Abstract
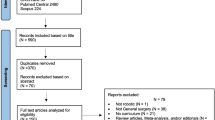
The use of robotic surgery has increased exponentially in the United States. Despite this uptick in popularity, no standardized training pathway exists for surgical residents or practicing surgeons trying to cross-train onto the platform. We set out to perform a systematic review of existing literature to better describe and analyze existing robotic surgical training curricula amongst academic surgery programs. A systematic electronic search of the PubMed, Cochrane, and EBSCO databases was performed for articles describing simulation in robotic surgery from January 2010 to May 2022. Medical Subject Heading (MeSH) terms and keywords used to conduct this search were “Robotic,” “Surgery,” “Robotic Surgery,” “Training,” “Curriculum,” “Education,” and “Residency Program.” A total of 110 articles were identified for the systematic review. After screening the titles and abstracts, a total of 36 full-text original articles were included in this systematic review. Of these, 24 involved robotic surgery curricula designed to teach general robotic skills, whereas the remaining 12 were for teaching procedure specific skills. Of the 24 studies involving general robotic skills, 13 included didactics as a part of the curriculum, 23 utilized virtual reality trainers, 3 used inanimate tissue, and 1 used live animal models. Of the 12 papers reviewed regarding procedure specific curricula, seven involved urologic procedures (radical prostatectomy and nephrectomy), two involved general surgical procedures (colectomy and Roux-en-Y gastric bypass surgery), two involved obstetrics and gynecology procedures (hysterectomy with myomectomy and sacrocolpopexy, hysterectomy with pelvic lymphadenectomy) and one involved a cardiothoracic surgery procedure (robotic internal thoracic artery harvest). With the rapid implementation of robotic surgery, training programs have been tasked with the responsibility of ensuring their trainees are adequately proficient in the platform prior to graduation. However, due to the lack of uniformity between surgical training programs, when it comes to robotic surgical experience, a strong need persists for a standardized national robotics training curriculum.

Similar content being viewed by others
Data availability
The authors confirms that the data supporting the findings of this paper is publically available.
References
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911–e1918911. https://doi.org/10.1001/jamanetworkopen.2019.18911
Childers CP, Maggard-Gibbons M (2018) Estimation of the acquisition and operating costs for robotic surgery. JAMA 320(8):835–836. https://doi.org/10.1001/jama.2018.9219
Ericsson KA (2004) Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med 79(10 Suppl):S70-81. https://doi.org/10.1097/00001888-200410001-00022
Cannon-Bowers JA, Bowers C, Procci K (2010) Optimizing learning in surgical simulations: guidelines from the science of learning and human performance. Surg Clin North Am 90(3):583–603. https://doi.org/10.1016/j.suc.2010.02.006
Moulton CA et al (2006) Teaching surgical skills: what kind of practice makes perfect?: a randomized, controlled trial. Ann Surg 244(3):400–409. https://doi.org/10.1097/01.sla.0000234808.85789.6a
Sachdeva AK (2005) Acquiring skills in new procedures and technology: the challenge and the opportunity. Arch Surg 140(4):387–389. https://doi.org/10.1001/archsurg.140.4.387
Ericsson KA (2008) Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med 15(11):988–994. https://doi.org/10.1111/j.1553-2712.2008.00227.x
Foell K et al (2013) Robotic surgery basic skills training: evaluation of a pilot multidisciplinary simulation-based curriculum. Can Urol Assoc J 7(11–12):430–434. https://doi.org/10.5489/cuaj.222
Connolly M et al (2014) Validation of a virtual reality-based robotic surgical skills curriculum. Surg Endosc 28(5):1691–1694. https://doi.org/10.1007/s00464-013-3373-x
Green CA, Chern H, O’Sullivan PS (2018) Current robotic curricula for surgery residents: a need for additional cognitive and psychomotor focus. Am J Surg 215(2):277–281. https://doi.org/10.1016/j.amjsurg.2017.09.040
Dulan G et al (2012) Developing a comprehensive, proficiency-based training program for robotic surgery. Surgery 152(3):477–488. https://doi.org/10.1016/j.surg.2012.07.028
Winder JS et al (2016) Implementing a robotics curriculum at an academic general surgery training program: our initial experience. J Robot Surg 10(3):209–213. https://doi.org/10.1007/s11701-016-0569-9
