Abstract
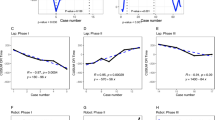
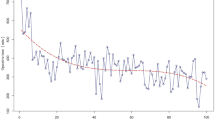
Although prior studies have discussed learning curves (LC) of robotic-assisted pancreaticoduodenectomy (RPD), a recognized definition is lacking. This study analyzed the clinical outcomes of 85 consecutive RPD cases performed by a single surgeon to evaluate the safety and learning curve of RPD using the da Vinci Xi robotic system. There were 51 male and 34 female patients, with a median age of 64 (20–87) years. The average preoperative body weight and BMI were 64.15 ± 11.43 kg and 23.36 ± 3.33 kg/m2, respectively. The clinical outcomes of each patient were analyzed using the textbook outcome(TO), and the learning curve of the RPD was evaluated by calculating the TO rate of patients using the cumulative sum analysis method (CUSUM).The operation time (OT) was 288.92 ± 44.41 min, and the postoperative hospital stay was 10 (1–134) days. In total, 23.52% (20/85), 5.88% (5/85), 2.35% (2/85), and 5.9% (5/85) experienced grade IIIa, IIIb, IV, and V complications. A total of 46 patients achieved TO outcomes (TO group), while 39 did not (non-TO group). The smoking rate in the TO group was lower (P < 0.05) and the albumin level was higher (P < 0.05) than that in the non-TO group. The TO rate became positive after the 56th case, all patients were divided into a learning improvement group (56 cases) and a proficient group (29 cases). The total bilirubin level in the learning improvement group was lower (P < 0.05) and the bleeding volume was higher (P < 0.05).RPD is safe and effective for carefully selected patients. The learning curve was completed after 56 patients.



Similar content being viewed by others
References
Whipple AO (1945) Pancreaticoduodenectomy for islet carcinoma : a five-year follow-up. Ann Surg 121(6):847–852. https://doi.org/10.1097/00000658-194506000-00008
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8(5):408–410. https://doi.org/10.1007/BF00642443
Asbun HJ, Stauffer JA (2012) Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 215(6):810–819. https://doi.org/10.1016/j.jamcollsurg.2012.08.006
Yin Z, Jian Z, Hou B, Jin H (2019) Surgical and oncological outcomes of laparoscopic versus open pancreaticoduodenectomy in patients with pancreatic duct adenocarcinoma. Pancreas 48(7):861–867. https://doi.org/10.1097/MPA.0000000000001363
Podda M, Gerardi C, Di Saverio S, Marino MV, Davies RJ, Pellino G et al (2020) Robotic-assisted versus open pancreaticoduodenectomy for patients with benign and malignant periampullary disease: a systematic review and meta-analysis of short-term outcomes. Surg Endosc 34(6):2390–2409. https://doi.org/10.1007/s00464-020-07460-4
Bao PQ, Mazirka PO, Watkins KT (2014) Retrospective comparison of robot-assisted minimally invasive versus open pancreaticoduodenectomy for periampullary neoplasms. J Gastrointest Surg 18(4):682–689. https://doi.org/10.1007/s11605-013-2410-3
Giulianotti PC, Mangano A, Bustos RE, Fernandes E, Masrur MA, Valle V et al (2020) Educational step-by-step surgical video about operative technique in robotic pancreaticoduodenectomy (RPD) at University of Illinois at Chicago (UIC): 17 steps standardized technique-Lessons learned since the first worldwide RPD performed in the year 2001. Surg Endosc 34(6):2758–2762. https://doi.org/10.1007/s00464-020-07383-0
Stafford AT, Walsh RM (2015) Robotic surgery of the pancreas: the current state of the art. J Surg Oncol 112(3):289–294. https://doi.org/10.1002/jso.23952
Memeo R, Sangiuolo F, de Blasi V, Tzedakis S, Mutter D, Marescaux J et al (2016) Robotic pancreaticoduodenectomy and distal pancreatectomy: Sstate of the art. J Visc Surg 153(5):353–359. https://doi.org/10.1016/j.jviscsurg.2016.04.001
Liu R, Wakabayashi G, Palanivelu C, Tsung A, Yang K, Goh BKP et al (2019) International consensus statement on robotic pancreatic surgery. Hepatobiliary Surg Nutr 8(4):345–360. https://doi.org/10.21037/hbsn.2019.07.08
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Görgec B, Benedetti Cacciaguerra A, Lanari J, Russolillo N, Cipriani F, Aghayan D et al (2021) Assessment of textbook outcome in laparoscopic and open liver surgery. JAMA Surg 156(8):e212064. https://doi.org/10.1001/jamasurg.2021.2064
Halpern SE, Moris D, Gloria JN, Shaw BI, Haney JC, Klapper JA et al (2023) Textbook outcome: definition and analysis of a novel quality measure in lung transplantation. Ann Surg 277(2):350–357. https://doi.org/10.1097/SLA.0000000000004916
