Abstract
Background
Mitral valve repair has been proved to provide better outcomes when compared with replacement in degenerative disease. However, it is still unclear that benefits of repair still remain in active endocarditis. Patient clinical conditions and severity of tissue destruction might limit successful durable repair.
Methods
Of all 247 patients who received surgery during active phase of native left-sided endocarditis from Jan 2006 to Dec 2017, 114 had mitral valve procedures due to active infection of mitral valve apparatus (38 repair and 76 replacement). Perioperative data and mid-term outcomes were retrospectively compared.
Results
Mean age was 46.4 years old. Repair group had significantly less patients with NYHA class IV (18.4% vs 56.6%, p = 0.001). Both groups had preserved ejection fraction but accompanied by severe pulmonary hypertension. Major organism was streptococci (50%) and timing of surgery was 11 days after diagnosis. Bypass and cross-clamp time were similar but repair group had significantly less combined procedures. Bi-leaflet involvement was common (47.4% vs 57.6%) and valve lesions were comparable. There was 13.2% of postoperative moderate to severe mitral regurgitation in repair group without recurrent endocarditis. Repair group tended to have better 5-year survival estimates (91.6% vs 70.0%, p = 0.08) with comparable reoperation rate (7.9% vs 2.6%). By logistic regression analysis, mitral valve replacement was more likely to be performed in patients with decompensated heart failure and combined procedures.
Conclusions
Mitral valve repair during active endocarditis can be safely performed with good mid-term outcomes, especially in selected group of patients without extremely high surgical risk.
Similar content being viewed by others
Introduction
Mitral valve repair has been continuously developed and evolved for decades [1]. It has been proved to provide excellent long-term outcomes and be considered as treatment of choice for degenerative mitral valve disease [2]. However, uncertainty remains on more challenging conditions such as active infective endocarditis (IE) [3, 4].
With previous research and recent guidelines [5, 6], early surgery should be applied for patients with active, left-sided infective endocarditis to prevent clinical deterioration and embolization [7]. But questions to be answered are what is the feasibility and durability of mitral valve repair during active phase when there are more serious clinical conditions and sicker patients. Will benefits of repair remain while mitral valve tissues are edematous, fragile, and difficult to handle, especially when compared with mitral valve replacement.
Patients and methods
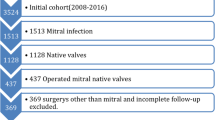
Retrospective review was conducted in our institution among patients who underwent heart valve surgery during active phase (during course of antibiotics) from January 2007 to December 2017 (Fig. 1). Inclusion criteria were age older than 18 with left-sided native valve endocarditis. Patients were excluded if they had completed course of antibiotics or prosthetic valve endocarditis (PVE).
Those patients who underwent mitral valve procedures were selected and divided to mitral valve repair and replacement groups. We further excluded patients who had only isolated ring annuloplasty from repair group in order to compare only those who had direct involvement of IE to mitral apparatus. In the final, there were 38 patients in repair group, compared to 76 patients in replacement group.
Data records were collected including preoperative characteristics, clinical status, microbiology, echocardiographic findings, mitral valve lesions and extents of involvement, timing of surgery, operative details including mitral valve repair techniques, and operative mortality. Patient status was obtained during follow-up period including survival, recurrence of IE or mitral regurgitation, and re-intervention. This study was approved by the ethics committee at Chiang Mai University (065/2562). The need of informed consent was waived because this was a retrospective study.
Statistical analysis
Categorical variables were reported as frequency (percent) and continuous variables were reported as mean ± standard deviation (SD) or median (interquartile range—IQR) depending on data distribution. The Fisher’s exact test was used to compare categorical variables and Student’s t test or rank-sum test was used to compare continuous variable between groups.
The correlation between mitral valve procedures (repair vs replacement) and mid-term outcomes (overall survival, re-intervention, and postoperative moderate to severe MR) was analyzed by multilevel survival analysis stratified by propensity score and shown with Kaplan–Meier curve.
