Abstract
Background
Concomitant tricuspid valve (TV) repair is a safe and effective procedure to protect against late moderate or greater tricuspid regurgitation (TR) after left-sided valve surgery, but studies regarding its late outcomes and recurrent TR are limited. This study aimed to reveal the late outcomes and explore the predictors of mortality and recurrent TR among patients who underwent concomitant TV repair with left-sided valve surgery.
Methods and results
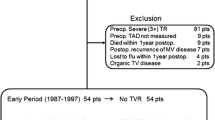
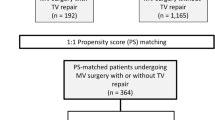
This study included 645 patients (mean age, 69.7 years; 44% male) who underwent concomitant TV repair with left-sided valve surgery (mitral valve surgery in 594 cases, aortic valve surgery in 172 cases) from 2006–2020. Preoperative TR was grade 4, 3, and less than 2 in 85, 235, and 325 patients, respectively. The median follow-up period was 4.6 (IQR 1.7–7.8) years. The in-hospital or 30-day mortality was 1.7% (n = 11). Regarding long-term outcomes after TV repair, 90.3% and 80.8% achieved 5- and 10-year survival, respectively, while 96.1% and 88.8% achieved 5- and 10-year freedom from recurrent TR, respectively. The following were independent predictors of overall mortality on multivariate analysis in patients with preoperative TR grade ≥ 3: prior pacemaker implantation, preoperative renal dysfunction, diabetes mellitus and NYHA class ≥ 3. Also, suture annuloplasty and ring type of ring annuloplasty were not independent risk factors for recurrent TR, classified as grade ≥ 3.
Conclusions
Concomitant TV repair with left-sided valve surgery had acceptable outcomes in terms of survival and TR durability. In patients with preoperative TR grade ≥ 3, preoperative patient status had negative impacts on prognosis.



Similar content being viewed by others
Data availability
The datasets generated and/ or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kwak JJ, Kim YJ, Kim MK, Kim HK, Park JS, Kim KH, et al. Development of tricuspid regurgitation late after left-sided valve surgery: a single-center experience with long-term echocardiographic examinations. Am Heart J. 2008;155:732–7.
Izumi C, Miyake M, Takahashi S, Matsutani H, Hashiwada S, Kuwano K, et al. Progression of isolated tricuspid regurgitation late after left-sided valve surgery: clinical features and mechanisms. Circ J. 2011;75:2902–7.
Lee H, Sung K, Kim WS, Lee YT, Park SJ, Carriere KC, et al. Clinical and hemodynamic influences of prophylactic tricuspid annuloplasty in mechanical mitral valve replacement. J Thorac Cardiovasc Surg. 2016;151:788–95.
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, et al. ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation 2021. 2020;143:e72–227.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease: developed by the task force for the management of valvular heart disease of the European society of cardiology (ESC) and the European association for cardio-thoracic surgery (EACTS). Eur J Cardio Thorac Surg. 2021;60:727–800.
Jeganathan R, Armstrong S, Al-Alao B, David T. The risk and outcomes of reoperative tricuspid valve surgery. Ann Thorac Surg. 2013;95:119–24.
Fujita T, Kobayashi J, Toda K, Nakajima H, Iba Y, Shimahara Y, et al. Long-term outcome of combined valve repair and maze procedure for nonrheumatic mitral regurgitation. J Thorac Cardiovasc Surg. 2010;140:1332–7.
Kakuta T, Fukushima S, Minami K, Saito T, Kawamoto N, Tadokoro N, et al. Novel risk score for predictiong recurrence of atrial fibrillation after the cryo-maze procedure. Eur J Cardiothorac Surg. 2021;59:1218–25.
Iqbal S, Chen PH. Passive liver congestion and hypoxic hepatitis. In: Cardio-hepatology: connections between hepatic and cardiovascular disease. Elsevier; 2023. p. 123–32.
Parolari A, Barili F, Pilozzi A, Pacini D. Ring or suture annuloplasty for tricuspid regurgitation? A meta-analysis review. Ann Thorac Surg. 2014;98:2255–63.
Saran N, Dearani JA, Said SM, Greason KL, Pochettino A, Stulak JM, et al. Long-term outcomes of patients undergoing tricuspid valve surgery. Eur J Cardio Thorac Surg. 2019;56:950–8.
Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004;43:405–9.
Behm CZ, Nath J, Foster E. Clinical correlates and mortality of hemodynamically significant tricuspid regurgitation. J Heart Valve Dis. 2004;13:784–9.
