Abstract
Monocyte distribution width (MDW) has been associated with inflammation and poor prognosis in various acute diseases. Chronic obstructive pulmonary disease (COPD) exacerbations (ECOPD) are associated with mortality. The objective of this study was to evaluate the utility of the MDW as a predictor of ECOPD prognosis. This retrospective study included patient admissions for ECOPD. Demographic, clinical and biochemical information; intensive care unit (ICU) admissions; and mortality during admission were recorded. A total of 474 admissions were included. MDW was positively correlated with the DECAF score (r = 0.184, p < 0.001) and C-reactive protein (mg/dL) (r = 0.571, p < 0.001), and positively associated with C-RP (OR 1.115 95% CI 1.076–1.155, p < 0.001), death (OR 9.831 95% CI 2.981– 32.417, p < 0.001) and ICU admission (OR 11.204 95% CI 3.173–39.562, p < 0.001). High MDW values were independent risk factors for mortality (HR 3.647, CI 95% 1.313–10.136, p = 0.013), ICU admission (HR 2.550, CI 95% 1.131–5.753, p = 0.024), or either mortality or ICU admission (HR 3.084, CI 95% 1.624–5.858, p = 0.001). In ROC analysis, a combined MDW–DECAF score had better diagnostic power (AUC 0.777 95% IC 0.708–0.845, p < 0.001) than DECAF (p = 0.023), MDW (p = 0.026) or C-RP (p = 0.002) alone. MDW is associated with ECOPD severity and predicts mortality and ICU admission with a diagnostic accuracy similar to that of DECAF and C-RP. The MDW– DECAF score has better diagnostic accuracy than MDW or DECAF alone in identifying mortality or ICU admission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide [1]. COPD exacerbation (ECOPD) is a major outcome of this disease and ECOPD severity is associated with future mortality risk [2], a decline in FEV1 [3], diminished quality of life [4] and future ECOPD [5, 6]. Moreover, ECOPD hospitalizations are associated with high mortality rates [7, 8]. Nonetheless, few tools are available to help clinicians to determine ECOPD prognosis in hospitalized patients. These tools include C-reactive protein (C-RP), the only biomarker recommended by GOLD [9] to evaluate ECOPD severity, and the dyspnea–eosinopenia–consolidation–acidemia–atrial fibrillation (DECAF) prognostic score, which uses several clinical variables (dyspnea, eosinopenia, consolidation, acidemia and atrial fibrillation) to establish the prognosis of severe ECOPD [10]. Therefore, new parameters must be investigated in clinical practice to determine prognosis in patients with severe ECOPD.
The inflammatory response during ECOPD is mediated by the activation of neutrophilic and lymphocytic inflammation [11]. Circulating neutrophils and monocytes are involved in the initial response to pathogenic organisms that cause ECOPD [12]. Monocyte distribution width (MDW) reflects the degree of change in circulating monocyte volume (“heterogeneity”) in response to proinflammatory signals elicited by infectious organisms. MDW determination is easily automated, inexpensive and quickly obtained as part of routine blood counts. Recent data have suggested that an increase in MDW may be useful in early detection of all-cause sepsis [13,14,15,16,17,18,19,20,21]. However, few studies have been performed in acute respiratory conditions; one example is a study in a limited number of patients with COVID-19 [22,23,24]. Some studies have suggested that MDW may be associated with the neutrophil/lymphocyte ratio, a biomarker associated with ECOPD prognosis [11].
We hypothesized that high MDW at hospital admission might serve as a prognostic inflammatory biomarker in patients with ECOPD and that combining the MDW with the DECAF score might further increase the prognostic value. To our knowledge, this aspect has not previously been studied in this setting.
Methods
This was a multicenter observational retrospective study in which clinical records from patients admitted for ECOPD between March 1st, 2020, and March 1st, 2023, to three public hospitals of the Servicio Cántabro de Salud network in the Cantabria community in northern Spain were reviewed. The ethics committee of our institution (2023.061) approved the study.