Propensity score was calculated by logistic regression analysis method evaluating confounding by indication/contraindication between mitral valve replacement and mitral valve repair. The variables included age, gender, New York Heart Association (NYHA) functional class, creatinine clearance, preoperative mechanical ventilator, preoperative inotropic usage, preoperative persistent sepsis, preoperative end-organ damage, presence of vegetation and/or large area of destruction of mitral valve, preoperative pulmonary artery pressure (PAP), grading of mitral valve stenosis, tricuspid regurgitation, and underlying rheumatic heart disease (RHD).
Odds ratios of correlation between variables and mitral valve replacement to be more likely performed were calculated by logistic regression analysis and reported with 95% confidence interval (95% CI). All statistical calculations were performed through STATA version 15.1.
Results
Preoperative characteristics
Patients were young (mean age 46.4 years old) and predominantly male gender (68.4%). There was no difference in age, gender, renal dysfunction, previous stroke, embolization, and persistent sepsis between groups (Table 1). Replacement group was sicker due to worse functional class (NYHA class IV 18.4% in repair group VS 56.6% in replacement group, p = 0.001), more preoperative mechanical ventilation and inotropic support. European System for Cardiac Operative Risk Evaluation (EuroSCORE II) was also significantly higher for replacement group (median score 3.2 vs 9.5, p = 0.007). Left ventricular ejection fraction (LVEF) was preserved in both groups (64.6% vs 63.4%), while estimated pulmonary artery pressure was comparably high (50.0 mmHg vs 57.8 mmHg).
Streptococcus species were major causative organisms (53% vs 51%) while one-third of patients had culture-negative results. 60% of patients underwent surgery during first to second weeks after diagnosis and median time from diagnosis to surgery was similar at 11–12 days. Only 11.4% received emergency surgery in the first 24 h after diagnosis (Fig. 2).
There were 11 preoperative cerebral embolization/complications (7 infarction, 2 parenchymal lesions, and 2 intracerebral hemorrhage with mycotic aneurysm). The median timing of surgery in this group was 10.5 days, although surgery was delayed to 22 and 42 days in 2 patients who had intracerebral hemorrhage.
Surgical findings
Bi-leaflet or/and commissural involvement was the most common presentation, followed by isolated anterior leaflet involvement. Among recorded mitral valve lesions, repair group had significantly less proportion of vegetations (50.0% vs 76.3%) and peri-annular extension (2.6% vs 17.1%) (Table 2).
Operative details and mitral valve reconstruction techniques
Both groups had comparable cardiopulmonary bypass time, and aortic cross-clamp time (140 and 111 min, respectively). Active endocarditis involvement to aortic valve and concomitant aortic valve replacement were presented in 44.7% vs 48.7% of patient in each group. Replacement group tended to receive more other additional procedures (31.6% vs 47.4%, p = 0.059). The most common additional non-endocarditis-related procedure was tricuspid valve repair (13.2% vs 35.5%).
Most common reconstructive technique was leaflet resection (triangular or quadrangular) and re-approximation, followed by chordal replacement with polytetrafluoroethylene (PTFE neo-chords), and glutaraldehyde-treated autologous pericardial patch reconstruction (47.4%, 42.1%, and 42.1%, respectively). Other minor techniques included delamination/peeling of infective membrane, rheumatic repair techniques such as commissurotomy and chordal release in those who had underlying rheumatic mitral valve disease. Complete ring annuloplasty was applied in 79.0% of patients, partial posterior band in 10.5%, and without annuloplasty in 10.5%.
Operative mortality and mid-term survival
Postoperative intensive care unit (ICU) stay was fewer in mitral valve repair group (median, 1 day vs 2 days, p = 0.001) but overall postoperative hospital stay was not different between groups (median, 7.5 days vs 10 days, p = 0.238). There was 1 operative mortality (2.6%) in repair group, non-statistically different from 8 deaths (10.5%) in replacement group (p = 0.268). The causes of 9 operative deaths were from 4 severe low cardiac outputs, 3 malignant arrhythmia, and 2 new cerebral bleeding. 3 patients developed new cerebral bleeding after surgery without prior cerebral emboli and 2 of them died. In contrast, no patient with prior cerebral emboli developed new hemorrhagic infarction.
