Abstract
Objectives
To detect metastatic lung tumors of less than 1 mm in size by focusing on the clearance of contrast material using synchrotron radiation (SR) angiography characterized by high spatial resolution and high-sensitivity receiver.
Methods
C6 cells, derived from rat glioma cells, were injected to the rat tail vein. Two weeks after injection, the rats underwent SR angiography using a high-gain avalanche rushing amorphous photoconductor (HARP) receiver of extra-high sensitivity with high contrast resolution. The 256-grayscale value was employed in the analysis of images.
Results
19 nodules were identified in images. The tumors were confirmed histopathologically. The average tumor size was 621 ± 193 µm. The clearance curve of the densities was expressed as a logarithm function. Tumors showed delayed clearance of contrast material, taking up to 28 s, compared with arteries, which cleared rapidly at 8 s. In 256 grayscale, the distance was 50. This gap in density clearance made it possible to identify tumors.
Conclusions
SR angiography with a HARP receiver provides high sensitivity and spatial resolution and makes it possible to diagnose metastatic lung tumors of less than 1 mm in size by focusing on differences in the clearance times of contrast material.




Similar content being viewed by others
References
Smith RA, Cokkinides V. American cancer society guidelines for the detection of cancer. CA Cancer. 2002;52:8–22.
Deppermann KM. Lung cancer screening-where we are in 2004. Lung Cancer. 2004;45:S39–42.
McDonald DM, Choyke PL. Imaging of angiogenesis: from microscope to clinic. Nat Med. 2003;9:713–25.
Koh DM, Cook GJ, Husband JE. New horizons in oncologic imaging. N Engl J Med. 2003;348:2487–8.
Battista G, Sassi C, Zompatori M, Palmarini D, Canini R. Ground-glass opacity: interpretation of high resolution CT findings. Radiol Med. 2003;106:425–44.
Hannahan D, Wein berg RA. The hallmarks of cancer. Cell. 2000;100:57–70.
Folkman J. Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat Med. 1995;1:27–31.
Leggett DAC, Kelley BB, Bunce IH, Miles KA. Colorectal cancer: diagnostic potential of CT measurements of hepatic perfusion and implications for contrast enhancement protocols. Radiology. 1997;205:716–20.
Kuszyk BS, Corl FM, Franano FN, Bluemke DA, Hofmann LV, Fortman BJ, et al. Tumor transport physiology: implications for imaging and imaging-guided therapy. AJR. 2001;177:747–53.
Gossmann A, Okuhata Y, Shames DM, Helbich TH, Roberts TP, Wendland MF, et al. Prostate cancer tumor grade differentiation with dynamic contrast-enhanced MR imaging in the rat: comparison of macromolecular and small-molecular contrast media—preliminary experience. Radiology. 1999;213:265–72.
Kuszyk BS, Boitnott JK, Choti MA, Bluemke DA, Sheth S, Magee CA, et al. Local tumor recurrence following hepatic cryoablation: radiologic–histologic correlation in an animal model. Radiology. 2000;217:477–86.
Schwenke DO, Pearson JT, Umetani K, Kangawa K, Shirai M. Imaging of the pulmonary circulation in the closed-chest rat using synchrotron radiation microangiography. J Appl Physiol. 2007;102:787–93.
Ikura H, Shimizu K, Ikezoe J, Nagareda T, Yagi N. In vitro evaluation of normal and abnormal lungs with ultra-high-resolution CT. J Thorac Imaging. 2004;19:8–15.
Bayat S, Porra L, Suhonen H, Nemoz C, Suortti P, Sovijärvi AR. Differences in the time course of proximal and distal airway response to inhaled histamine studied by synchrotron radiation CT. J Appl Physiol. 2006;100:1964–73.
Kono M, Ohbayashi C, Yamasaki K, Ohno Y, Adachi S, Sugimura K, et al. Refraction imaging and histologic correlation in excised tissue from a normal human lung: preliminary report. Acad Radiol. 2001;8:898–902.
Konishi T, Matsushita S, Hyodo K, Sato F, Hiramatsu Y, Sakakibara Y. Examination of a new angiographic system that utilizes a highly sensitive receiver and synchrotron radiation for reducing the dose of contrast medium. Am J Roentgenol. 2011;197:W508–13.