Moit H et al (2019) A standardized robotic training curriculum in a general surgery program. JSLS. https://doi.org/10.4293/JSLS.2019.00045
Chen R et al (2020) A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc 34(1):361–367. https://doi.org/10.1007/s00464-019-06775-1
Satava RM et al (2020) Proving the effectiveness of the fundamentals of robotic surgery (FRS) skills curriculum: a single-blinded, multispecialty, multi-institutional randomized control trial. Ann Surg 272(2):384–392. https://doi.org/10.1097/SLA.0000000000003220
Stegemann AP et al (2013) Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology 81(4):767–774. https://doi.org/10.1016/j.urology.2012.12.033
Herron D, Marohn M (2008) A consensus document on robotic surgery. Surg Endosc 22(2):313–325. https://doi.org/10.1007/s00464-007-9727-5
Ahmed K et al (2015) Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int 116(1):93–101. https://doi.org/10.1111/bju.12974
Brunckhorst O et al (2016) Training, simulation, the learning curve, and how to reduce complications in urology. Eur Urol Focus 2(1):10–18. https://doi.org/10.1016/j.euf.2016.02.004
Bahler CD, Sundaram CP (2014) Training in robotic surgery: simulators, surgery, and credentialing. Urol Clin 41(4):581–589. https://doi.org/10.1016/j.ucl.2014.07.012
Farivar BS, Flannagan M, Leitman IM (2015) General surgery residents’ perception of robot-assisted procedures during surgical training. J Surg Educ 72(2):235–242. https://doi.org/10.1016/j.jsurg.2014.09.008
Moher D et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Aradaib M et al (2019) Safe adoption of robotic colorectal surgery using structured training: early Irish experience. J Robot Surg 13(5):657–662. https://doi.org/10.1007/s11701-018-00911-0
Bertolo R et al (2018) Single session of robotic human cadaver training: the immediate impact on urology residents in a teaching hospital. J Laparoendosc Adv Surg Tech A 28(10):1157–1162. https://doi.org/10.1089/lap.2018.0109
Dioun SM et al (2017) Setting benchmarks for the new user: training on the robotic simulator. JSLS. https://doi.org/10.4293/JSLS.2017.00059
Fantola G et al (2014) Robotic Roux-en-Y gastric bypass surgical simulation curriculum. Obes Surg 24(10):1833–1834. https://doi.org/10.1007/s11695-014-1370-3
Fastenberg JH, Gibber MJ, Smith RV (2018) Introductory TORS training in an otolaryngology residency program. J Robot Surg 12(4):617–623. https://doi.org/10.1007/s11701-018-0784-7
Gerull W, Zihni A, Awad M (2020) Operative performance outcomes of a simulator-based robotic surgical skills curriculum. Surg Endosc 34(10):4543–4548. https://doi.org/10.1007/s00464-019-07243-6
Gomez PP, Willis RE, Van Sickle KR (2015) Development of a virtual reality robotic surgical curriculum using the da Vinci Si surgical system. Surg Endosc 29(8):2171–2179. https://doi.org/10.1007/s00464-014-3914-y
Grannan HR et al (2021) Robotic general surgery resident training curriculum: a pilot experience. Surg Laparosc Endosc Percutaneous Tech 31(5):588–593. https://doi.org/10.1097/SLE.0000000000000942
Harrison P et al (2018) The validation of a novel robot-assisted radical prostatectomy virtual reality module. J Surg Educ 75(3):758–766. https://doi.org/10.1016/j.jsurg.2017.09.005
Hogg ME et al (2017) Training in minimally invasive pancreatic resections: a paradigm shift away from “See one, do one, teach one.” HPB (Oxford) 19(3):234–245. https://doi.org/10.1016/j.hpb.2017.01.016
Ko YH, Choi JY, Song PH (2018) Concurrent validation of a robotic simulator curriculum focused on “core” exercises: does it help overcome baseline skill levels? Int J Urol 25(8):760–761. https://doi.org/10.1111/iju.13704
Krause W, Bird J (2019) Training robotic community surgeons: our experience implementing a robotics curriculum at a rural community general surgery training program. J Robot Surg 13(3):385–389. https://doi.org/10.1007/s11701-018-0860-z
Larcher A et al (2019) The ERUS curriculum for robot-assisted partial nephrectomy: structure definition and pilot clinical validation. Eur Urol 75(6):1023–1031. https://doi.org/10.1016/j.eururo.2019.02.031
Larcher A et al (2019) Virtual reality validation of the ERUS simulation-based training programmes: results from a high-volume training centre for robot-assisted surgery. Eur Urol 75(5):885–887. https://doi.org/10.1016/j.eururo.2019.02.008
Margueritte F et al (2020) Description of an initiation program to robotic in vivo gynecological surgery for junior surgeons. J Gynecol Obstet Hum Reprod 49(3):101627. https://doi.org/10.1016/j.jogoh.2019.101627