Participants
We recruited patients hospitalized for ECOPD between March 2020 and March 2023.
The inclusion criteria were as follows: (1) Patients older than 40 years previously diagnosed with COPD according to the GesEPOC guidelines [25] and (2) Patients hospitalized because of ECOPD. ECOPD was defined by an increase in more than one of the following respiratory symptoms: dyspnea, sputum purulence, increased sputum, cough or wheezing; symptoms persisting for at least 2 consecutive days; and symptoms requiring treatment with antibiotics and/or systemic steroids [9].
The exclusion criteria were as follows: (1) Patients with a diagnosis other than ECOPD at discharge; (2) Patients without clinical, biochemical or microbiological data consistent with ECOPD; (3) Patients with active cancer, leukemia, lymphoma, lymphoproliferative disorders, bone marrow diseases or AIDS; (4) Patients with vitamin B12 or folic acid deficiency; and (5) Patients treated with immunosuppressants (including systemic corticosteroids) or drugs causing macrocytosis.
Measurements
Stable spirometry was performed according to the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR) protocol [26] less than 1 year before admission. Patient age; sex; smoking status; number of moderate and severe ECOPD events 1 year before admission; comorbidities included in the Charlson index [27]; basal mMRC dyspnea score; and dates of hospital admission, ICU admission and/or death during hospitalization were retrospectively recorded. The DECAF score [25] was calculated for all patients. The MDW and results of routine blood tests performed after arrival at the emergency department of each center were retrospectively collected.
Routine hematological and biochemical analytes were measured with automated assays. Specifically, C-RP was measured with Siemens traceable enzymatic method assays (Atellica Analyzer, Siemens, Germany).
MDW was measured in the emergency laboratory of each center with the same DxH 900 analyzer (Beckman Coulter. Inc., Brea, California, USA), according to the manufacturer´s instructions.
Statistical analysis
Data are presented as mean ± SD for normally distributed data or median (interquartile range) for nonparametric data. We calculated sample sizes in Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.), with an α level of 0.05 and a β level of 0.2. Differences between groups were analyzed with unpaired t tests for parametric data or Mann–Whitney tests for nonparametric data. Normality of distribution was evaluated with the Kolmogorov–Smirnov test. We evaluated the correlation between MDW and other variables with Spearman tests. Evaluation of MDW as a dichotomized variable was established with a cutoff at 21.5 units, according to previous studies [28,29,30] performed in the same setting and using similar laboratory protocols as our study. We evaluated cross-sectional associations with high versus low MDW through univariate and multivariate logistic regression, with outcome variables of mortality; ICU admission; and a composite end point including in-hospital all-cause mortality and escalation to ICU admission. We used Kaplan–Meier estimates to calculate the proportion of participants experiencing mortality; ICU admission; and a composite end point including in-hospital all-cause mortality and escalation to ICU admission due to ECOPD over time. We performed univariate and multivariate Cox proportional risk analysis in SPSS version 25.00. A receiver operating characteristic (ROC) curve and the area under the ROC curve (AUC) were used to assess the diagnostic value of MDW for a composite end point including in-hospital all-cause mortality and escalation to ICU admission as the outcome variables. ROC curve analysis was performed in MEDCALC version 11.6.1.0 (MedCalc Software, Mariakerke, Belgium). Differences with p values < 0.05 were considered significant. All reported p values were two sided.
Results
Patient characteristics
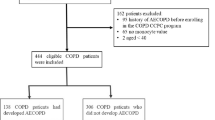
A total of 474 pw ECOPD were ultimately included in the study (flowchart for patient selection in Fig. 1; demographic, clinical and biochemical data in Table 1). The median patient age was 75 (67–82) years, and most patients were men (67.7%). The prevalence of current smokers (32.9%) was high. Most patients had a previous admission for ECOPD [178 (37.6%)] and moderate or severe obstruction, on the basis of FEV1 (%) 50 (35–67). A total of 26 patients died (5.5%); although ICU admission was not frequent [31 (6.5)], a composite end point including mortality or ICU admission reached 11% (52 patients). The blood MDW levels were 19.2 (17.2–21.2) units, the blood leucocyte levels were 9900 (7300–13525) cells/µL and the serum C-RP levels were 4.4 (1.5–11.7) mg/dL.
