Abstract
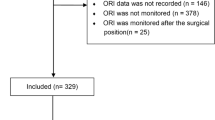
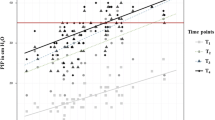
Robot-assisted laparoscopic radical prostatectomy (RALP) has emerged as an effective treatment for prostate cancer with obvious advantages. This study aims to identify risk factors related to hypoxemia during the emergence from anesthesia in patients undergoing RALP. A cohort of 316 patients undergoing RALP was divided into two groups: the hypoxemia group (N = 134) and the non-hypoxemia group (N = 182), based on their postoperative oxygen fraction. Comprehensive data were collected from the hospital information system, including preoperative baseline parameters, intraoperative data, and postoperative recovery profiles. Risk factors were examined using multiple logistic regression analysis. The study showed that 38.9% of patients had low preoperative partial pressure of oxygen (PaO2) levels. Several clinical parameters showed significant differences between the hypoxemia group and the non-hypoxemia group, including weight (P < 0.0001), BMI (P < 0.0001), diabetes mellitus (P = 0.044), history of emphysema and pulmonary alveoli (P < 0.0001), low preoperative PaO2 (P < 0.0001), preoperative white blood cell count (P = 0.012), preoperative albumin (P = 0.048), intraoperative bleeding (P = 0.043), intraoperative CO2 accumulation (P = 0.001), duration of surgery (P = 0.046), postoperative hemoglobin level (P = 0.002), postoperative hypoxemia (P = 0.002), and early postoperative fever (P = 0.006). Multiple logistic regression analysis revealed BMI (adjusted odds ratio = 0.696, 95% confidence interval 0.612–0.719), low preoperative PaO2 (adjusted odds ratio = 9.119, 95% confidence interval 4.834–17.203), and history of emphysema and pulmonary alveoli (adjusted odds ratio = 2.804, 95% confidence interval 1.432–5.491) as independent factors significantly associated with hypoxemia on emergence from anesthesia in patients undergoing RALP. Our results demonstrate that BMI, lower preoperative PaO2, and a history of emphysema and pulmonary alveolar disease are independent risk factors associated with hypoxemia on emergence from anesthesia in patients undergoing RALP. These findings provide a theoretical framework for surgeons and anesthesiologists to facilitate strategies to mitigate postoperative hypoxemia in this unique patient population.
Similar content being viewed by others
Data availability
The datasets utilized and analyzed in the present study are available from the corresponding author upon reasonable request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- ASA:
-
American Society of Anesthesiology
- BGA:
-
Blood gas analysis
- BMI:
-
Body mass index
- CO2 :
-
Carbon dioxide
- Cr:
-
Creatinine
- CRP:
-
C-reactive protein
- DM:
-
Diabetes mellitus
- EtCO2 :
-
End Tidal Volume of Carbon-dioxide
- Hb:
-
Hemoglobin
- ICU:
-
Intensive care unit
- PaCO2 :
-
Pressure of arterial carbon dioxide
- PACU:
-
Post-anesthesia care unit
- PaO2 :
-
Partial pressure of oxygen
- PLT:
-
Platelet
- PPCs:
-
Postoperative pulmonary complications
- RALP:
-
Robot-assisted laparoscopic radical prostatectomy
- WBC:
-
White blood cell
References
Culp MB, Soerjomataram I, Efstathiou JA, Bray F, Jemal A (2020) Recent global patterns in prostate cancer incidence and mortality rates. Eur Urol 77(1):38–52. https://doi.org/10.1016/j.eururo.2019.08.005
Teo MY, Rathkopf DE, Kantoff P (2019) Treatment of advanced prostate cancer. Annu Rev Med 70:479–499. https://doi.org/10.1146/annurev-med-051517-011947