Mariani A, Pellegrini E, De Momi E (2021) Skill-oriented and performance-driven adaptive curricula for training in robot-assisted surgery using simulators: a feasibility study. IEEE Trans Biomed Eng 68(2):685–694. https://doi.org/10.1109/TBME.2020.3011867
Mariani A, et al (2018) Design and evaluation of a performance-based adaptive curriculum for robotic surgical training: a pilot study. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual International Conference. 2018:2162–2165. https://doi.org/10.1109/EMBC.2018.8512728
Mustafa S et al (2019) Robotic curriculum enhances minimally invasive general surgery residents’ education. J Surg Educ 76(2):548–553. https://doi.org/10.1016/j.jsurg.2018.08.020
Raison N et al (2017) Competency based training in robotic surgery: benchmark scores for virtual reality robotic simulation. BJU Int 119(5):804–811. https://doi.org/10.1111/bju.13710
Raza SJ et al (2014) Construct validation of the key components of fundamental skills of robotic surgery (FSRS) curriculum—a multi-institution prospective study. J Surg Educ 71(3):316–324. https://doi.org/10.1016/j.jsurg.2013.10.006
Rusch P, Verheijen RHM (2018) The Society of European Robotic Gynaecological Surgery (SERGS) pilot curriculum for robot-assisted gynaecological surgery: authors’ reply to a letter to the editor. Arch Gynecol Obstet 297(6):1597. https://doi.org/10.1007/s00404-017-4612-5
Shay SG et al (2019) Initial and long-term retention of robotic technical skills in an otolaryngology residency program. Laryngoscope 129(6):1380–1385. https://doi.org/10.1002/lary.27425
Shim JS et al (2018) Comparison of effective teaching methods to achieve skill acquisition using a robotic virtual reality simulator: expert proctoring versus an educational video versus independent training. Medicine (Baltimore) 97(51):e13569. https://doi.org/10.1097/MD.0000000000013569
Shim JS et al (2018) Predictive validation of a robotic virtual reality simulator: the tube 3 module for practicing vesicourethral anastomosis in robot-assisted radical prostatectomy. Urology 122:32–36. https://doi.org/10.1016/j.urology.2018.08.013
Suh I et al (2011) Training program for fundamental surgical skill in robotic laparoscopic surgery. Int J Med Robot 7(3):327–333. https://doi.org/10.1002/rcs.402
Tillou X et al (2016) Robotic surgery simulator: elements to build a training program. J Surg Educ 73(5):870–878. https://doi.org/10.1016/j.jsurg.2016.04.008
Valdis M et al (2015) Validation of a novel virtual reality training curriculum for robotic cardiac surgery: a randomized trial. Innovations (Phila) 10(6):383–388. https://doi.org/10.1097/IMI.0000000000000222
Vargas MV et al (2017) Transferability of virtual reality, simulation-based, robotic suturing skills to a live porcine model in novice surgeons: a single-blind randomized controlled trial. J Minim Invasive Gynecol 24(3):420–425. https://doi.org/10.1016/j.jmig.2016.12.016
Volpe A et al (2015) Pilot validation study of the European association of urology robotic training curriculum. Eur Urol 68(2):292–299. https://doi.org/10.1016/j.eururo.2014.10.025
Walliczek U et al (2016) Effect of training frequency on the learning curve on the da Vinci Skills Simulator. Head Neck 38(Suppl 1):E1762–E1769. https://doi.org/10.1002/hed.24312
Walliczek-Dworschak U et al (2017) The effect of different training exercises on the performance outcome on the da Vinci Skills Simulator. Surg Endosc 31(6):2397–2405. https://doi.org/10.1007/s00464-016-5240-z
White J, Sharma A (2018) Development and assessment of a transoral robotic surgery curriculum to train otolaryngology residents. ORL 80(2):69–76. https://doi.org/10.1159/000479744
Wiener S et al (2015) Construction of a urologic robotic surgery training curriculum: how many simulator sessions are required for residents to achieve proficiency? J Endourol 29(11):1289–1293. https://doi.org/10.1089/end.2015.0392
Perrenot C et al (2012) The virtual reality simulator dV-Trainer® is a valid assessment tool for robotic surgical skills. Surg Endosc 26(9):2587–2593. https://doi.org/10.1007/s00464-012-2237-0
Lee CS et al (2022) Model development of a novel robotic surgery training exercise with electrocautery. Cureus. https://doi.org/10.7759/cureus.24531
Patnaik R et al (2022) Building a low-cost and low-fidelity kidney transplant model: a technical report on the san antonio kidney transplant model. Cureus. https://doi.org/10.7759/cureus.23883