The group of patients with ECOPD and high MDW tended to have high ECOPD severity, on the basis of the DECAF score, mortality, ICU admission rate and elevated inflammatory parameters, such as C-RP and the neutrophil to lymphocyte ratio. Notably, the group with high MDW had slightly higher FEV1 values. However, the two groups had similar age, sex distribution, smoking habits, basal mMRC scores and ECOPD history.
MDW correlations
MDW was positively correlated with the DECAF score (r = 0.184, p < 0.001), FEV1 (L) (r = 0.153, p = 0.001), FEV1 (% predicted) (r = 0.149, p = 0.001), FEV1/FVC (r = 0.106, p = 0.022), C-RP (mg/dL) (r = 0.571, p < 0.001) and neutrophil to lymphocyte ratio (r = 0.135, p = 0.003).
MDW was negatively correlated with basophil count (r = −0.111, p = 0.016) and eosinophil count (r = −0.288, p < 0.001).
MDW did not correlate with age (r = 0.025, p = 0.588), Charlson score (r = 0.056, p = 0.291), BMI (r = −0.02, p = 0.978), FVC (L) (r = 0.069, p = 0.145), FVC FEV1 (% predicted) (r = 0.077, p = 0.099), paO2 (r = -0.084, p = 0.069), paCO2 (r = −0.088, p = 0.056), HCO3 (r = −0.065, p = 0.173), pH (r = 0.088, p = 0.056), leucocyte count (r = 0.024, p = 0.597), neutrophil count (r = 0.063, p = 0.172), monocyte count (r = 0.050, p = 0.274) or lymphocyte count (r = −0.080, p = 0.081).
Association of MDW with ECOPD characteristics
Table 2 highlights the associations of MDW with baseline ECOPD characteristics. Multivariate logistic regression analysis showed that high MDW was positively associated with C-RP (OR 1.115 95% CI 1.076–1.155, p < 0.001), death (OR 9.831 95% CI 2.981–32.417, p < 0.001) and ICU admission (OR 11.204 95% CI 3.173–39.562, p < 0.001); however, no associations with other ECOPD characteristics were observed.
MDW as a predictor of mortality, ICU admission or both
Among 474 patients with ECOPD included in the study, 109 had a high MDW. Table 1 shows the clinical characteristics of both groups. A total of 26 patients died during hospitalization (18 in the high MDW group), 31 patients were admitted to the ICU (17 in the high MDW group) and 52 patients met the composite end point including mortality or ICU admission (30 in the high MDW group).
Predictors of mortality
Univariate Cox proportional risk analysis indicated that age (p = 0.04), sex (women) (p = 0.292), MDW (p = 0.001) and high MDW (higher than 21.5) (p = 0.002), but not smoking status (p = 0.064), FEV1 (p = 0.626), Charlson index (p = 0.101), DECAF score (p = 0.069), C-RP (p = 0.127) or neutrophil to lymphocyte ratio (p = 0.416) were predictors of mortality during hospitalization due to ECOPD. Multivariate Cox proportional risk analysis revealed that the absolute values of MDW (HR 1.171, CI 95% 1.073–1.277, p < 0.001) (Table 3) and high MDW (HR 3.647, CI 95% 1.313–10.136, p = 0.013) (Table 3, Fig. 2) were independent risk factors for mortality during hospitalization for ECOPD.
Predictors of ICU admission
Univariate Cox proportional risk analysis indicated that age (p < 0.001), smoking status (p = 0.007), DECAF score (p < 0.001), C-RP (p = 0.002), MDW (p < 0.001) and high MDW (higher than 21.5) (p < 0.001), but not sex (p = 0.292), FEV1 (p = 0.802), Charlson index (p = 0.995) or neutrophil to lymphocyte ratio (p = 0.654) were predictors of ICU admission. Multivariate Cox proportional risk analysis revealed that absolute values of MDW (HR 1.086, CI 95% 1.009–1.169, p = 0.027) (Table 3) and high MDW (HR 2.550, CI 95% 1.131–5.753, p = 0.024) (Table 3, Fig. 2) were independent risk factors for ICU admission.
