Abstract
Patient safety is a significant concern worldwide. The Emergency Departments (EDs) are vulnerable to adverse events. Europe, with its diverse healthcare systems, differs in patient safety. This study aimed to identify safety challenges through a comparative analysis of healthcare professionals’ perceptions of patient safety in European EDs. In early 2023, a validated questionnaire was distributed to European ED professionals, meeting specific response rate criteria. The questionnaire included five safety domains and additional questions about infection control and team morale, with 36 ordinal scale questions. Responses ranged in five levels from “Never” to “Always,” and the scores were summed to calculate the total safety score (TSS). The study examined the impact of per capita healthcare expenditure on safety perceptions using descriptive statistics, correlation assessments and SPSS 17 used for the analysis. The analysis of 1048 valid responses from 24 European countries revealed significant variability in safety perceptions. Teamwork scored highest, signifying effective collaboration. Common safety issues included overcrowding, patient flow management, understaffing, limited training and facilities for mental illnesses. TSS showed correlation with team morale and infection control, but no correlation with per capita healthcare expenditure. This comparative study underlines the disparities in patient safety perceptions across European EDs. Each country displayed unique safety concerns. Safety perceptions did not align with per capita healthcare expenditure, indicating that addressing ED safety needs multifaceted strategies. Policymakers can leverage these findings to inform strategic planning, encouraging targeted interventions to enhance patient safety at both the national and European levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization calls for patient safety to be recognized as a health priority in national health policies and programs [1]. Patient harm from unsafe care is a significant and growing public health concern globally, contributing substantially to mortality and disability rates worldwide [2,3,4,5], including Europe [6]. In high-income countries, clinical waste accounts for up to 15% of hospital spending due to safety failures [1]. The cost associated with medication errors has been estimated at $42 billion USD annually globally, excluding lost wages and productivity or increased healthcare costs [7]. The costs related to adverse events in European hospitals vary between 1.3 and 32% of public health expenditure [6].
Significant variations remain between healthcare systems in different European countries, in terms of both quality of care and patient safety [6, 8]. European countries adopt different ways of organizing and financing their healthcare systems; two common models are the public and private healthcare system. They also have different access to care, care processes, and healthcare spending per capita [9]. A considerable part of patient harm, and thus healthcare costs, can be avoided by promoting a culture of safety [6, 10]. Emergency departments (EDs) are at high risk of adverse events that affect patient safety [11,12,13,14]. Rapid patient turnover, overcrowding, and physician inexperience, which are common in EDs, can increase patient mortality [15, 16]. Furthermore, burnout in emergency medicine not only has serious consequences on the well-being of healthcare workers but can also negatively affect the quality and safety of care provided to patients [17, 18]. The effective management of medical emergencies requires robust and well-organized healthcare systems capable of providing timely, appropriate, and safe care to all patients. In early 2023, a validated questionnaire [19] was distributed to healthcare professionals working in EDs to assess their perceptions of safety. The global results have been published elsewhere [20]. This study aimed to conduct a comparative analysis of the results among ED workers in most European countries and highlight the most critical aspects related to safety in each country.
Study design and methods
The researchers designed an observational study based on a cross-sectional online survey. Study participants were healthcare professionals working within the emergency medical services system. The methodology and content of the survey were described in a previous publication [20]. The survey was based on an ED safety questionnaire developed in the USA by Magid et al. [21] and modified and validated by the Royal College of Emergency Medicine [22].
The survey is organized into five different safety domains: teamwork, safety leadership, physical environment and equipment, staff and external team, and organizational factors and informatics, with different items in each domain. Seven questions were added to the infection control and team morale domains; these questions were explored in previous studies in different health settings [23]. Each domain is composed of different independent questions, with a total of 36 ordinal scale questions. Each question is based in an orientated assessment where the respondent can select from five different levels of agreement. The study sample included only European countries in which a response rate of more than one valid response per million habitants or, when this criterion was not met, more than 20 responses per country were obtained. A score was elaborated for each domain by the simple addition of the values of questions using the following ranking, ranging from 1 to 5: Never = 1, Rarely = 2, Sometimes = 3, Usually = 4, and Always = 5 (the inverse ranking was used in the negative questions). Higher scores indicated safer situations. The aggregation of the scores for the five safety domains composed the total safety score (TSS).
