Abstract
The adoption of minimally invasive laparoscopic techniques has revolutionised urological practice. This necessitates a pneumoperitoneum (PNP) and the impact the PNP pressure has on post-operative outcomes is uncertain. During the current COVID-19 era guidance has suggested the utilisation of lower PNP pressures to mitigate the risk of intra-operative viral transmission. Review the current literature regarding the impact of pneumoperitoneum pressure, within the field of urology, on post-operative outcomes. A search of the PubMed, Medline and EMBASE databases was undertaken to identify studies that met the inclusion criteria. The Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines were adhered to. Ten studies, that included both randomised controlled trials and retrospective case series reviews, were identified that met the inclusion criteria. The effect of PNP pressure on outcomes following prostatectomy, live donor nephrectomy, partial nephrectomy and a variety of benign upper tract procedures were discussed. Low pressure PNP appears safe when compared to high pressure PNP, potentially reducing post-operative pain and rates of ileus. When compared to general surgery, there is a lack of quality evidence investigating the impact of PNP pressures on outcomes within urology. Low pressure PNP appears non-inferior to high pressure PNP. More research is required to validate this finding, particularly post-cystectomy and nephrectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pneumoperitoneum (PNP), the act of introducing gas into the peritoneum, is a requisite in laparoscopic surgery as it creates a space and a visual field. The pressure at which gas is insufflated into the abdominal cavity to create the pneumoperitoneum may influence both peri-operative variables and post-operative recovery [1]. When compared to other surgical specialities there is a paucity of research on PNP pressures within urology.
Since the laparoscopic approach to surgery was adopted by surgeons from various specialities, there has been ongoing interest regarding the pressures required to create the artificial PNP. During the current COVID-19 pandemic, controversy has existed regarding the aerosol-generation necessitated to create the PNP, and the effect this may have on viral transmission. There is, however, limited evidence to suggest that significant transmission occurs. Recommendations, to mitigate any potential exposure to aerosolised particles, have included the lowering of pneumoperitoneum pressures (to 12 mmHg) [2].
Intraoperatively, the use of a higher pressure offers advantages such as improved visibility and larger space within which to operate in [3]. The associated pressure applied to tissues, compressing them, is assumed to reduce peri-operative venous ooze. High pressures conversely have been suggested to potentially cause tissue ischaemia due to compression and diaphragmatic splinting [4].
Postoperatively, laparoscopic surgery is associated with a specific discomfort or pain secondary to the pneumoperitoneum created. This classically presents as abdominal discomfort and referred shoulder tip pain. A lower pressure pneumoperitoneum has been demonstrated in a variety of general surgical operations to reduce this postoperative pain, accelerating recovery times, analgesic use and hospital stay [5].
The Cochrane Meta-Analysis reviewing low pressure laparoscopic cholecystectomy did not demonstrate higher incidence of post-operative complications [5]. The aim of this review is to assess the literature to date investigating pneumoperitoneum pressures within the field of urology.
Method
The primary outcome assessed in this paper was the effect on postoperative clinical outcomes of changing pneumoperitoneum pressures. This included intraoperative blood loss, length of operation, postoperative pain, length of hospital stay, readmission within 30 days, day 1 postoperative haemoglobin and eGFR and complication rates (including ileus, fistula formation, urinary retention and haematoma). A secondary outcome was the safety and viability of the operation. Some studies allocated subjective scores to ‘difficulty’ and ‘progression’ of the operations.
A search of PubMed, Medline and EMBASE databases was performed by two independent authors using the following search terms.
((Pneumoperitoneum[Title]) OR (Insufflation[Title]) OR ("Intra-abdominal pressure"[Title])) AND ((Nephrectomy[Title]) OR (Prostatectomy[Title]) OR (Cystectomy[Title]) OR ("Partial nephrectomy"[Title]) OR (Urol*[Title]) OR (Robot*[Title])).
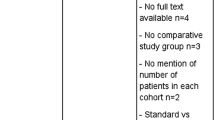
The titles and abstracts of the papers were screened to ensure they met the inclusion criteria and to ascertain their relevance. The inclusion and exclusion criteria were as described below.
Papers that did not report on clinical parameters as their primary or secondary outcomes were excluded. Multiple papers reported on outcomes from an anaesthesiologist’s perspective and evaluated parameters such as mean arterial pressure or intraoperative lactate. They also included papers discussing the effect on renal, respiratory and cardiac function intraoperatively. These papers did not meet our inclusion criteria and this data was not reported on.
