker GA, Jansen WJJ, Deliens L, et al. Involvement of a case manager in palliative care reduces hospitalisations at the end of life in cancer patients; a mortality follow-back study in primary care. PLoS One. 2015;10(7). https://doi.org/10.1371/journal.pone.0133197
King M, Jones L, Richardson A, Murad S, Irving A, Aslett H, et al. The relationship between patients’ experiences of continuity of cancer care and health outcomes: a mixed methods study. Br J Cancer. 2008;98(3):529–36. https://doi.org/10.1038/sj.bjc.6604164.
Chen HM, Tu YH, Chen CM. Effect of continuity of care on quality of life in older adults with chronic diseases: a meta-analysis. Clin Nurs Res. 2017;26(3):266–84. https://doi.org/10.1177/1054773815625467.
Stegmann ME, Geerse OP, Tange D, Richel C, Brom L, Engelen V, et al. Experiences and needs of patients with incurable cancer regarding advance care planning: results from a national cross-sectional survey. Support Care Cancer. 2020;28(9):4211–7. https://doi.org/10.1007/s00520-019-05285-z.
Elrod JK, Fortenberry JL. The hub-and-spoke organization design: an avenue for serving patients well. BMC Health Serv Res. 2017;17. https://doi.org/10.1186/s12913-017-2341-x
de Heus E, van der Zwan JM, Husson O, Frissen A, van Herpen CML, Merkx MAW, et al. Unmet supportive care needs of patients with rare cancer: a systematic review. Eur J Cancer Care. 2021;30(6): e13502. https://doi.org/10.1111/ecc.13502.
Acknowledgements
We thank all participating hospitals and healthcare professionals for their effort and support regarding this study. Moreover, we thank all participating patients for completing the questionnaires and sharing their experiences in the last phase of their lives.
Funding
The eQuiPe study is funded by the Roparun Foundation.
Author information
Authors and Affiliations
Contributions
Anouk van Oss: Conceptualisation, data curation, methodology, statistical analysis, interpretation, writing (original draft). Linda Brom: Conceptualisation, methodology, interpretation, writing (review and editing). Saskia F.A. Duijts: Conceptualisation, methodology, interpretation, writing (review and editing). Natasja JH Raijmakers: Methodology, interpretation, writing (review and editing). Hanneke van Laarhoven: Writing (review and editing). Evelien Kuip: Writing (review and editing).
Corresponding author
Ethics declarations
Ethics approval
The eQuiPe study protocol has been reviewed by the Medical Ethical Committee (METC) of the Netherlands Cancer Institute (NKI) in Amsterdam, the Netherlands (METC17.1491). The METC has exempted this observational research from full ethical review, according to the Dutch Medical Research Involving Human Subjects Act (WMO). Informed consent was obtained from all the participating patients.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent to publish
Written informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van Oss, A., Duijts, S.F.A., van Laarhoven, H. et al. Quality of care and quality of life as experienced by patients with advanced cancer of a rare tumour type: results of the multicentre observational eQuiPe study. J Cancer Surviv 17, 997–1007 (2023). https://doi.org/10.1007/s11764-022-01323-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01323-8