The country’s health investment per capita (HIPC) and purchasing power parity (PPP) were used to evaluate the effect of the country’s health investment on professionals’ safety perceptions [24]. The response rate was calculated using the most recent available information about country population [25]. The descriptive analysis was performed using central tendency estimators and confidence intervals (95% CI) distribution, the Wald method, and medians [26]. For a clear comparation of the level of safety in each country, the centralized value of the mean (actual value minus mean value) was calculated for the single safety domain. Correlation analysis was used to estimate the associations among the TSS, team morale and infection control scores, and HIPC; the Pearson correlation coefficient was reported. Statistical significance was set at a p value of < 0.05. SPSS 17 was used for the analysis. The study did not require research and ethics committee review but received approval from the EUSEM board of directors.
Results
The initial survey included 1256 responses from 101 different countries, and 1048 responses were finally included in the present study, representing 24 European countries that met the minimum response rate or response rate per million inhabitants. The number of valid responses per country, the rate per population to calculate the TSS, and the HIPC are represented in Table 1.
The descriptive values of the valid responses for each safety domain are shown in Table 2, including the TSS, team morale, and infection control values.
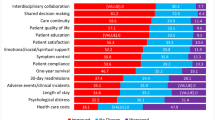
The global responses to the individual questions for each domain are summarized in Table 3, including the descriptors of central tendency and variability. Regarding safety, the mean value of responses to some questions was reassuring, such as “enough monitoring devices” (4.20) and “enough personal protective equipment (PPE)” (4.18), while answers to the questions “number of patients” (2.28) and “interruptions affect care” (2.35) scored lowest. The variability among countries in some response is very low, such as “Doctors and nurses work well together” (0.15) or “Handover creates loss of information” (0.22), indicating a diffuse common feeling about these situations. Conversely, items such as “IT resources availability” (0.60) or the questions in the team morale domain show greater variability, with some values exceeding 0.9.
Differences between countries using the centralized mean values of the different safety domains are shown in Fig. 1.
Safety domains’ score per country—y axis: total domain score, centralized value of the mean; x axis: included countries. MT Malta, IE Ireland, PT Portugal, UK United Kingdom, AL Albania, TR Turkey, HR Croatia, FR France, SE Sweden, IT Italy, SI Slovenia, ES Spain, RO Romania, EL Greece, DE Germany, Denmark DK, Estonia EE, HU Hungary, Finland FI, CH Switzerland, AT Austria, BE Belgium, CZ check, NL Netherland
Full details of the responses for each country in each domain, including the team morale and infection control domains, using the mean values are presented in the Appendix. The Pearson correlation coefficient of the TSS for team morale is 0.63 (p < 0.00) and for infection control is 0.62 (p < 0.00). The correlation coefficient of the TTS for HIPC is 0.142 (p > 0.05) and for PPP is 0.136 (p > 0.05) and are represented in Fig. 2.
Discussion
This study presents a comprehensive assessment of the perception of safety in EDs in 24 European countries. The results highlight the differences between European countries, showing that the TSS of countries is highly variable and indicating that the overall perception of safety is strong in some countries but worrisome in others. However, in each country, there is at least one domain that is more problematic than the others. It is interesting that issues related to safety appear even in wealthy countries with well-functioning healthcare systems.
The countries with higher scores achieved high scores related to the teamwork domain, where the best score was given to “collaboration between nurses and doctors” and “good communication between the team”. Additionally, the availability of monitors and PPE, existence of specific protocols for safe management of patients, and initial assessment and triage were included among the high teamwork scores. These data demonstrate that EDs are well organized and equipped and that the internal organization and competence are strong enough to be considered safe.
The most recurrent safety problems referred to by respondents were overcrowding due to boarding, difficulty in managing patient flow, lack of adequate space, and understaffing (both doctors and nurses). These findings are in line with the European [22, 27,28,29] and international literature [30,31,32], although no study has been conducted on European countries.
Management of patients with mental illnesses represents a problem to emergency medicine professionals. This could be due to both insufficient staff and the lack of a suitable space to maintain and manage patients in a safe environment. Moreover, the lack of training on how to deal with such patients may be a source of unsafety. In recent years, there has been considerable interest in mental health and psychiatric illnesses, partly due to the increasing incidence of these illnesses in Europe, particularly in EDs [33,34,35]. Thus, it is necessary to address this aspect that may exacerbate unsafety and stress among professionals and patients.