Tanioka K, Matsubara T, Ohkawa Y, Miyakawa K, Suzuki S, Takahata T, et al. Ultra-high-sensitivity new super-HARP pickup tube and its camera. IEICE Trans Electron. 2003;E86-C(9):1790–5.
Matsushita S, Hyodo K, Imazuru T, Tokunaga C, Sato F, Enomoto Y, et al. The minimum coronary artery diameter in which coronary spasm can be identified by synchrotron radiation coronary angiography. Eur J Radiol. 2008;68:S84–8.
Mandybur TI, Liwnicz BH, Wechsler W. Disseminated (metastatic) tumors in nude mice produced by intravenous injection of cells of human and nonhuman neurogenic tumor lines. Acta Neuropathol. 1984;63:203–9.
Arfelli F. Synchrotron light and imaging systems for medical radiology. Nucl Instrum Methods Phys Res A. 2000;454:11–25.
Miyakawa K, Ohkawa Y, Matsubara T, Kikuchi K, Suzuki S, Tanioka K, et al. Development of FOP-HARP imaging device. Sensors, cameras, and systems for industrial/scientific applications XI SPIE-IS&T. 2010; 7536:753604-1-8.
Meuli R, Hwu Y, Je JH, Margaritondo G. Synchrotron radiation in radiology: radiology techniques based on synchrotron sources. Eur Radiol. 2004;14:1550–60.
Carmeliet P, Jain RK. Angiogenesis in cancer and other disease. Nature. 2000;407:249–57.
Fink C, Kiessling F, Bock M, Lichy MP, Misselwitz B, Peschke P, et al. High-resolution three-dimensional MR angiography of rodent tumors. J Magn Reson Imaging. 2003;18:59–65.
Helmlinger G, Yuan F, Dellian M, Jain RK. Interstitial pH and pO2 gradients in solid tumors in vivo: high-resolution measurements reveal a lack of correlation. Nat Med. 1997;3:177–82.
Furuya M, Yonemitsu Y. Cancer neovascularization and proinflammatory microenvironments. Curr Cancer Drug Targets. 2008;8:253–65.
Hida K, Hida Y, Amin DN, Flint AF, Panigrahy D, Morton CC, et al. Tumor-associated endothelial cells with cytogenetic abnormalities. Cancer Res. 2004;64:8249–55.
Gerlowski LE, Jain RK. Microvascular permeability of normal and neoplastic tissues. Microvasc Res. 1986;31:288–305.
Roberts HC, Roberts TP, Brasch RC, Dillon WP. Quantitative measurement of microvascular permeability in human brain tumors achieved using dynamic contrast-enhanced MR imaging: correlation with histologic grade. AJNR Am J Neuroradiol. 2000;21:891–9.
Cuenod CA, Fournier L, Balvay D, Guinebretiere JM. Tumor angiogenesis: pathophysiology and implications for contrast-enhanced MRI and CT assessment. Abdom Imaging. 2006;31:188–93.
Acknowledgments
The authors thank Mr. Kenkichi Tanioka of Tokyo Denki University, Mr. Misao Kubota, Mr. Kazunori Miyakawa of NHK Science and Technical Research Laboratory and Mr. Akira Kobayashi of Hamamatsu Photonics Corporation for their technical assistance. The authors are grateful to Mr. Avi Landau for his language consultation. This study was supported in part by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (Grant C-20591471 and Grant C-23592053).
Conflict of interest
The authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
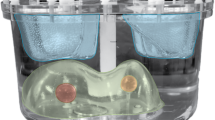
Supplementary material 1 (MPG 6680 kb) Online Resource1. The original animation of SR angiography (the case of Fig. 2). Several nodules were shown with delayed clearance of density from a few seconds after rapid infusion, and some of them remained visible for a few minutes. Their time course of density were analyzed (Fig. 1) using captured still images (Fig. 2)
Rights and permissions
About this article
Cite this article
Ito, H., Matsushita, S., Hyodo, K. et al. Focusing on delayed clearance for identifying small-sized metastatic lung tumors using synchrotron radiation angiography with a highly sensitive receiver. Gen Thorac Cardiovasc Surg 62, 553–559 (2014). https://doi.org/10.1007/s11748-014-0430-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-014-0430-x