Abstract
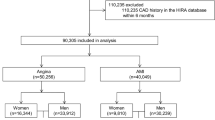
Few studies have assessed sex differences in the management of suspected acute coronary syndrome (ACS). We aimed to compare the evaluation, treatment, and outcomes between males and females with suspected ACS in the emergency department. Data were obtained from a prospective registry of acute chest pain involving 21 emergency departments in Shandong Province, China. The primary endpoint was 30-day major adverse cardiac events (MACEs). Overlap propensity score weighting was used to address potential confounding. A total of 8046 patients were analysed (42.8% female). Overlap-weighted analysis showed no significant association of female sex with 30-day MACEs (odds ratio, 0.91; 95% CI 0.75 to 1.11; P = 0.363). Secondary analyses found that women were less likely to be identified as high risk at first presentation (odds ratio, 0.86; 95% CI 0.78 to 0.94; P < 0.001). In the emergency department, women were less likely to undergo antiplatelet therapy (odds ratio, 0.87; 95% CI 0.79 to 0.96; P = 0.004) or coronary angiography (odds ratio, 0.78; 95% CI, 0.69 to 0.88; P < 0.001). Women had a longer length of stay in the emergency department and were less likely to be admitted to a ward at disposition. These sex differences existed only in the non-ST-elevation subgroup and were independent of risk stratification. Women with non-ST-elevation chest pain in China received suboptimal treatment in the emergency department. However, their clinical outcomes were not significantly different from those of men. Further studies are needed to determine the causes and impacts of these sex differences.


Similar content being viewed by others
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Vos T, Lim SS, Abbafati C et al (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396:1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Zhou M, Wang H, Zeng X et al (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 394:1145–1158. https://doi.org/10.1016/S0140-6736(19)30427-1
Hao Y, Liu J, Liu J et al (2019) Sex differences in in-hospital management and outcomes of patients with acute coronary syndrome. Circulation 139:1776–1785. https://doi.org/10.1161/CIRCULATIONAHA.118.037655
D’Onofrio G, Safdar B, Lichtman JH et al (2015) Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: results from the VIRGO study. Circulation 131:1324–1332. https://doi.org/10.1161/CIRCULATIONAHA.114.012293
Ezekowitz JA, Savu A, Welsh RC, McAlister FA, Goodman SG, Kaul P (2020) Is there a sex gap in surviving an acute coronary syndrome or subsequent development of heart failure? Circulation 142:2231–2239. https://doi.org/10.1161/CIRCULATIONAHA.120.048015
Cenko E, Yoon J, Kedev S et al (2018) Sex differences in outcomes after STEMI: effect modification by treatment strategy and age. JAMA Intern Med 178:632–639. https://doi.org/10.1001/jamainternmed.2018.0514
Redfors B, Angerås O, Råmunddal T et al (2015) Trends in gender differences in cardiac care and outcome after acute myocardial infarction in Western Sweden: a report from the Swedish Web system for enhancement of evidence-based care in heart disease evaluated according to recommended therapies (SWEDEHEART). J Am Heart Assoc 4(7):e001995. https://doi.org/10.1161/JAHA.115.001995
Hollander JE, Than M, Mueller C (2016) State-of-the-art evaluation of emergency department patients presenting with potential acute coronary syndromes. Circulation 134:547–564. https://doi.org/10.1161/CIRCULATIONAHA.116.021886
Collet J-P, Thiele H, Barbato E et al (2021) 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 42:1289–1367. https://doi.org/10.1093/eurheartj/ehaa575
Rosengren A, Smyth A, Rangarajan S et al (2019) Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the prospective urban rural epidemiologic (PURE) study. Lancet Glob Health 7:e748–e760. https://doi.org/10.1016/S2214-109X(19)30045-2