Median follow-up time was 33.2 months for repair group and 40.9 months for replacement group. Overall observed mortality was 5 deaths (13.2%) in repair group versus 21 deaths (27.6%) in replacement group, p = 0.100. Overall survival estimates between groups using Kaplan–Meier curves were not statistically different as shown in Fig. 3. 65.4% of late death were related to cardiac or valvular causes, while 15.4% were from non-cardiac-related causes such as stroke and sepsis. The reason for mortality could not be identified in 19.2% due to lack of exact information.
Mitral regurgitation, recurrent endocarditis, and re-intervention
5 patients (13.2%) in repair group had more than mild residual mitral regurgitation (3 moderate, 2 severe MR), significantly higher in comparison with 1 patient (1.5%) in replacement group, p < 0.0001. Of all 5 patients who had residual moderate–severe MR in repair group, 4 were firstly documented to have only mild MR intraoperatively but postoperative or follow-up echocardiogram showed worsen degree of MR. 4 had initial bi-leaflet or commissure involvement by infection. 1 patient underwent reoperation while the others have been medically treated and followed. Recurrent infective endocarditis was lower in repair group (0% vs 6.6%).
Overall re-interventions were 3 (7.9%) in repair group versus 2 (2.6%) in replacement group. The reasons for each reoperation in repair group were residual MR, progression of mitral stenosis, and newly developed aortic regurgitation. The reasons for each reoperation in replacement group were prosthetic valve endocarditis (PVE) and prosthetic valve dysfunction. Kaplan–Meier curves for freedom from re-intervention were comparable (Fig. 3).
Correlation between type of surgery and outcomes
Multilevel survival analysis stratified by propensity score using adjusted hazard ratio (HR) and 95% confidence interval (CI) showed non-significant correlation between type of surgery (MV replacement versus repair) and mid-term outcomes including overall mortality (HR 2.0, 95% CI 0.73–5.54, p = 0.180), re-intervention (HR 0.36, 95% CI 0.06–2.14, p = 0.260), and residual moderate to severe mitral regurgitation, although there was trend toward less likelihood of residual mitral regurgitation with mitral valve replacement (HR 0.38, 95% CI 0.13–1.12, p = 0.081).
Factors associated with mitral valve replacement in active IE
From logistic regression analysis, mitral valve replacement was to be more likely performed when patient presented with NYHA functional class IV and when there were additional combined procedures. While the mitral valve lesions such as vegetations, area of leaflet destruction, and peri-annular extension were not significantly associated with decision to replacement as shown in Table 3.
Discussion
Our results probably represented situations of surgery in active, native, mitral valve endocarditis in our region—Thailand and Southeast Asia. Patients were in young age group—30–60 years old, predominantly (45–50%) infected by streptococci group in both aortic and mitral valve with a median timing of surgery between 1 and 2 weeks after antibiotics/diagnosis. Although patients were in devastating conditions (50% of NYHA IV), outcomes of surgery were acceptable with the overall operative mortality of 7.9% and mitral valve repair could be possible in selected patients of 33.3%. Retrospectively, patients in replacement group tended to have worse preoperative risks, especially decompensated heart failure and more additional combined procedures. For mid-term (5-year) outcomes, repair group predictably had more residual MR but no difference in reoperation rate. There was non-significant trend toward better survival in repair group (91.6% vs 72.0%, p = 0.081). Type of surgery between repair and replacement had no correlation with these outcomes when using multilevel analysis stratified by propensity score.
Because our institute is a surgical referral center, this might reflect why there were high rates of culture negative IE (33%) and why median timing of surgery was at 11–12 days. Most patients were initially treated with antibiotics in primary hospitals before definite IE diagnosis has been made. This precluded the chance of positive cultures and early surgical intervention as urgent basis (in the first week after diagnosis/antibiotics) as emphasized by international guidelines [5, 6]. Postoperative antimicrobial treatment was also more difficult to judge. In those who had preoperative cerebral complications, timing of surgery was considered in the same basis at 10.5 days except when complication was cerebral hemorrhage; surgery was deferred to 4–6 weeks when hemorrhage was resolved.
