Abstract
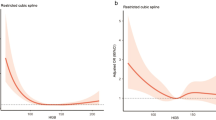
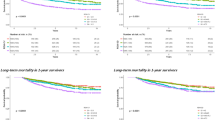
Intracranial hemorrhage (ICH) is a neurological emergency with a poor prognosis. This study aimed to understand the association between hemoglobin levels, red blood cell distribution width ratio (HRR), and mortality in patients with ICH. Information on patients with ICH was extracted from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. Cox proportional risk models were used to assess the relationship between HRR and 28-day and 90-day mortality, and constructed by adjusting for relevant covariates. Segmented regression models and smoothing curves were used to analyze the linear relationship between HRR and mortality. This study recruited 4,716 patients with ICH. The HRR Q4 group was negatively associated with the 28- and 90-day mortality. For patients aged > 65 years, the right-hand threshold inflection points of the HRR were 0.92 and 0.93, respectively, which were negatively associated with 28-day mortality (HR:0.06, 95% CI 0.01, 0.35, p = 0.0016) and with 90-day mortality (p = 0.0006). In the non-linear model, both 28-day mortality (HR, 0.17; 95% CI 0.04–0.75, p = 0.0191; HRR > 0.89) and 90-day mortality (HR, 0.13; 95% CI 0.04–0.49, p = 0.0022; HRR > 0.85) were associated in men. In the subgroup analysis, the negative association between HRR and mortality was more pronounced in patients > 65 years of age, as well as in patients with non-dementia, diabetes, and malignant cancer. We found a non-linear relationship between mortality and the HRR in elderly patients, and a higher HRR was negatively associated with mortality in patients with ICH.



Similar content being viewed by others
Data availability
Data supporting the results of this study are available from the Massachusetts Institute of Technology (MIT) and the Beth Israel Deaconess Medical Center (BIDMC) with restrictions on the availability of these data, which were used with permission in this study and are therefore not publicly available. However, upon reasonable request, the data are available with permission from MIT and BIDMC.
References
Taylor CA, Bell JM, Breiding MJ, Xu L (2017) Traumatic brain injury-related emergency department visits, hospitalizations, and deaths-United States, 2007 and 2013. Morbidity and mortality weekly report. Surveill Summaries (Washington, DC: 2002). 66(9):1–16
Anderson TN, Hwang J, Munar M, Papa L, Hinson HE, Vaughan A et al (2020) Blood-based biomarkers for prediction of intracranial hemorrhage and outcome in patients with moderate or severe traumatic brain injury. J Trauma Acute Care Surg 89(1):80–86
Vos PE, Battistin L, Birbamer G, Gerstenbrand F, Potapov A, Prevec T et al (2002) EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol 9(3):207–219
Nishijima DK, Haukoos JS, Newgard CD, Staudenmayer K, White N, Slattery D et al (2013) Variability of ICU use in adult patients with minor traumatic intracranial hemorrhage. Ann Emerg Med 61(5):509–17.e4
Dadas A, Washington J, Diaz-Arrastia R, Janigro D (2018) Biomarkers in traumatic brain injury (TBI): a review. Neuropsychiatr Dis Treat 14:2989–3000
Maas AIR, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A et al (2017) Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. The Lancet Neurology 16(12):987–1048
Buonora JE, Yarnell AM, Lazarus RC, Mousseau M, Latour LL, Rizoli SB et al (2015) Multivariate analysis of traumatic brain injury: development of an assessment score. Front Neurol 6:68
Li N, Zhou H, Tang Q (2017) Red blood cell distribution width: a novel predictive indicator for cardiovascular and cerebrovascular diseases. Dis Markers 2017:7089493
Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G (2015) Red blood cell distribution width: a simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci 52(2):86–105