The subsequent studies that met the inclusion criteria were screened by the two initial authors in full. Having been identified for the review they were classified by type of operation.
Assessment of bias
The Risk of Bias in Non-randomised Studies—of interventions (ROBINS-I) tool was used to assess for bias within the non-randomised papers [6]. For the randomised studies, bias was assessed using the ‘Revised Cochrane risk-of-bias tool for randomised trials (RoB 2).
As per the Table 1, the 5 Randomised Control Trials (RCTs) included contained a significant amount of bias. There are 4 that have concerning levels of bias and 1 with a high risk of bias. Again, 3 of the non-randomised trials have a moderate risk of bias and 1 has a high risk of bias. The results should be interpreted with this in mind.
Results
Prostatectomy
Christensen and colleagues compared a pressure of 12 mmHg versus 15 mmHg, following a retrospective review of their single surgeon prostatectomy database from 2012 to 2015 [7]. 100 patients who had prostatectomy at 15 mmHg and then 100 who had prostatectomy at 12 mmHg. No randomisation was used as this was a retrospective study. A similar approach to a Montsouris approach was described but no mention of Trendelenburg position was made. ASA grades were not compared between the cohorts. Primary outcomes assessed included operative time, blood loss, length of stay, post-operative ileus rates, fistula formation, urinary retention and haematoma formation.
A lower rate of postoperative ileus in the low-pressure group was demonstrated, however, this was not deemed statistically different (4% versus 8% p = 0.23). Again, no statistically significant difference was found in any of the outcomes between the groups. From their study, they concluded that the lower pressure PNP was non-inferior.
Rohloff and colleagues performed a retrospective review of 400 patients undergoing prostatectomy over a 5-year period. A single surgeon (the same as in the Christensen et al. paper [7]) performed 209 successful prostatectomies at 15 mmHg of which, 202 were included in the study [8]. The same surgeon then changed practice and performed the remaining 198 prostatectomies at 12 mmHg which were included as the second arm of the study. Over a 5-year period, a considerable learning curve is likely to be present and should be accounted for. Once again, surgical approach was not described in detail and nor were ASA grades of the patients. Perioperative, intraoperative and postoperative parameters were standardised across the operations including the reporting of post-operative ileus for which they employed a strict criterion based on symptoms.
Primary outcomes were the rate of postoperative ileus, complications and length of stay. Secondary outcomes included blood loss intraoperatively and length of operation. Length of stay in days was statistically significantly reduced in the low-pressure group (1.49 versus 1.76 p = 0.022) although this may not translate significantly to clinical practice. Postoperative ileus rates were also significantly reduced at 12 mmHg vs 15 mmHg (10 patients versus 25 patients p = 0.014). No other parameters were significantly different between the groups. Accounting for the learning curve and retrospective nature of the study, the team concluded that, patient benefits could be derived, by performing their prostatectomies at lower pressures.
Rohloff and colleagues subsequently performed a prospective, randomised double blind trial comparing 105 patients undergoing prostatectomy at 12 mmHg with 96 patients at 8 mmHg [9]. They used a computer-generated code to randomise allocation of the patients to a study arm. A nurse programmed the pressure into the insufflation device after the DaVinci robot was docked and then the nurse covered the monitor. A single, experienced surgeon (again the same as the previous two papers) performed all the operations. Pressure was not increased during dissection of the dorsal venous complex and a standardised approach was used. All cases were performed in the steep Trendelenburg position. ASA grades were analysed and were similar between the cohorts. At the end of the case, the surgeon was asked to guess the pressure. This was not revealed to them until 30 days after discharge. The surgeon correctly guessed 61% of the time; at 8 mmHg 45% of the time and at 12 mmHg they guessed correctly 76% of the time.
The primary outcome was postoperative ileus rates and secondary outcomes included length of operation, estimated blood loss, and positive surgical margin status. A reduction in postoperative ileus rates with lower pneumoperitoneum pressures was observed; 2% at 8 mmHg and 4.8% at 12 mmHg, this, however, was not statistically significant (2 versus 5 p = 0.45). More overall complications were noted in the 12 mmHg group versus the 8 mmHg group (10 versus 8). In the 8 mmHg group, there were 3 Clavien–Dindo 3b complications, including 1 delayed rectal injury requiring diversion, 1 general surgery consult for extensive adhesiolysis resulting in enterotomy and 1 small bowel injury requiring resection and anastomosis. The team analysed the video footage of the operation postoperatively and ‘strongly felt that these injuries were due to anatomic aberrations and were inevitable regardless of PNP pressure’. There were no significant differences in estimated blood loss, total length of operative time and positive margin status.