Wei W, Zeng H, Zheng R, Zhang S, An L, Chen R et al (2020) Cancer registration in China and its role in cancer prevention and control. Lancet Oncol 21(7):e342–e349. https://doi.org/10.1016/s1470-2045(20)30073-5
Binder J, Kramer W (2001) Robotically-assisted laparoscopic radical prostatectomy. BJU Int 87(4):408–410. https://doi.org/10.1046/j.1464-410x.2001.00115.x
He S, Weng Y, Jiang Y (2022) Robot-assisted radical resection in prostate cancer comparative assessment with conventional laparoscopic prostatectomy: a retrospective comparative cohort study with single-center experience. Transl Androl Urol 11(12):1729–1734. https://doi.org/10.21037/tau-22-739
Zhu S, Ye H, Wu H, Ding G, Li G (2021) Ligating clip migration after robot-assisted laparoscopic radical prostatectomy: a single-center experience. Transl Cancer Res 10(7):3429–3435. https://doi.org/10.21037/tcr-21-7
Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A et al (2012) Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 62(3):405–417. https://doi.org/10.1016/j.eururo.2012.05.045
Moretti TBC, Magna LA, Reis LO (2022) Surgical results and complications for open, laparoscopic, and robot-assisted radical prostatectomy: a reverse systematic review. Eur Urol Open Sci 44:150–161. https://doi.org/10.1016/j.euros.2022.08.015
Gainsburg DM (2012) Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol 78(5):596–604
Templeton TW, Miller SA, Lee LK, Kheterpal S, Mathis MR, Goenaga-Diaz EJ et al (2021) Hypoxemia in young children undergoing one-lung ventilation: a retrospective cohort study. Anesthesiology 135(5):842–853. https://doi.org/10.1097/ALN.0000000000003971
Liu K, Scott JB, Jing G, Li J (2021) Management of postoperative hypoxemia. Respir Care 66(7):1136–1149. https://doi.org/10.4187/respcare.08929
Pan LL, Gao LL, Yang L, Pan CX, Yin YH, Zhu Y et al (2022) Effect of EIT-guided individualized PEEP setting on the incidence of hypoxemia in elderly patients undergoing robot-assisted radical prostatectomy. Zhonghua Yi Xue Za Zhi 102(47):3727–3733. https://doi.org/10.3760/cma.j.cn112137-20220415-00818
Smetana GW, Lawrence VA, Cornell JE (2006) American college of P. preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 144(8):581–95. https://doi.org/10.7326/0003-4819-144-8-200604180-00009
McKown AC, Casey JD, Russell DW, Joffe AM, Janz DR, Rice TW et al (2018) Risk factors for and prediction of hypoxemia during tracheal intubation of critically Ill adults. Ann Am Thorac Soc 15(11):1320–1327. https://doi.org/10.1513/AnnalsATS.201802-118OC
Baillard C, Boubaya M, Statescu E, Collet M, Solis A, Guezennec J et al (2019) Incidence and risk factors of hypoxaemia after preoxygenation at induction of anaesthesia. Br J Anaesth 122(3):388–394. https://doi.org/10.1016/j.bja.2018.11.022
Duan XZ, Zhang X, Tong DK, Ji F, Xu KH, He RZ (2020) Risk factors for and predictive nomogram of postoperative hypoxaemia in elderly patients with femoral neck fractures. J Int Med Res 48(10):300060520945132. https://doi.org/10.1177/0300060520945132
Zhu M, Wang J, Wang Q, Xie K, Wang M, Qian C et al (2019) The incidence and risk factors of low oxygenation after orthotropic liver transplantation. Ann Transplant 24:139–146. https://doi.org/10.12659/aot.913716
Luna IE, Kehlet H, Olsen RM, Wede HR, Hoevsgaard SJ, Aasvang EK (2020) Hypoxemia following hospital discharge after fast-track hip and knee arthroplasty—a prospective observational study subanalysis. Acta Anaesthesiol Scand 64(10):1405–1413. https://doi.org/10.1111/aas.13671
Rudasill SE, Dillon D, Karunungan K, Mardock AL, Hadaya J, Sanaiha Y et al (2021) The obesity paradox: underweight patients are at the greatest risk of mortality after cholecystectomy. Surgery 170(3):675–681. https://doi.org/10.1016/j.surg.2021.03.034