Hogg ME et al (2017) Mastery-based virtual reality robotic simulation curriculum: the first step toward operative robotic proficiency. J Surg Educ 74(3):477–485. https://doi.org/10.1016/j.jsurg.2016.10.015
Aghazadeh MA et al (2015) External validation of global evaluative assessment of robotic skills (GEARS). Surg Endosc 29(11):3261–3266. https://doi.org/10.1007/s00464-015-4070-8
Messick S (1998) Test validity: a matter of consequence. Soc Indic Res 45(1):35–44. https://doi.org/10.1023/A:1006964925094
Kotsis SV, Chung KC (2013) Application of see one, do one, teach one concept in surgical training. Plast Reconstr Surg 131(5):1194. https://doi.org/10.1097/PRS.0b013e318287a0b3
Cameron JL (1997) William Stewart Halsted. Our surgical heritage. Annals Surg 225(5):445. https://doi.org/10.1097/00000658-199705000-00002
Bandura A (2009) Social cognitive theory of mass communication. Routledge, Media Effects, pp 110–140. https://doi.org/10.1207/S1532785XMEP0303_03
Issenberg SB, McGaghie WC (2013) Looking to the future. International best practices for evaluation in the health professions. Radcliffe Publishing Ltd, London, p 344
Gallagher AG et al (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241(2):364. https://doi.org/10.1097/01.sla.0000151982.85062.80
Scott DJ, Dunnington GL (2008) The new ACS/APDS skills curriculum: moving the learning curve out of the operating room. J Gastrointest Surg 12(2):213–221. https://doi.org/10.1007/s11605-007-0357-y
Barsuk JH et al (2017) Residents’ procedural experience does not ensure competence: a research synthesis. J Grad Med Educ 9(2):201–208. https://doi.org/10.4300/JGME-D-16-00426.1
Brunner WC et al (2004) Laparoscopic virtual reality training: are 30 repetitions enough? J Surg Res 122(2):150–156
Rashid P (2017) Surgical education and adult learning: integrating theory into practice. F1000Research. https://doi.org/10.12688/f1000research.10870.1
Patnaik R, Stefanidis D (2019) Outcome-based training and the role of simulation. In: Comprehensive healthcare simulation: surgery and surgical subspecialties. Springer, p. 69–78. https://doi.org/10.1007/978-3-319-98276-2_7
Holst D et al (2015) Crowd-sourced assessment of technical skills: an adjunct to urology resident surgical simulation training. J Endourol 29(5):604–609. https://doi.org/10.1089/end.2014.0616
Lendvay TS, White L, Kowalewski T (2015) Crowdsourcing to assess surgical skill. JAMA Surg 150(11):1086–1087. https://doi.org/10.1001/jamasurg.2015.2405
Chen C et al (2014) Crowd-sourced assessment of technical skills: a novel method to evaluate surgical performance. J Surg Res 187(1):65–71. https://doi.org/10.1016/j.jss.2013.09.024
Vassiliou MC et al (2010) FLS and FES: comprehensive models of training and assessment. Surg Clin 90(3):535–558. https://doi.org/10.1016/j.suc.2010.02.012
Vassiliou MC et al (2014) Fundamentals of endoscopic surgery: creation and validation of the hands-on test. Surg Endosc 28(3):704–711. https://doi.org/10.1007/s00464-013-3298-4
Goova MT et al (2008) Implementation, construct validity, and benefit of a proficiency-based knot-tying and suturing curriculum. J Surg Educ 65(4):309–315. https://doi.org/10.1016/j.jsurg.2008.04.004
Green CA et al (2020) The current state of surgeon credentialing in the robotic era. Annals Laparosc Endosc Surg. https://doi.org/10.2103/ales.2019.11.06
Torrent-Sellens J, Jiménez-Zarco AI, Saigí-Rubió F (2021) Do people trust in robot-assisted surgery? Evidence from Europe. Int J Environ Res Public Health 18(23):12519. https://doi.org/10.3390/ijerph182312519
Acknowledgements
We would like to thank the Defense Health Agency Restoral Grant along with Ruth L Kirschstein NRSA Institutional Research Training Grant (T32CA148724 awarded to Dr. Mustafa T.A. Khan) for their support of this work along with the Brooke Army Medical Center librarian for performing some of the literature searches.
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
MK, RP, CL, CW, VD, RK, RL performed literature search, reviewed abstracts, reviewed full papers, wrote main manuscript text. RP prepared Fig. 1. All authors reviewed manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We do not have any relevant financial disclosures or conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khan, M.T.A., Patnaik, R., Lee, C.S. et al. Systematic review of academic robotic surgery curricula. J Robotic Surg 17, 719–743 (2023). https://doi.org/10.1007/s11701-022-01500-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01500-y