Merath K, Chen Q, Bagante F, Beal E, Akgul O, Dillhoff M et al (2020) Textbook outcomes among medicare patients undergoing hepatopancreatic surgery. Ann Surg 271(6):1116–1123. https://doi.org/10.1097/SLA.0000000000003105
Ryoo DY, Eskander MF, Hamad A, Li Y, Cloyd J, Manilchuk A et al (2021) Mitigation of the robotic pancreaticoduodenectomy learning curve through comprehensive training. HPB (Oxford) 23(10):1550–1556. https://doi.org/10.1016/j.hpb.2021.03.010
Zureikat AH, Postlewait LM, Liu Y, Gillespie TW, Weber SM, Abbott DE et al (2016) A multi-institutional comparison of perioperative outcomes of robotic and open pancreaticoduodenectomy. Ann Surg 264(4):640–649. https://doi.org/10.1097/SLA.0000000000001869
Boone BA, Zenati M, Hogg ME, Steve J, Moser AJ, Bartlett DL et al (2015) Assessment of quality outcomes for robotic pancreaticoduodenectomy: identification of the learning curve. JAMA Surg 150(5):416–422. https://doi.org/10.1001/jamasurg.2015.17
Chen S, Chen J-Z, Zhan Q, Deng X-X, Shen B-Y, Peng C-H et al (2015) Robot-assisted laparoscopic versus open pancreaticoduodenectomy: a prospective, matched, mid-term follow-up study. Surg Endosc 29(12):3698–3711. https://doi.org/10.1007/s00464-015-4140-y
Rice MK, Hodges JC, Bellon J, Borrebach J, Al Abbas AI, Hamad A et al (2020) Association of mentorship and a formal robotic proficiency skills curriculum with subsequent generation’s learning curve and safety for robotic pancreaticoduodenectomy. JAMA Surg 155(7):607–615. https://doi.org/10.1001/jamasurg.2020.1040
Morelli L, Furbetta N, Palmeri M, Guadagni S, Di Franco G, Gianardi D et al (2023) Initial 50 consecutive full-robotic pancreatoduodenectomies without conversion by a single surgeon: a learning curve analysis from a tertiary referral high-volume center. Surg Endosc 37(5):3531–3539. https://doi.org/10.1007/s00464-022-09784-9
Shi Y, Wang W, Qiu W, Zhao S, Wang J, Weng Y et al (2021) Learning curve from 450 cases of robot-assisted pancreaticoduocectomy in a high-volume pancreatic center: optimization of operative procedure and a retrospective study. Ann Surg 274(6):e1277–e1283. https://doi.org/10.1097/SLA.0000000000003664
Stiles ZE, Dickson PV, Deneve JL, Glazer ES, Dong L, Wan JY et al (2018) The impact of unplanned conversion to an open procedure during minimally invasive pancreatectomy. J Surg Res 227:168–177. https://doi.org/10.1016/j.jss.2018.02.028
van Berge Henegouwen MI, Allema JH, van Gulik TM, Verbeek PC, Obertop H, Gouma DJ (1995) Delayed massive haemorrhage after pancreatic and biliary surgery. Br J Surg 82(11):1527–1531. https://doi.org/10.1002/bjs.1800821124
Trede M, Schwall G (1988) The complications of pancreatectomy. Ann Surg 207(1):39–47. https://doi.org/10.1097/00000658-198801000-00009
Bassi C, Falconi M, Salvia R, Mascetta G, Molinari E, Pederzoli P (2001) Management of complications after pancreaticoduodenectomy in a high volume centre: results on 150 consecutive patients. Dig Surg 18(6):453–457. https://doi.org/10.1159/000050193
Büchler MW, Wagner M, Schmied BM, Uhl W, Friess H, Z’Graggen K (2003) Changes in morbidity after pancreatic resection: toward the end of completion pancreatectomy. Arch Surg 138(12):1310–1314. https://doi.org/10.1001/archsurg.138.12.1310
Coe TM, Fong ZV, Wilson SE, Talamini MA, Lillemoe KD, Chang DC (2015) Outcomes improvement is not continuous along the learning curve for pancreaticoduodenectomy at the hospital level. J Gastrointest Surg 19(12):2132–2137. https://doi.org/10.1007/s11605-015-2967-0
Kawka M, Gall TMH, Hand F, Nazarian S, Cunningham D, Nicol D et al (2023) The influence of procedural volume on short-term outcomes for robotic pancreatoduodenectomy-a cohort study and a learning curve analysis. Surg Endosc 37(6):4719–4727. https://doi.org/10.1007/s00464-023-09941-8
Zhang T, Zhao Z-M, Gao Y-X, Lau WY, Liu R (2019) The learning curve for a surgeon in robot-assisted laparoscopic pancreaticoduodenectomy: a retrospective study in a high-volume pancreatic center. Surg Endosc 33(9):2927–2933. https://doi.org/10.1007/s00464-018-6595-0
Beane JD, Zenati M, Hamad A, Hogg ME, Zeh HJ, Zureikat AH (2019) Robotic pancreatoduodenectomy with vascular resection: outcomes and learning curve. Surgery 166(1):8–14. https://doi.org/10.1016/j.surg.2019.01.037
Napoli N, Kauffmann EF, Palmeri M, Miccoli M, Costa F, Vistoli F et al (2016) The learning curve in robotic pancreaticoduodenectomy. Dig Surg 33(4):299–307. https://doi.org/10.1159/000445015