Amano M, Izumi C, Taniguchi T, Morimoto T, Miyake M, Nishimura S, et al. Impact of concomitant tricuspid regurgitation on long-term outcomes in severe aortic stenosis. Eur Heart J Cardiovasc Imaging. 2019;20:353–60.
Groves PH, Lewis NP, Ikram S, Maire R, Hall RJ. Reduced exercise capacity in patients with tricuspid regurgitation after successful mitral valve replacement for rheumatic mitral valve disease. Heart. 1991;66:295–301.
Dreyfus J, Ghalem N, Garbarz E, Cimadevilla C, Nataf P, Vahanian A, et al. Timing of referral of patients with severe isolated tricuspid valve regurgitation to surgeons (from a French nationwide database). Am J Cardiol. 2018;122:323–6.
Antunes MJ, Rodríguez-Palomares J, Prendergast B, De Bonis M, Rosenhek R, Al-Attar N, et al. Management of tricuspid valve regurgitation. Eur J Cardio Thorac Surg. 2017;52:1022–30.
Hung J, Koelling T, Semigran MJ, Dec GW, Levine RA, Di Salvo TG. Usefulness of echocardiographic determined tricuspid regurgitation in predicting event-free survival in severe heart failure secondary to idiopathic-dilated cardiomyopathy or to ischemic cardiomyopathy. Am J Cardiol. 1998;82:1301–3.
Izumi C. Isolated functional tricuspid regurgitation: when should we go to surgical treatment? J Cardiol. 2020;75:339–43.
Kim JB, Jung SH, Choo SJ, Chung CH, Lee JW. Clinical and echocardiographic outcomes after surgery for severe isolated tricuspid regurgitation. J Thorac Cardiovasc Surg. 2013;146:278–84.
Dreyfus J, Audureau E, Bohbot Y, Coisne A, Lavie-Badie Y, Bouchery M, et al. TRI-SCORE: a new risk score for in-hospital mortality prediction after isolated tricuspid valve surgery. Eur Heart J. 2022;43:654–62.
Butcher SC, Fortuni F, Dietz MF, Prihadi EA, van der Bijl P, Ajmone Marsan N, et al. Renal function in patients with significant tricuspid regurgitation: pathophysiological mechanisms and prognostic implications. J Intern Med. 2021;290:715–27.
Rangaswami J, Bhalla V, Blair JEA, Chang TI, Costa S, Lentine KL, et al. Cardiorenal syndrome: classification, pathophysiology, diagnosis, and treatment strategies: a scientific statement from the American heart association. Circulation. 2019;139:e840-878.
Ter Maaten JM, Damman K, Verhaar MC, Paulus WJ, Duncker DJ, Cheng C, et al. Connecting heart failure with preserved ejection fraction and renal dysfunction: the role of endothelial dysfunction and inflammation. Eur J Heart Fail. 2016;18:588–98.
Hata H, Fujita T, Miura S, Shimahara Y, Kume Y, Matsumoto Y, et al. Long-term outcomes of suture vs. ring tricuspid annuloplasty for functional tricuspid regurgitation. Circ J. 2017;81:1432–8.
Bogachev-Prokophiev AV, Ovcharov MA, Sapegin AV, Lavinykov SO, Astapov DA, Ivanzov SM, et al. Rigid ring versus flexible band for tricuspid valve repair in patients scheduled for mitral valve surgery: a prospective randomised study. Heart Lung Circ. 2021;30:1949–57.
Zhu TY, Wang JG, Meng X. Is a rigid tricuspid annuloplasty ring superior to a flexible band when correcting secondary tricuspid regurgitation? Interact Cardiovasc Thorac Surg. 2013;17:1009–14.
Fukunaga N, Okada Y, Konishi Y, Murashita T, Koyama T. Late outcome of tricuspid annuloplasty using a flexible band/ring for functional tricuspid regurgitation. Circ J. 2015;79:1299–306.
Acknowledgements
We would like to thank Joseph M from Enago (www.enago.jp) for the English language review.
Funding
This research did not receive any specific graft from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Writing: KN; Critical review and revision: all authors; Final approval of the article: all authors; Accountability for all aspects of the work: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
IRB information
Reporting were approved by the National Cerebral and Cardiovascular Center Institutional Review Board (reference number: M30-026).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Noda, K., Kawamoto, N., Kainuma, S. et al. Predictors of late outcomes after concomitant tricuspid valve repair with left-sided valve surgery. Gen Thorac Cardiovasc Surg (2024). https://doi.org/10.1007/s11748-024-02033-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11748-024-02033-x