O’Byrne ML, Kim S, Hornik CP, Yerokun BA, Matsouaka RA, Jacobs JP et al (2017) Effect of obesity and underweight status on perioperative outcomes of congenital heart operations in children, adolescents, and young adults: an analysis of data from the society of thoracic surgeons database. Circulation 136(8):704–718. https://doi.org/10.1161/circulationaha.116.026778
Ranucci M, Ballotta A, La Rovere MT, Castelvecchio S, Surgical, (2014) Clinical outcome research G. postoperative hypoxia and length of intensive care unit stay after cardiac surgery: the underweight paradox? PloS one 9(4):e93992. https://doi.org/10.1371/journal.pone.0093992
Zatterale F, Longo M, Naderi J, Raciti GA, Desiderio A, Miele C et al (2019) Chronic adipose tissue inflammation linking obesity to insulin resistance and type 2 diabetes. Front Physiol 10:1607. https://doi.org/10.3389/fphys.2019.01607
Rosenberg AL, Watts C (2000) Patients readmitted to ICUs* : a systematic review of risk factors and outcomes. Chest 118(2):492–502. https://doi.org/10.1378/chest.118.2.492
Eikermann M, Santer P, Ramachandran SK, Pandit J (2019) Recent advances in understanding and managing postoperative respiratory problems. F1000 Res. https://doi.org/10.12688/f1000research.16687.1
Mohammed Iddrisu S, Considine J, Hutchinson A (2018) Frequency, nature and timing of clinical deterioration in the early postoperative period. J Clin Nurs 27(19–20):3544–3553. https://doi.org/10.1111/jocn.14611
Wortel CH, van Deventer SJ, Aarden LA, Lygidakis NJ, Büller HR, Hoek FJ et al (1993) Interleukin-6 mediates host defense responses induced by abdominal surgery. Surgery 114(3):564–570
Roberts J, Barnes W, Pennock M, Browne G (1988) Diagnostic accuracy of fever as a measure of postoperative pulmonary complications. Heart Lung 17(2):166–170
Engoren M (1995) Lack of association between atelectasis and fever. Chest 107(1):81–84. https://doi.org/10.1378/chest.107.1.81
Acknowledgements
We would like to express our sincere gratitude to Professor Chonghong Miao from Fudan University, for his invaluable guidance and expertise throughout the course of this research
Funding
The study was funded by Major Scientific Research Projects from Municipal Health Commission of Wuxi (Z202101 X.Z), Guiding Project from Science and Technology Bureau of Wuxi (NZ2021002 X.Z), National Natural Science Foundation of China(82271251 X.Z), Jiangsu Distinguished Medical Expert Project (X.Z) and Jiangsu Health Innovation Team Project (X.Z).
Author information
Authors and Affiliations
Contributions
QYZ: Study conception and design, acquisition of data, data analysis and interpretation, manuscript writing and critical revisions. LLZ, JSY and SML: Study conception and design, data analysis and interpretation, manuscript writing and critical revisions. XZ: supervision and critical revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval and consent to participate.
Ethical approval for this study was granted by the Clinical Research Ethics Committee of Wuxi People’s Hospital (Protocol Number: KY23038). The Clinical Research Ethics Committee of Wuxi People’s Hospital waived the need for informed consent.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Q., Zhu, L., Yuan, S. et al. Identifying risk factors for hypoxemia during emergence from anesthesia in patients undergoing robot-assisted laparoscopic radical prostatectomy. J Robotic Surg 18, 200 (2024). https://doi.org/10.1007/s11701-024-01964-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-024-01964-0