Zhou G, Ai Y, Guo S, Chen Q, Feng X, Xu K et al (2021) Association between red blood cell distribution width and thyroid function. Front Endocrinol 12:807482
Long J, Xie X, Xu D, Huang C, Liu Y, Meng X et al (2021) Association between red blood cell distribution width-to-albumin ratio and prognosis of patients with aortic aneurysms. Int J Gener Med 14:6287–6294
Lu C, Long J, Liu H, Xie X, Xu D, Fang X et al (2022) Red blood cell distribution width-to-albumin ratio is associated with all-cause mortality in cancer patients. J Clin Lab Anal 36(5):e24423
Hoff CM (2012) Importance of hemoglobin concentration and its modification for the outcome of head and neck cancer patients treated with radiotherapy. Acta Oncolog (Stockholm, Sweden) 51(4):419–432
Fang Y, Sun X, Zhang L, Xu Y, Zhu W (2022) Hemoglobin/red blood cell distribution width ratio in peripheral blood is positively associated with prognosis of patients with primary hepatocellular carcinoma. Med Sci Monit 28:e937146
Chi G, Lee JJ, Montazerin SM, Marszalek J (2022) Prognostic value of hemoglobin-to-red cell distribution width ratio in cancer: a systematic review and meta-analysis. Biomark Med 16(6):473–482
Giesa N, Heeren P, Klopfenstein S, Flint A, Agha-Mir-Salim L, Poncette A et al (2022) MIMIC-IV as a clinical data schema. Stud Health Technol Inform 294:559–560
Lee CT, Maragkakis M (2021) SamQL: a structured query language and filtering tool for the SAM/BAM file format. BMC Bioinformatics 22(1):474
Han YQ, Yan L, Zhang L, Ouyang PH, Li P, Lippi G et al (2021) Performance of D-dimer for predicting sepsis mortality in the intensive care unit. Biochemia medica 31(2):020709
Guo M, Shu Y, Chen G, Li J, Li F (2022) A real-world pharmacovigilance study of FDA adverse event reporting system (FAERS) events for niraparib. Sci Rep 12(1):20601
Hu ZD, Lippi G, Montagnana M (2020) Diagnostic and prognostic value of red blood cell distribution width in sepsis: A narrative review. Clin Biochem 77:1–6
Fava C, Cattazzo F, Hu ZD, Lippi G, Montagnana M (2019) The role of red blood cell distribution width (RDW) in cardiovascular risk assessment: useful or hype? Ann Transl Med 7(20):581
Zöller B, Melander O, Svensson P, Engström G (2014) Red cell distribution width and risk for venous thromboembolism: a population-based cohort study. Thromb Res 133(3):334–339
Borné Y, Smith JG, Melander O, Engström G (2014) Red cell distribution width in relation to incidence of coronary events and case fatality rates: a population-based cohort study. Heart (British Cardiac Society) 100(14):1119–1124
Pinho J, Silva L, Quintas-Neves M, Marques L, Amorim JM, Reich A et al (2021) Red cell distribution width is associated with 30-day mortality in patients with spontaneous intracerebral hemorrhage. Neurocrit Care 34(3):825–832
Lorente L, Martín MM, González-Rivero AF, Pérez-Cejas A, Sabatel R, Ramos L et al (2020) Red blood cell distribution width and mortality of spontaneous intracerebral hemorrhage patients. Clin Neurol Neurosurg 195:106066
Hou H, Sun T, Li C, Li Y, Guo Z, Wang W et al (2017) An overall and dose-response meta-analysis of red blood cell distribution width and CVD outcomes. Sci Rep 7:43420
Vayá A, Alis R, Hernández JL, Calvo J, Micó L, Romagnoli M et al (2013) RDW in patients with systemic lupus erythematosus. Influence of anaemia and inflammatory markers. Clin Hemorheol Microcirc 54(3):333–339
Zhu H, Wang Z, Yu J, Yang X, He F, Liu Z et al (2019) Role and mechanisms of cytokines in the secondary brain injury after intracerebral hemorrhage. Prog Neurobiol 178:101610
Xiao L, Zheng H, Li J, Wang Q, Sun H (2020) Neuroinflammation mediated by NLRP3 inflammasome after intracerebral hemorrhage and potential therapeutic targets. Mol Neurobiol 57(12):5130–5149
Zahr AA, Salama ME, Carreau N, Tremblay D, Verstovsek S, Mesa R et al (2016) Bone marrow fibrosis in myelofibrosis: pathogenesis, prognosis and targeted strategies. Haematologica 101(6):660–671