The rate of successful repair was 33.3% (38 in 114) in our series when mitral apparatus was actively involved by endocarditis, excluding those patients who had only mitral annuloplasty alone due to secondary annular dilation from severe aortic valve regurgitation. The rate of successful mitral valve repair in active IE varies differently among previous literatures [8, 9] from 15% up to 100%. These non-uniform numbers might reflect differences and changes in patient status, surgical concepts, endocarditis approaches, technical expertise, and also repair enthusiasm from time to time among centers. Reported individual series might not represent “real-world” situation as shown by Toyoda et al. [10] that the rate of repair from all centers in New York and California states was 19% (with individual surgeon range from 0 to 84%). Regarding valve lesions, repair group had less vegetations and peri-annular extension. This would reflect selection bias that we did not really challenge repair in the most difficult lesions to avoid long operative time in high-risk population.
Our studies also made a small exploration on which factors that could drive decision toward mitral replacement than repair. It looks like patient risk status including decompensated heart failure and additional combined procedures had more influences than valve lesions or extension of infection. As shown by previous studies, surgical mortality rates rise higher when patients’ NYHA functional class worsen and emergency surgery should be considered in those who have refractory pulmonary edema [11, 12]. With these reasons, surgeons were likely predisposed to select quicker operation such as valve replacement to save patients’ life as first priority [13].
Although previous systematic review [14] and reports from the western countries such as Ruttmann et al. [15] and Solari et al. [16] have shown significant survival benefits after mitral repair in comparison to replacement during active IE, in contrast, we could not clearly identify the same benefit—just trend toward better survival in repair group. These findings are almost the same as reports from eastern countries such as Miura et al. [17] and Jung et al. [18]. This suggests that survival differences could be from multifactorial factors including ethnics, underlying mitral etiology (rheumatic vs degenerative), timing of surgery, causative organism, and severity of infection.
Durability of mitral valve repair during active IE might be compromised when compared to degenerative disease. This could lead to residual mitral regurgitation and re-intervention. The rate of re-intervention varies from 4 to 13% at 3–5 years and most studies [19] homogenously found that freedom from re-intervention was similar for both repair and replacement. Our study also found 7.9% re-intervention rate and comparable freedom from re-intervention.
Among various techniques [20, 21] that have been developed to reconstruct the destroyed leaflet tissues/commissures and maintain the adequacy of coaptation surfaces, pericardial patch reconstruction is the commonly used at least in 30–40% of patients with active mitral valve IE [17]. Whether the use of patch techniques reduces the durability of repair or not is the main question. Those who had significant residual MR in our series initially presented with bi-leaflet or commissural involvement that required the use of patch reconstruction. Although recent evidences [16] support the inferiority long-term outcomes of patch techniques, we believe that there are variabilities with this technique including patch type, location, extent of reconstruction, surgical experience and expertise. Further studies might be necessary to clarify this area.
Limitations
There were many limitations in our study. By nature of retrospective review, the data completeness and reliability might be compromised. Patient selection bias by surgeon was always presented as sicker patients tended to receive replacement in the fear of prolonged operative time. Our series had small numbers and the follow-up time was still short. Results could be different when sample size increases and follow-up time is longer. Also, there are always changes and improvement in endocarditis management and surgical experiences over time.
Conclusions
Mitral valve repair during active infective endocarditis provides acceptable good in-hospital and mid-term outcomes, comparable with mitral valve replacement. It can be safely performed especially in non-extremely high-risk group of patients. Better endocarditis strategy and surgical experiences might further improve both quantity and quality of repair in this challenging situation.
References
Braunberger E, Deloche A, Berrebi A, Abdallah F, Celestin JA, Meimoun P, et al. Very long-term results (more than 20 years) of valve repair with Carpentier’s techniques in nonrheumatic mitral valve insufficiency. Circulation. 2001;104(Suppl):I8–11.
DiBardino DJ, ElBardissi AW, McClure RS, Razo-Vasquez OA, Kelly NE, Cohn LH. Four decades of experience with mitral valve repair: analysis of differential indications, technical evolution, and long-term outcome. J Thorac Cardiovasc Surg. 2010;139:76–84.