Predictors of the composite end point (mortality or ICU admission)
Univariate Cox proportional risk analysis indicated that age (p = 0.047), DECAF score (p < 0.001), C-RP (p < 0.001), MDW (p < 0.001) and high MDW (higher than 21.5) (p < 0.001), but not smoking status (p = 0.072), sex (p = 0.767), FEV1 (p = 0.786), Charlson index (p = 0.100) or neutrophil to lymphocyte ratio (p = 0.754) were predictors of the composite end point (mortality or ICU admission). Multivariate Cox proportional risk analysis revealed that absolute values of MDW (HR 1.122, CI 95% 1.065–1.182, p < 0.001) (Table 3) and high MDW (HR 3.084, CI 95% 1.624–5.858, p = 0.001) (Table 3, Fig. 2) were independent risk factors for the composite end point (mortality or ICU admission).
Potential utility of the MDW and DECAF–MDW score in predicting the composite end point
According to our findings, we created a new tool, the MDW–DECAF score, based on the DECAF score and including the same variables as DECAF and the MDW, with a relative weight assigned according to the regression coefficient for the composite end point (3 points). In ROC analysis (Fig. 3), the MDW–DECAF score’s AUC for differentiating patients who died or were admitted to the ICU from the rest of the patients (AUC 0.777 95% IC 0.708–0.845, p < 0.001) had the best diagnostic power and was followed by the DECAF score (AUC 0.710 95% IC 0.639–0.782, p < 0.001) and MDW (AUC 0.705 95% IC 0.618–0.791, p < 0.001) (Fig. 3, Supplementary file 1). Youden’s index for MDW was > 21.7, with a sensitivity of 57.69 and a specificity of 81.95. Youden’s index for the MDW–DECAF score was > 2, with a sensitivity of 84.62 and a specificity of 63.01. MDW–DECAF had a statistically significantly higher AUC than the DECAF score (p = 0.023), MDW (p = 0.026), C-RP (p = 0.002) and neutrophil to lymphocyte ratio. No statistically significant differences were found among the AUC values of the remaining variables.
Receiver operator characteristic curve showing the discrimination ability of MDW, C-reactive protein, neutrophil to lymphocyte ratio, the DECAF score and the MDW–DECAF score for in-hospital mortality or ICU admission. MDW monocyte distribution width, DECAF dyspnea, eosinopenia, consolidation, acidemia and atrial fibrillation score
Discussion
This study provides the first demonstration that MDW is associated with the severity of severe ECOPD and can be used as a predictor of mortality and ICU admission. Moreover, it introduces the new MDW–DECAF score.
Patients with high MDW, as reported by previous studies in patients with systemic inflammatory response syndrome [28, 29] or COVID-19 [30], had elevated C-RP, DECAF scores and neutrophil to lymphocyte ratios, and lower blood eosinophils; these prognostic factors are well known to be associated with both ECOPD inflammatory response and severity [10, 11, 31,32,33]. We also evaluated variables associated with higher MDW values in a multivariate logistic regression analysis, which indicated that C-RP, mortality and ICU admission were associated with high MDW values. Our findings indicate the importance of inflammation in MDW levels, as discussed in other clinical contexts, such as sepsis [16, 19, 20, 24, 28, 29], COVID-19 [22,23,24], influenza [34] and complicated diverticulitis [35].
Our findings provide the first evidence that the MDW values according to blood tests performed after emergency department arrival predict death and ICU admission for ECOPD. This novel finding has not previously been described in the context of COPD, but has been reported in other settings, such as COVID-19 [23] and sepsis [28]. Furthermore, our results were obtained by using Cox regression analysis considering the time to the event, whereas other studies have evaluated ECOPD prognosis by using only logistic regression analysis [10, 11]. Additionally, the cutoff point of the test was determined on the basis of previous studies [28,29,30]. This was similar to Youden’s index in our study.