Wei Z-G, Liang C-J, Du Y, Zhang Y-P, Liu Y (2022) Learning curve for a surgeon in robotic pancreaticoduodenectomy through a “G”-shaped approach: a cumulative sum analysis. World J Clin Cases 10(14):4357–4367. https://doi.org/10.12998/wjcc.v10.i14.4357
Shi Y, Jin J, Qiu W, Weng Y, Wang J, Zhao S et al (2020) Short-term outcomes after robot-assisted vs open pancreaticoduodenectomy after the learning curve. JAMA Surg 155(5):389–394. https://doi.org/10.1001/jamasurg.2020.0021
Park SE, Choi HJ, You YK, Hong TH (2021) Effectiveness and stability of robot-assisted anastomosis in minimally invasive pancreaticoduodenectomy. Ann Surg Treat Res 100(6):329–337. https://doi.org/10.4174/astr.2021.100.6.329
Chalikonda S, Aguilar-Saavedra JR, Walsh RM (2012) Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection. Surg Endosc 26(9):2397–2402. https://doi.org/10.1007/s00464-012-2207-6
Zeh HJ, Zureikat AH, Secrest A, Dauoudi M, Bartlett D, Moser AJ (2012) Outcomes after robot-assisted pancreaticoduodenectomy for periampullary lesions. Ann Surg Oncol 19(3):864–870. https://doi.org/10.1245/s10434-011-2045-0
Kim HS, Han Y, Kang JS, Kim H, Kim JR, Kwon W et al (2018) Comparison of surgical outcomes between open and robot-assisted minimally invasive pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci 25(2):142–149. https://doi.org/10.1002/jhbp.522
Joseph S, Vyas D (2015) Jury is out: robotic or laparoscopic or open surgery. Am J Robot Surg 2(1):59. https://doi.org/10.1166/ajrs.2015.1012
Buchs NC, Addeo P, Bianco FM, Ayloo S, Benedetti E, Giulianotti PC (2011) Robotic versus open pancreaticoduodenectomy: a comparative study at a single institution. World J Surg 35(12):2739–2746. https://doi.org/10.1007/s00268-011-1276-3
Howard TJ, Krug JE, Yu J, Zyromski NJ, Schmidt CM, Jacobson LE et al (2006) A margin-negative R0 resection accomplished with minimal postoperative complications is the surgeon’s contribution to long-term survival in pancreatic cancer. J Gastrointest Surg 10(10):1338–1345. https://doi.org/10.1016/j.gassur.2006.09.008
Pawlik TM, Gleisner AL, Cameron JL, Winter JM, Assumpcao L, Lillemoe KD et al (2007) Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 141(5):610–618. https://doi.org/10.1016/j.surg.2006.12.013
Corsini MM, Miller RC, Haddock MG, Donohue JH, Farnell MB, Nagorney DM et al (2008) Adjuvant radiotherapy and chemotherapy for pancreatic carcinoma: the Mayo Clinic experience (1975–2005). J Clin Oncol 26(21):3511–3516. https://doi.org/10.1200/JCO.2007.15.8782
Al Faraï A, Garnier J, Ewald J, Marchese U, Gilabert M, Moureau-Zabotto L et al (2019) International Study Group of Pancreatic Surgery type 3 and 4 venous resections in patients with pancreatic adenocarcinoma:the Paoli-Calmettes Institute experience. Eur J Surg Oncol 45(10):1912–1918. https://doi.org/10.1016/j.ejso.2019.06.003
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ et al (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25. https://doi.org/10.1016/j.surg.2007.02.001
Zhou J, Xiong L, Miao X, Liu J, Zou H, Wen Y (2020) Outcome of robot-assisted pancreaticoduodenectomy during initial learning curve versus laparotomy. Sci Rep 10(1):9621. https://doi.org/10.1038/s41598-020-66722-2
Acknowledgements
The authors would like to thank all the reviewers who participated in the review. We would like to thank Editage (www.editage.cn) for English language editing.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
YY made substantial contributions to the conception and design of the study. CE and CL contributed to the acquisition of the data. LW analyzed and interpreted the data. TJ critically revised it for important intellectual content. All authors reviewed the results and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was granted by the ethics committee of The China–Japan Union Hospital of Jilin University and performed in line with the principles of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Data availability
All data are available from the corresponding author on reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, Y., Changyong, E., Lin, C. et al. Safety and learning curve analysis of robotic-assisted pancreaticoduodenectomy: experience of a single surgeon. J Robotic Surg 18, 92 (2024). https://doi.org/10.1007/s11701-024-01844-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-024-01844-7