Iung B, Rousseau-Paziaud J, Cormier B, Garbarz E, Fondard O, Brochet E, et al. Contemporary results of mitral valve repair for infective endocarditis. J Am Coll Cardiol. 2004;43:386–92.
Shimokawa T, Kasegawa H, Matsuyama S, Seki H, Manabe S, Fukui T, et al. Long-term outcome of mitral valve repair for infective endocarditis. Ann Thorac Surg. 2009;88:733–9.
Habib G, Lacellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Eur Heart J. 2015;36:3075–123.
Baddour LM, Wilson WR, Bayer AS, Fowler VG, Tleyjeh IM, Rybak MJ, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435–86.
Kang DH, Kim YJ, Kim SH, Sun BJ, Kim DH, Yun SC, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012;366:2466–73.
Evans CF, Gammie JS. Surgical management of mitral valve infective endocarditis. Semin Thoracic Surg. 2011;23:232–40.
Zhao D, Zhang B. Are valve repair associated with better outcomes than replacements in patients with native active valve endocarditis? Interact Cardiovasc Thorac Surg. 2014;19:1036–9.
Toyoda N, Itagaki S, Ergorova NN, Tannous H, Anyanwu AC, El-Eshmawi A, et al. Real-world outcomes of surgery for native mitral valve endocarditis. J Thorac Cardiovasc Surg. 2017;154:1906–12.
Kiefer T, Park L, Tribouilloy C, Cortes C, Castillo R, Chu V, et al. Association between valvular surgery and mortality among patients with infective endocarditis complicated by heart failure. JAMA. 2011;306:2239–47.
Prendergast BD, Tomos P. Surgery for infective endocarditis: who and when? Circulation. 2010;121:1141–52.
Gammie JS, O’Brien SM, Griffith BP, Peterson ED. Surgical treatment of mitral valve endocarditis in north America. Ann Thorac Surg. 2005;80:2199–204.
Feringa HH, Shaw LJ, Poldermans D, Hoeks S, van der Wall EE, Dion RA. Mitral valve repair and replacement in endocarditis: a systematic review of literature. Ann Thorac Surg. 2007;83:564–71.
Ruttmann E, Legit C, Poelzl G, Mueller S, Chevtchik O, Cottogni M, et al. Mitral valve repair provides improved outcome over replacement in active infective endocarditis. J Thorac Cardiovasc Surg. 2005;130:765–71.
Solari S, De Kerchove L, Tamer S, Aphram G, Baert J, Borsellino S, et al. Active infective mitral valve endocarditis: is a repair-oriented surgery safe and durable? Eur J Cardiothorac Surg. 2019;55:256–62.
Miura T, Hamawaki M, Hazama S, Hashizume K, Ariyoshi T, Sumi M, et al. Outcome of surgical management for active mitral native valve infective endocarditis: a collective review of 57 patients. Gen Thorac Cardiovasc Surg. 2014;62:488–98.
Jung SH, Je GH, Choo SJ, Song H, Chung CH, Lee JW. Surgical results of active infective native mitral valve endocarditis: repair versus replacement. Eur J Cardiothorac Surg. 2011;40:834–9.
Hu NY, Wan S. Repair of infected mitral valves: what have we learned? Surg Today. 2018;48:899–908.
Lee EM, Shapiro LM, Wells FC. Conservative operation for infective endocarditis of the mitral valve. Ann Thorac Surg. 1998;65:1087–92.
Aubert S, Barreda T, Acar C, Leprince P, Bonnet N, Ecochard R, et al. Mitral valve repair for commissural prolapse: surgical techniques and long term results. Eur J Cardiothorac Surg. 2005;28:443–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tepsuwan, T., Rimsukcharoenchai, C., Tantraworasin, A. et al. Comparison between mitral valve repair and replacement in active infective endocarditis. Gen Thorac Cardiovasc Surg 67, 1030–1037 (2019). https://doi.org/10.1007/s11748-019-01132-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01132-4