The AUC of MDW for predicting the prognosis of severe ECOPD in terms of mortality or ICU admission was comparable to that of other well-known inflammatory markers of COPD, such as C-RP [9] or the neutrophil to lymphocyte ratio [11]. MDW is biomarker that can be routinely measured rapidly, easily and inexpensively in emergency departments. Further studies are necessary to evaluate the limitations and benefits of each biomarker in COPD. The DECAF score [10] is a well-known risk stratification tool for patients with severe ECOPD, but its AUC can be improved by using novel biomarkers. Because MDW is a different predictor from the DECAF score for mortality or ICU admission, we created a new score, the MDW–DECAF score, which had a better AUC than the other biomarkers or the DECAF score alone. Further studies are required to evaluate the potential roles of these scores in assessing specific etiologies of ECOPD or inflammatory conditions.
This study has several strengths. First, it is a novel study reporting the first evaluation of MDW in ECOPD in real-world circumstances. Second, this was a multicenter study in patients from three hospitals. Finally, the patients included in this study were carefully selected and well characterized, and patients with diseases or therapies that might have influenced the results were excluded.
However, our study also has several limitations. First, this was a retrospective study and therefore was subject to a risk of information bias. Although all routine blood tests were performed minutes after arrival at the emergency department, the retrospective nature of this study could imply different timing for analysis from whole blood venous sample collection. Furthermore, our results cannot be extrapolated to all patients with COPD since we excluded patients with hematological and nutritional conditions. Our findings should be replicated in other settings, in a larger number of patients, with standardized therapy and multiple samples, to evaluate the time course of the responses of MDW. Future specifically designed prospective studies should be performed to evaluate the utility of MDW and externally validate MDW–DECAF.
Conclusion
Our study provides the first evidence that MDW is associated with ECOPD severity and predicts mortality and ICU admission with a diagnostic accuracy similar to that of DECAF and C-RP. Furthermore, on the basis of our results, we created a new tool, the MDW–DECAF score, which has better diagnostic accuracy than the DECAF score in identifying mortality or ICU admission.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
GBD Chronic Respiratory Disease Collaborators (2020) Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet Respir Med 8:585–596
Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R (2005) Severe acute exacerbations, and mortality in patients with chronic obstructive pulmonary disease. Thorax 60:925–931
Dransfield MT, Kunisaki KM, Strand MJ, Anzueto A, Bhatt SP, Bowler RP, Criner GJ, Curtis JL, Hanania NA, Nath H, Putcha N, Roark SE, Wan ES, Washko GR, Wells JM, Wendt CH, Make BJ, COPDGene Investigators (2017) Acute exacerbations and lung function loss in smokers with and without chronic obstructive pulmonary disease. Am J Respir Crit Care Med 195:324–330
Spencer S, Jones PW, GLOBE Study Group (2003) Time course of recovery of health status following an infective exacerbation of chronic bronchitis. Thorax 58:589–593
Suissa S, Dell’Aniello S, Ernst P (2012) Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax 67:957–963
Jacobs DM, Noyes K, Zhao J, Gibson W, Murphy TF, Sethi S, Ochs-Balcom HM (2018) Early hospital readmissions after an acute exacerbation of chronic obstructive pulmonary disease in the nationwide readmissions database. Ann Am Thorac Soc 15:837–845