Kamphuis CBM, Turrell G, Giskes K, Mackenbach JP, van Lenthe FJ (2012) Socioeconomic inequalities in cardiovascular mortality and the role of childhood socioeconomic conditions and adulthood risk factors: a prospective cohort study with 17-years of follow up. BMC Public Health 12:1045. https://doi.org/10.1186/1471-2458-12-1045
Vogel B, Acevedo M, Appelman Y et al (2021) The Lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet 397:2385–2438. https://doi.org/10.1016/S0140-6736(21)00684-X
Roth GA, Johnson C, Abajobir A et al (2017) Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol 70:1–25. https://doi.org/10.1016/j.jacc.2017.04.052
Zheng W, Wang J, Xu F et al (2018) Evaluation and management of patients with acute chest pain in China (EMPACT): protocol for a prospective, multicentre registry study. BMJ Open 8:e017872. https://doi.org/10.1136/bmjopen-2017-017872
Li F, Thomas LE, Li F (2019) Addressing extreme propensity scores via the overlap weights. Am J Epidemiol 188:250–257. https://doi.org/10.1093/aje/kwy201
Sarma AA, Braunwald E, Cannon CP et al (2019) Outcomes of women compared with men after non-ST-segment elevation acute coronary syndromes. J Am Coll Cardiol 74:3013–3022. https://doi.org/10.1016/j.jacc.2019.09.065
Berger JS, Elliott L, Gallup D et al (2009) Sex differences in mortality following acute coronary syndromes. JAMA 302:874–882. https://doi.org/10.1001/jama.2009.1227
Du X, Spatz ES, Dreyer RP et al (2016) Sex differences in clinical profiles and quality of care among patients with ST-segment elevation myocardial infarction from 2001 to 2011: insights from the China patient-centered evaluative assessment of cardiac events (PEACE)-retrospective study. J Am Heart Assoc 5:e002157. https://doi.org/10.1161/JAHA.115.002157
Wilkinson C, Bebb O, Dondo TB et al (2019) Sex differences in quality indicator attainment for myocardial infarction: a nationwide cohort study. Heart 105:516–523. https://doi.org/10.1136/heartjnl-2018-313959
Jespersen L, Hvelplund A, Abildstrøm SZ et al (2012) Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 33:734–744. https://doi.org/10.1093/eurheartj/ehr331
Lichtman JH, Leifheit EC, Safdar B et al (2018) Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: evidence from the VIRGO study (variation in recovery: role of gender on outcomes of young AMI Patients). Circulation 137:781–790. https://doi.org/10.1161/CIRCULATIONAHA.117.031650
Haider A, Bengs S, Luu J et al (2020) Sex and gender in cardiovascular medicine: presentation and outcomes of acute coronary syndrome. Eur Heart J 41:1328–1336. https://doi.org/10.1093/eurheartj/ehz898
Fairweather D, Frisancho-Kiss S, Rose NR (2008) Sex differences in autoimmune disease from a pathological perspective. Am J Pathol 173:600–609. https://doi.org/10.2353/ajpath.2008.071008
Vaccarino V, Sullivan S, Hammadah M et al (2018) Mental stress-induced-myocardial ischemia in young patients with recent myocardial infarction: sex differences and mechanisms. Circulation 137:794–805. https://doi.org/10.1161/CIRCULATIONAHA.117.030849
Vitale C, Mendelsohn ME, Rosano GMC (2009) Gender differences in the cardiovascular effect of sex hormones. Nat Rev Cardiol 6:532–542. https://doi.org/10.1038/nrcardio.2009.105
Grandi SM, Filion KB, Yoon S et al (2019) Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications. Circulation 139:1069–1079. https://doi.org/10.1161/CIRCULATIONAHA.118.036748
DeVon HA, Mirzaei S, Zègre-Hemsey J (2020) Typical and atypical symptoms of acute coronary syndrome: time to retire the terms? J Am Heart Assoc 9:e015539. https://doi.org/10.1161/JAHA.119.015539
Mehta LS, Beckie TM, DeVon HA et al (2016) Acute myocardial infarction in women: a scientific statement from the American heart association. Circulation 133:916–947. https://doi.org/10.1161/CIR.0000000000000351
Ghare MI, Chandrasekhar J, Mehran R, Ng V, Grines C, Lansky A (2019) Sex disparities in cardiovascular device evaluations: strategies for recruitment and retention of female patients in clinical device trials. JACC Cardiovasc Interv 12:301–308. https://doi.org/10.1016/j.jcin.2018.10.048