The safety domain of organizational factors and informatics, where the questions were related to procedures and support from the hospital and system to ED functioning, seems to be critical and widely heterogeneous among countries. In particular, the procedures for reporting errors are not effective and emergency medicine professionals feel heavy pressure toward external targets, while the hospital may not support ED patient flow and needs. This may be very frustrating and lead to increased burnout and unsafety.
Considering the TSS per country, it is an objective measure of the perception of safety in EDs. Figure 2A, B show the direct correlation between the TSS and the team morale or infection control domain. This means that infection control is a matter of safety concern in EDs [36] and that a safer environment turns into a happier team [37, 38]. A possible suggestion from this observation could be to monitor the TSS over time to measure the impact of safety initiatives and improvements in healthcare systems.
It is noteworthy that safety perceptions in EDs are not closely related to per capita health expenditure, and this is even more evident when the purchasing power of each country is adjusted for, as shown in Fig. 2C, D. This shows that the issue of safety in emergency medicine is quite complex and holds great challenges in Europe, most importantly at the political level. Policymakers and investors are not devoting attention to safety in EDs. On the contrary, there are medium-income countries (e.g., Romania) that have a very high level of safety leadership, physical environment and equipment, and teamwork, demonstrating a marked sensitivity toward emergency medicine safety.
It is evident that each safety aspect in EDs affects the well-being of healthcare workers, reducing burnout and, thus, the rapid turnover of healthcare workers [39]. In addition, safety affects final patient outcomes, reducing the level of mortality and disability and healthcare costs [6].
Healthcare workers and policymakers can use this information to inform strategic planning and decision-making, ultimately leading to improved safety outcomes in emergency medicine in each country and propose European-wide standards.
Limitations
The study has several limitations, including potential bias in survey responses and variations in healthcare systems and cultural contexts across countries. Future research should explore the reasons behind variations in safety perceptions, examine the impact of safety initiatives on patient outcomes, and identify best practices for improving safety in emergency medicine.
Conclusions
The data obtained from the safety questionnaire provide valuable insights into the strengths and areas for improvement within emergency medicine in each European country. To improve safety, healthcare institutions should focus on solving the problems identified in each area. This may involve implementing targeted interventions, improving resource allocation, and promoting a safety culture and open communication between healthcare teams. Regular evaluation and monitoring of safety domains can help identify trends and monitor the effectiveness of safety initiatives over time, ultimately leading to a safer and more efficient emergency medicine environment for both patients and healthcare professionals.
Data sharing
Data are available in the Appendix.
References
Global Patient Safety Action Plan 2021–2030: towards eliminating avoidable harm in health care. World Health Organization (2021). https://www.who.int/teams/integrated-health-services/patient-safety/policy/global-patient-safety. Accessed 15 Nov 2023
Makary MADM (2016) Medical error-the third leading cause of death in the US. BMJ 353:i2139. https://doi.org/10.1136/bmj.i2139
Wang YEN, Metersky ML, Sonnenfeld N et al (2016) Association between hospital performance on patient safety and 30-day mortality and unplanned readmission for Medicare fee-for-service patients with acute myocardial infarction. J Am Heart Assoc 5(7):e003731. https://doi.org/10.1161/JAHA.116.003731
Classen DCM, Munier WM, Verzier NM et al (2021) Measuring patient safety: the Medicare patient safety monitoring system (past, present, and future). J Patient Saf 17(3):e234–e240. https://doi.org/10.1097/PTS.0000000000000322
America. IoMUCoQoHCi (2000) To err is human: building a safer health system. In: Kohn LT, Corrigan JM, Donaldson MS (eds.). National Academies Press (US), Washington, DC