Osorio EY, Gugala Z, Patterson GT, Palacios G, Cordova E, Uscanga-Palomeque A et al (2022) Inflammatory stimuli alter bone marrow composition and compromise bone health in the malnourished host. Front Immunol 13:846246
Bommenahalli Gowda S, Gosavi S, Ananda Rao A, Shastry S, Raj SC, Menon S et al (2021) Prognosis of COVID-19: red cell distribution width, platelet distribution width, and C-reactive protein. Cureus 13(2):e13078
Badjatia N, Ryan A, Choi HA, Parikh GY, Jiang X, Day AG et al (2021) Relationship between nutrition intake and outcome after subarachnoid hemorrhage: results from the International Nutritional Survey. J Intensive Care Med 36(10):1141–1148
Rass V, Gaasch M, Kofler M, Schiefecker AJ, Ianosi BA, Steinkohl F et al (2019) Fluid intake but not fluid balance is associated with poor outcome in nontraumatic subarachnoid hemorrhage patients. Crit Care Med 47(7):e555–e562
Bayir A, Ak A, Ozdinç S, Seydanoğlu A, Köstekçi SK, Kara F (2010) Acute-phase vitamin B12 and folic acid levels in patients with ischemic and hemorrhagic stroke: is there a relationship with prognosis? Neurol Res 32(2):115–118
Akpinar I, Sayin MR, Gursoy YC, Aktop Z, Karabag T, Kucuk E et al (2014) Plateletcrit and red cell distribution width are independent predictors of the slow coronary flow phenomenon. J Cardiol 63(2):112–118
Anwar MA, Al Shehabi TS, Eid AH (2016) Inflammogenesis of secondary spinal cord injury. Front Cell Neurosci 10:98
Tutwiler V, Litvinov RI, Lozhkin AP, Peshkova AD, Lebedeva T, Ataullakhanov FI et al (2016) Kinetics and mechanics of clot contraction are governed by the molecular and cellular composition of the blood. Blood 127(1):149–159
Bergström M, Ericson K, Levander B, Svendsen P, Larsson S (1977) Variation with time of the attenuation values of intracranial hematomas. J Comput Assist Tomogr 1(1):57–63
Parizel PM, Makkat S, Van Miert E, Van Goethem JW, van den Hauwe L, De Schepper AM (2001) Intracranial hemorrhage: principles of CT and MRI interpretation. Eur Radiol 11(9):1770–1783
Lu Y, Jin H, Zhao Y, Li Y, Xu J, Tian J et al (2022) Impact of INCREASED HEMOGLOBIN ON SPONTANEOUS INTRACEREBRAL HEMORRHAGE. Neurocrit Care 36(2):395–403
Acosta JN, Leasure AC, Kuohn LR, Both CP, Petersen NH, Sansing LH et al (2021) Admission hemoglobin levels are associated with functional outcome in spontaneous intracerebral hemorrhage. Crit Care Med 49(5):828–837
Nakamura T, Hua Y, Keep RF, Park JW, Xi G, Hoff JT (2005) Estrogen therapy for experimental intracerebral hemorrhage in rats. J Neurosurg 103(1):97–103
Morotti A, Marini S, Lena UK, Crawford K, Schwab K, Kourkoulis C et al (2017) Significance of admission hypoalbuminemia in acute intracerebral hemorrhage. J Neurol 264(5):905–911
Funding
Science and Technology Plan Project of Jiangxi Administration of Traditional Chinese Medicine (No. 2022B952).
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to and agree with the content of the manuscript. Conceptualization: FZ and YX. Methodology: QXL, Software: WHD, JPL, Validation: FZ. Formal Analysis: QXL. Data Curation: WHD. Writing of the original draft: QXL. Writing, Review & Editing: All authors. Visualization: QXL. Supervision: FZ and YX.
Corresponding authors
Ethics declarations
Conflict of interest
This study did not include any research conducted on human or animal participants. The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, Q., Liao, J., Dong, W. et al. The relationship between hemoglobin/red blood cell distribution width ratio and mortality in patients with intracranial hemorrhage: a possible protective effect for the elderly?. Intern Emerg Med 18, 2301–2310 (2023). https://doi.org/10.1007/s11739-023-03431-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-023-03431-4