Scott PE, Unger EF, Jenkins MR et al (2018) Participation of women in clinical trials supporting FDA approval of cardiovascular drugs. J Am Coll Cardiol 71:1960–1969. https://doi.org/10.1016/j.jacc.2018.02.070
Alexander KP, Chen AY, Newby LK et al (2006) Sex differences in major bleeding with glycoprotein IIb/IIIa inhibitors: results from the CRUSADE (can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the ACC/AHA guidelines) initiative. Circulation 114:1380–1387. https://doi.org/10.1161/CIRCULATIONAHA.106.620815
Lau ES, Braunwald E, Murphy SA et al (2017) Potent P2Y12 inhibitors in men versus women: a collaborative meta-analysis of randomized trials. J Am Coll Cardiol 69:1549–1559. https://doi.org/10.1016/j.jacc.2017.01.028
Al-Lamee R, Thompson D, Dehbi H-M et al (2018) Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet 391:31–40. https://doi.org/10.1016/S0140-6736(17)32714-9
Schieber AC, Delpierre C, Lepage B et al (2014) Do gender differences affect the doctor-patient interaction during consultations in general practice? Results from the INTERMEDE study. Fam Pract 31(6):706–713. https://doi.org/10.1093/fampra/cmu057
Vafaie M, Hochadel M, Münzel T et al (2020) Guideline-adherence regarding critical time intervals in the German chest pain unit registry. Eur Heart J Acute Cardiovasc Care 9:52–61. https://doi.org/10.1177/2048872618762639
Lee KK, Ferry AV, Anand A et al (2019) Sex-specific thresholds of high-sensitivity troponin in patients with suspected acute coronary syndrome. J Am Coll Cardiol 74:2032–2043. https://doi.org/10.1016/j.jacc.2019.07.082
Cullen L, Greenslade JH, Carlton EW et al (2016) Sex-specific versus overall cut points for a high sensitivity troponin I assay in predicting 1-year outcomes in emergency patients presenting with chest pain. Heart 102:120–126. https://doi.org/10.1136/heartjnl-2015-308506
Pagidipati NJ, Peterson ED (2016) Acute coronary syndromes in women and men. Nat Rev Cardiol 13:471–480. https://doi.org/10.1037/nrcardio.2016.89
Thomas LE, Li F, Pencina MJ (2020) Overlap weighting: a propensity score method that mimics attributes of a randomized clinical trial. JAMA 323:2417–2418. https://doi.org/10.1001/jama.2020.7819
Acknowledgements
The authors thank all participating hospitals for their contributions to the EMPACT registry.
Funding
Study was supported by the National Key R&D Program of China (2020YFC1512700, 2020YFC1512705, 2020YFC1512703, 2022YFC0868600), National Science & Technology Fundamental Resources Investigation Project (2018FY100600, 2018FY100602), Key R&D Program of Shandong Province (2021ZLGX02, 2021SFGC0503), Taishan Pandeng Scholar Program of Shandong Province (tspd20181220), The Interdisciplinary Young Researcher Groups Program of Shandong University (2020QNQT004), Youth Top-Talent Project of National Ten Thousand Talents Plan and Qilu Young Scholar Program, Shandong Provincial Natural Science Foundation (ZR2017PH070).
Author information
Authors and Affiliations
Contributions
YC, FX, and JW had the conception and designed the study. KC, WZ, WS, JM, JP, and CP did the literature search. KC, WZ, JZ, JM, JP, CP, and GW provided critical input to the data collection and interpretation. KC and SW did the statistical analysis. KC drafted the manuscript. YC, FX, JW, and YW reviewed the manuscript. All authors revised the manuscript critically and approved the final version. FX takes responsibility for the integrity of the work as a whole from inception to published article.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the ethics committee of Qilu Hospital of Shandong University.
Research involving human participants and/or animals
Our work does not involve any violation of human and animal rights.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheng, K., Wang, J., Zheng, W. et al. Sex differences in the management of patients with suspected acute coronary syndrome in China. Intern Emerg Med (2023). https://doi.org/10.1007/s11739-023-03494-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-023-03494-3