Abstract
Objectives
In this study, we aimed to determine conditions associated with the development of air bubbles in the pulmonary veins during lung resection.
Methods
A total of 28 patients who underwent lung resection at our institution between October 2016 and March 2018 were included in the study. An intraoperative transesophageal echocardiography was conducted, and the influx of air bubbles in the orifice of the pulmonary vein leading to the left atrium was observed during lung resection.
Results
The median age of all patients was 75 years. The study included 13 men and 15 women. Moreover, seven, 14, and seven patients underwent wedge resection, segmentectomy, and lobectomy, respectively. The presence of air bubbles was observed in 15 patients and was detected when the lung parenchyma was cut (13 patients) or compressed (3 patients) using staplers and when an energy device was used (1 patient). No postoperative organ infarction occurred in any patients.
Conclusions
Although the presence of air bubbles was noted in the pulmonary vein during lung resection via transesophageal echocardiography, the clinical condition of the patients in our study did not deteriorate. The clinical significance of air bubbles is not clear. Therefore, more data about such events must be collected in future.

Similar content being viewed by others
References
Bateman BT, Schumacher HC, Wang S, Shaefi S, Berman MF. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009;110:231–8.
Ohtaka K, Hida Y, Kaga K, Kato T, Muto J, Nakada-Kubota R, et al. Thrombosis in the pulmonary vein stump after left upper lobectomy as a possible cause of cerebral infarction. Ann Thorac Surg. 2013;95:1924–8.
Yamamoto T, Suzuki H, Nagato K, Nakajima T, Iwata T, Yoshida S, et al. Is left upper lobectomy for lung cancer a risk factor for cerebral infarction? Surg Today. 2016;46:780–4.
Tomiyama N, Yasuhara Y, Nakajima Y, Adachi S, Arai Y, Kusumoto M, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol. 2006;59:60–4.
Nakano T, Shimizu K, Otani Y, Kakegawa S, Morishita Y, Taketoshi I. Cerebral air embolism complicating computed tomography-guided percutaneous needle biopsy of the lung: a case report with effective hyperbaric oxygen therapy. Jpn J Chest Surg. 2007;21:859–64.
Matsuura Y, Watari M. Two cases of air bubble in intracardiac cavity after computed tomography-guided lung puncture. Jpn J Chest Surg. 2010;24:967–71.
Sakiyama S, Kondo K, Matsuoka H, Yoshida M, Miyoshi T, Yoshida S, et al. Fatal air embolism during computed tomography-guided pulmonary marking with a hook-type marker. J Thorac Cardiovasc Surg. 2003;126:1207–9.
Sinner WN. Complications of percutaneous transthoracic needle aspiration biopsy. Acta Radiol Diagn. 1976;17:813–28. (Stockh)
Richardson CM, Pointon KS, Manhire AR, Macfarlane JT. Percutaneous lung biopsies: a survey of UK practice based on 5444 biopsies. Br J Radiol. 2002;75:731–5.
Yamashita Y, Mukaida H, Hirabayashi N, Takiyama W. Cerebral air embolism after intrathoracic anti-cancer drug administration. Ann Thorac Surg. 2006;82:1121–3.
Menendez-Gonzalez M, Oliva-Nacarino P, Alvarez-Cofino A. Cerebral gas embolism caused by pleural fibrinolytic treatment. Stroke. 2007;38:2602–4.
Schneider F, Lion R, Kummerlen C, Ducrocq X, Tempe JD. Neurological complications and pleural lavage with a fibrinolytic agent. A two-case report. Intensive Care Med. 2000;26:995–7.
Ohuchi M, Inoue S, Ozaki Y, Ueda K. Systemic air embolism during pleural lavage for empyema. Gen Thorac Cardiovasc Surg. 2017;65:602–4.
Saada M, Goarin JP, Riou B, Rouby JJ, Jacquens Y, Guesde R, et al. Systemic gas embolism complicating pulmonary contusion. Diagnosis and management using transesophageal echocardiography. Am J Respir Crit Care Med. 1995;152:812–5.
Shaikh N, Ummunisa F. Acute management of vascular air embolism. J Emerg Trauma Shock. 2009;2:180–5.
Hemmerling TM, Schmidt J, Bosert C, Klein P. Systemic air embolism during wedge resection of the lung. Anesth Analg. 2001;93:1135–6.
Kawaguchi K, Usami N, Taniguchi T, Ishikawa Y, Fukui T, Yokoi K. Systemic air embolism during double sleeve left upper lobectomy: caution regarding this fatal complication. Jpn J Chest Surg. 2013;27:472–6.
Yuki D, Kawano O, Fukai I. Systemic air embolism during wedge resection of the lung: Report of a case. Jpn J Chest Surg. 2015;29:798–802.
Funding
This study was not supported by a sponsor or funding agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
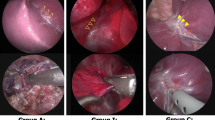
Video 1: We identified air bubbles during transesophageal echocardiography when the lung parenchyma was cut. The patient in this figure is the same as the one in Fig. 1. (MPG 7066 KB)
Rights and permissions
About this article
Cite this article
Nakahashi, K., Oizumi, H., Suzuki, J. et al. Influx of air into the left atrium during lung resection. Gen Thorac Cardiovasc Surg 67, 880–883 (2019). https://doi.org/10.1007/s11748-019-01112-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01112-8