Connors AF, Dawson NV, Thomas C et al (1996) Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (study to understand prognoses and preferences for outcomes and risks of treatments). Am J Respir Crit Care 154:959–967
Gunen H, Hacievliyagil SS, Kosar F et al (2005) Factors affecting survival of hospitalised patients with COPD. Eur Respir J 26:234–241
GOLD (2023) Global initiative for chronic obstructive lung disease. GOLD, Fontana
Steer J, Gibson J, Bourke SC (2012) The DECAF score: predicting hospital mortality in exacerbations of chronic obstructive pulmonary disease. Thorax 67:970–976
Lu FY, Chen R, Li N, Sun XW, Zhou M, Li QY, Guo Y (2021) Neutrophil-to-lymphocyte ratio predicts clinical outcome of severe acute exacerbation of COPD in frequent exacerbators. Int J Chron Obstruct Pulmon Dis 17(16):341–349
Yang J, Qiao M, Li Y, Hu G, Song C, Xue L, Bai H, Yang J, Yang X (2018) Expansion of a population of large monocytes (atypical monocytes) in peripheral blood of patients with acute exacerbations of chronic obstructive pulmonary diseases. Mediators Inflamm 2018:9031452
Dilmoula A, Kassengera Z, Turkan H (2011) Volume, conductivity, and scatter properties of leukocytes (VCS technology) in detecting sepsis in critically ill adult patients. Blood 118:4729
Celik IH, Demirel G, Askoy HT (2012) Automated determination of neutrophil VCS parameters in diagnosis and treatment efficacy of neonatal sepsis. Pediatr Res 71:121–125
Bhargava M, Saluja S, Sindhuri U, Saraf A, Sharma P (2014) Elevated mean neutrophil volume + CRP is a highly sensitive and specific predictor of neonatal sepsis. Int J Lab Hematol 36:e11–e14
Lee AJ, Kim SG (2013) Mean cell volumes of neutrophils and monocytes are promising markers of sepsis in elderly patients. Blood Res 48:193–197
Chaves F, Tierno B, Xu D (2005) Quantitative determination of neutrophil VCS parameters by the coulter automated hematology analyzer: new and reliable indicators for acute bacterial infection. Am J Clin Pathol 124:440–444
Chaves F, Tierno B, Xu D (2006) Neutrophil volume distribution width: a new automated hematologic parameter for acute infection. Arch Pathol Lab Med 130:378–380
Mardi D, Fwity B, Lobmann R, Ambrosch A (2010) Mean cell volume of neutrophils and monocytes compared with C-reactive protein, interleukin-6, and white blood cell count for prediction of sepsis and nonsystemic bacterial infections. Int J Lab Hematol 32:410–418
Crouser ED, Parrillo JE, Seymour C, Angus DC, Bicking K, Tejidor L, Magari R, Careaga D, Williams J, Closser DR, Samoszuk M, Herren L, Robart E, Chaves F (2017) Improved early detection of sepsis in the ED with a novel monocyte distribution width biomarker. Chest 152:518–526
Lippi G, Sanchis-Gomar F, Henry BM (2021) Pooled analysis of monocyte distribution width in subjects with SARS-CoV-2 infection. Int J Lab Hematol 43:O161–O163
Lin HA, Lin SF, Chang HW, Lee YJ, Chen RJ, Hou SK (2020) Clinical impact of monocyte distribution width and neutrophil-to-lymphocyte ratio for distinguishing COVID-19 and influenza from other upper respiratory tract infections: a pilot study. PLoS ONE 15:e0241262
Lorubbio M, Tacconi D, Iannelli G, Feri M, Scala R, Montemerani S, Mandò M, Ognibene A (2022) The role of monocyte distribution width (MDW) in the prognosis and monitoring of COVID-19 patients. Clin Biochem 103:29–31
Alsuwaidi L, Al Heialy S, Shaikh N, Al Najjar F, Seliem R, Han A, Hachim M (2022) Monocyte distribution width as a novel sepsis indicator in COVID-19 patients. BMC Infect Dis 22:27
Miravitlles M, Calle M, Molina J, Almagro P, Gómez JT, Trigueros JA et al (2022) Spanish COPD guidelines (GesEPOC) 2021: updated pharmacological treatment of stable COPD. Arch Bronconeumol 58:69–81