Slawomirski L, Auraaen A, Klazinga N (2017) The economics of patient safety: strengthening a value-based approach to reducing patient harm at national level. OECD Health Working Papers, No. 96, OECD Publishing, Paris, https://doi.org/10.1787/5a9858cd-en
Aitken MGL (2012) Advancing the responsible use of medicines: applying levers for change. Parsippany (NJ), United States of America: IMS Institute for Healthcare Informatics; https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2222541. Accessed 16 June 2023
Krafft T, García Castrillo-Riesgo L, Edwards S et al (2003) European Emergency Data Project (EED Project): EMS data-based health surveillance system. Eur J Pub Health 13(1):85–90. https://doi.org/10.1093/eurpub/13.suppl_1.85
Schneider EC, Shah A, Doty MM et al. ECSe. Mirror, Mirror (2021)—reflecting poorly: health care in the U.S. compared to other high-income countries (Commonwealth Fund, Aug. 2021). https://doi.org/10.26099/01DV-H208
Weaver SJLL, Wilson RF, Pfoh ER et al (2013) Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med 158(5 Pt 2):369–374. https://doi.org/10.7326/0003-4819-158-5-201303051-00002
Ruiz-Ramos J, Santolaya-Perrín R, García-Martín MªÁ, et al. (2021) Prevalence of adverse drug events in emergency departments. FARM-URG multi-center project. Farm Hosp 45(4):176–179. https://doi.org/10.7399/fh.11596. (English)
Eriksson J, Gellerstedt L, Hillerås P et al (2018) Registered nurses’ perceptions of safe care in overcrowded emergency departments. J Clin Nurs 27(5–6):e1061–e1067. https://doi.org/10.1111/jocn.14143
do Nascimento Rocha HM, de Santana Filho VJ (2021) Adverse events in emergency department boarding: a systematic review. J Nurs Scholarsh 53(4):458–467. https://doi.org/10.1111/jnu.12653. (Epub 2021 Mar 31)
Ramlakhan SQH, Burke D, Brown R (2016) The safety of emergency medicine. Emerg Med J 33(4):293–299. https://doi.org/10.1136/emermed-2014-204564. (Epub 2015 Nov 3)
Sprivulis PCDSJ, Jacobs IG, Frazer AR et al (2006) The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 184(5):208–212. https://doi.org/10.5694/j.1326-5377.2006.tb00416.x. (Erratum in: Med J Aust. 2006 Jun 19;184(12):6)
Kwon JHSC, Lee JH, Oh BJ (2016) Efficient utilization of the limited number of emergency medicine specialists and statistics related to clinical outcomes in the emergency department. Clin Exp Emerg Med 3(1):46–51. https://doi.org/10.15441/ceem.15.082
Petrino R, Riesgo LG, Yilmaz B (2022) Burnout in emergency medicine professionals after 2 years of the COVID-19 pandemic: a threat to the healthcare system? Eur J Emerg Med 29(4):279–284. https://doi.org/10.1097/MEJ.0000000000000952. (Epub 2022 Jun 22)
Salyers MPBK, Luther L, Firmin RL et al (2017) The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med 32(4):475–482. https://doi.org/10.1007/s11606-016-3886-9. (Epub 2016 Oct 26)
Magid DJSA, Cleary PD, Rao SR et al (2009) The safety of emergency care systems: results of a survey of clinicians in 65 US emergency departments. Ann Emerg Med 53(6):715–23.e1. https://doi.org/10.1016/j.annemergmed.2008.10.007. (Epub 2008 Dec 3)
Petrino RTE, Bruzzone G, Garcia-Castrillo L (2023) Patient safety in emergency departments: a problem for health care systems? An international survey. Eur J Emerg Med. https://doi.org/10.1097/MEJ.0000000000001044. (Epub ahead of print)
Magid DJ, Sullivan AF, Cleary PD et al (2009) The safety of emergency care systems: results of a survey of clinicians in 65 US emergency departments. Ann Emerg Med 53(6):715–23.e1. https://doi.org/10.1016/j.annemergmed.2008.10.007
Flowerdew L, Tipping M (2021) SECUre: a multicentre survey of the safety of emergency care in UK emergency departments. Emerg Med J 38(10):769–775. https://doi.org/10.1136/emermed-2019-208965
Pronovost PJ, Weast B, Holzmueller CG et al (2003) Evaluation of the culture of safety: survey of clinicians and managers in an academic medical center. Qual Saf Health Care 12(6):405–410. https://doi.org/10.1136/qhc.12.6.405
Health spending per capita, 2020—Country rankings: Global Economy; 2020. https://www.theglobaleconomy.com/rankings/health_spending_per_capita/European-union/. Accessed 15 Nov 2023
European Countries by population (2023): Worldometer; 2023. https://www.worldometers.info/population/countries-in-europe-by-population/. Accessed Sep 2023
Agresti A, Coull BA (1998) Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat 52(2):119–126. https://doi.org/10.1080/00031305.1998.10480550