García-Río F, Calle M, Burgos F, Casan P, Del Campo F, Galdiz JB, Giner J, González-Mangado N, Ortega F, Puente ML (2013) Spanish society of pulmonology and thoracic surgery (SEPAR) spirometry. Arch Bronconeumol 49:388–401
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Wu J, Li L, Luo J (2022) Diagnostic, and prognostic value of monocyte distribution width in sepsis. J Inflamm Res 15:4107–4117
Hausfater P, Robert Boter N, Morales Indiano C, Cancella de Abreu M, Marin AM, Pernet J et al (2021) Monocyte distribution width (MDW) performance as an early sepsis indicator in the emergency department: comparison with CRP and procalcitonin in a multicenter international European prospective study. Crit Care 25:227
Wakamatsu K, Nagasawa Z, Katsuki K, Kumazoe H, Yasuda M, Kawamoto S, Kawamura A, Ueno T, Kiyotani R, Fukui I, Maki S, Nagata N, Kawasaki M, Yamada H (2023) Retrospective study on the efficacy of monocyte distribution width (MDW) as a screening test for COVID-19. Eur J Med Res 28:136
Stolz D, Christ-Crain M, Morgenthaler NG, Leuppi J, Miedinger D, Bingisser R, Müller C, Struck J, Müller B, Tamm M (2007) Copeptin, C-reactive protein, and procalcitonin as prognostic biomarkers in acute exacerbation of COPD. Chest 131:1058–1067
Antonescu-Turcu AL, Tomic R (2009) C-reactive protein and copeptin: prognostic predictors in chronic obstructive pulmonary disease exacerbations. Curr Opin Pulm Med 15:120–125
de Torres JP, Cordoba-Lanus E, López-Aguilar C, Muros de Fuentes M, Montejo de Garcini A, Aguirre-Jaime A, Celli BR, Casanova C (2006) C-reactive protein levels and clinically important predictive outcomes in stable COPD patients. Eur Respir J 2006(27):902–907
Badaki-Makun O, Levin S, Debraine A, Hernried B, Malinovska A, Smith A, Toerper M, Fenstermacher KZJ, Cottle T, Latallo M, Rothman RE, Hinson JS (2022) Monocyte distribution width as a pragmatic screen for SARS-CoV-2 or influenza infection. Sci Rep 12:21528
Chang CY, Hsu TY, He GY, Shih HM, Wu SH, Huang FW, Chen PC, Tsai WC (2023) Utility of monocyte distribution width in the differential diagnosis between simple and complicated diverticulitis: a retrospective cohort study. BMC Gastroenterol 23:96
Acknowledgements
We want to particularly acknowledge the patients involved in this study.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This study was funded by Sociedad Castellanoleonesa y Cántabra de patología respiratoria (SOCALPAR).
Author information
Authors and Affiliations
Contributions
Guarantor of the paper: CAA, CG. Conceptualization: CAA, JSO, GA, AM. Data curation: CG, JSO, GA, MRI, RP, LG, SG, LH, JZ, PD, PA, CP, AM Formal analysis: CAA, CG. Project administration: CAA, CG, GA. Methodology: CAA, GA, JSO, AM, MJM. Resources: CAA, JSO, GA, MRI, RP, LG, SG, LH, JZ, PD, PA, CP, AM. Visualization: CAA CG, GA, AM, JSO. Supervision: CAA, AM, GA. Software: CAA, CG. Writing—original draft: CAA, PM, BJL. Writing—review and editing: CAA, CG, AM, GA, JSO.
Corresponding authors
Ethics declarations
Conflict of interest
Carlos Amado has received speaker or consulting fees from Boehringer Ingelheim, Pfizer, AstraZeneca, Novartis, Chiesi, Faes Farma, Esteve and GSK. Guido Andretta has received speaker fees from AstraZeneca. Javier Zuazaga has received speaker fees from Boehringer Ingelheim. The rest of the authors do not have any conflict of interest.
Ethical statement
This study complies with internationally accepted standards for research practice and reporting. The ethics committee of our Institution approved the study (2023.061).
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amado, C.A., Ghadban, C., Manrique, A. et al. Monocyte distribution width (MDW) and DECAF: two simple tools to determine the prognosis of severe COPD exacerbation. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03632-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03632-5