Ricklin ME, Hess F, Hautz WE (2019) Patient safety culture in a university hospital emergency department in Switzerland—a survey study. GMS J Med Educ 36(2):Doc14. https://doi.org/10.3205/zma001222
Gambashidze N, Hammer A, Brösterhaus M, Manser T, WorkSafeMed Consortium (2017) Evaluation of psychometric properties of the German Hospital Survey on Patient Safety Culture and its potential for cross-cultural comparisons: a cross-sectional study. BMJ Open 7(11):e018366. https://doi.org/10.1136/bmjopen-2017-018366
Jones KJ, Skinner A, Xu L, Sun J, Mueller K (2008) The AHRQ hospital survey on patient safety culture: a tool to plan and evaluate patient safety programs. In: Henriksen K, Battles JB, Keyes MA, Grady ML (eds) Advances in patient safety: new directions and alternative approaches (vol. 2: culture and redesign). Agency for Healthcare Research and Quality (US), Rockville
Croskerry P, Sinclair D (2001) Emergency medicine: a practice prone to error? Can J Emerg Med 3(4):271–276. https://doi.org/10.1017/S1481803500005765
Babatabar-Darzi HJ-II, Mahmoudi H, Ebadi A (2020) Overcrowding management and patient safety: an application of the stabilization model. Iran J Nurs Midwifery Res 25(5):382–386. https://doi.org/10.4103/ijnmr.IJNMR_254_19
Famolaro T, Yount ND, Burns W, Flashner E, Liu H, Sorra J (2016) Agency for Healthcare Research and Quality, Rockville. AHRQ Publication No. 16-00121-EF
Castelpietra GKA, Agardh EE, Armocida B et al (2022) The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990–2019: findings from the Global Burden of Disease Study 2019. Lancet Reg Health Eur 16:100341. https://doi.org/10.1016/j.lanepe.2022.100341
Fitzgerald EFD, McNamara R, Barrett E et al (2020) Trends in mental health presentations to a pediatric emergency department. Ir Med J 113(2):20
Baracaia SMD, Baldwin S, Mytton J et al (2020) Mental health in hospital emergency departments: cross-sectional analysis of attendances in England 2013/2014. Emerg Med J 37(12):744–751. https://doi.org/10.1136/emermed-2019-209105. (Epub 2020 Nov 5)
Gammon JHJ, Williams S, Daniel S et al (2019) Infection prevention control and organisational patient safety culture within the context of isolation: study protocol. BMC Health Serv Res 19(1):296. https://doi.org/10.1186/s12913-019-4126-x
Moreira FTLDS, Albuquerque GA, Oliveira RM (2019) Effective communication strategies for managing disruptive behaviors and promoting patient safety. Rev Gaucha Enferm 40(spe):e20180308. https://doi.org/10.1590/1983-1447.2019.20180308. (Portuguese, English, Epub 2019 Apr 29)
Brennan PAHJ, Oeppen RS (2023) Applying human factors to improve patient safety, morale and team working for oral pathology and medicine specialists. J Oral Pathol Med 52(4):283–287. https://doi.org/10.1111/jop.13404. (Epub 2023 Jan 23)
Hodkinson AZA, Johnson J, Geraghty K et al (2022) Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ 378:e070442. https://doi.org/10.1136/bmj-2022-070442
Funding
Open access funding provided by Università della Svizzera italiana. The expenses for this paper, such as survey distribution and professional writing revision are covered by the European Society for Emergency Medicine (EUSEM).
Author information
Authors and Affiliations
Contributions
RP contributed to the study design, preparation of the survey, paper writing, final revision, and approval. CB contributed to the study design, paper writing, and final approval. LGC contributed to the study design, preparation of the survey, statistical analysis, final revision, and approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare not to have financial or competing interests.
Ethical approval
The protocol did not require approval by an ethics committee but was approved by the board of the EUSEM.
Human and animal rights
This study does not contain any studies with animals performed by any of the authors Informed consent: for this study informed consent is not required (as all the participants gave implicit consent by compiling the survey).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Petrino, R., Biondi, C. & Castrillo, L.G. Healthcare professionals’ perceptions of patient safety in European emergency departments: a comparative analysis of survey results. Intern Emerg Med 19, 1121–1127 (2024). https://doi.org/10.1007/s11739-023-03523-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03523-1