No operation required the surgeon to increase PNP pressure intraoperatively due to poor views or difficult progression. Furthermore, there were two independent variables, smoking and the administration of intra-operative intravenous fluids, were that found to be associated with postoperative ileus rate. The team concluded that robotic assisted Prostatectomy at low pressures is non-inferior to standard pressures.
Ferroni M and colleagues analysed their prospectively collected single surgeon database comparing 300 patients operated at 6 mmHg with their prior 300 patients operated on at 15 mmHg [10]. Outcomes assessed included pain scores, length of hospital stay, readmission rates and complications. They used a low lithotomy and steep Trendelenburg position in all cases. The pressure in the 6 mmHg group did not have to be increased intraoperatively in any cases due to poor visibility or lack of progression. They noted that the mean length of operation did not vary significantly between the first 100, second 100 and third 100 cases done at 6 mmHg.
Mean operative time was significantly longer in the 6 mmHg group (145.7 min versus 155.2 min p < 0.001). Mean estimated blood loss was higher at 6 mmHg, however, no blood transfusions were given to either group. Conversely, the mean length of stay was shorter in the 6-mmHg group at 0.57 versus 1.00 days with 43.3% of patients in the 6-mmHg group discharged home the day of surgery. There were no differences in morphine equivalents or maximum pain scores in the first 4 h after surgery, but there was a small improvement (18%) in pain scores at 5–12 h postoperatively in the low-pressure group. The 30-day complication rate was 8.7% in the 15 mmHg group versus 4.0% in the lower pressure group (p = 0.02), with 30-day hospital readmissions of 5.7% for the 15 mmHg group vs 1.0% for the 6 mmHg groups (p ≤ 0.01).
Live donor nephrectomy
The gold standard for live donor nephrectomy is a laparoscopic approach. PNP pressure is particularly relevant because of tissue ischaemia on the donor organ. There were several papers on live donor nephrectomy that were not included as they assessed intraoperative physiological parameters from the perspective of an anaesthesiologist. A particular challenge faced in reducing bias in these papers was that male patients have more peri-renal fat than female patients, numbers of arteries vary between patients due to normal variation and the left kidney has more venous branches than the right. All these factors affect the difficulty of the operation.
Warlé and colleagues undertook a randomised and blinded pilot study whereby 20 patients were assigned to either undergo laparoscopic donor nephrectomy at 7 mmHg (n = 10), in the experimental arm, or at 14 mmHg (n = 10), in the control arm [11]. A scrub nurse, not involved in the operation, installed the PNP pressure after choosing a sealed envelope allocating the patient to the relevant arm. All screens and monitors displaying the pressure were covered, and healthcare staff performing the procedure were hence blinded.
Primary outcomes were the overall pain and nausea scores rated on a linear scale of 0 to 10 immediately post operation and then every 24 h for 3 days. The pain scores were collected by a blinded independent observer. They subdivided the pain scores into three dimensions; superficial wound pain, deep intraabdominal pain and referred shoulder pain. Secondary outcomes included length of stay and complications within the first month of the operation. Furthermore, a subjective score, by the surgeon, on a scale of 1–3 on the ‘difficulty’ and ‘progression’ of the operation (Scores 1, 2, or 3 corresponding with an easy, intermediate, or difficult procedure and quick, intermediate and slow progression). At 1 month post operation an SF-36 quality of life score was obtained.
Despite randomisation, discrepancies were observed between the final groups. The low-pressure group contained 6 patients with > 1 renal artery whereas the high-pressure group contained 0 patients with > 1 renal artery, a significant difference of p = 0.011. The low-pressure group comprised of 7 male patients as opposed to 3 in the high-pressure group. Finally, the low-pressure group contained only 1 right kidney whereas the high-pressure group contained 3. Un-blinding occurred in two patients. In one case, conversion from low to high pressure was indicated due to lack of progression and in the other significant bleeding (> 100 ml) from a vein also necessitated conversion.
Skin-to-skin time was significantly longer in the low-pressure group (111 min versus 149 min p = 0.003), due to the pneumoperitoneum phase of the procedure (86 min versus 126 min p = 0.001). Taking account of the before mentioned discrepancies between the low- and high-pressure groups, this may explain the difference. No statistically significant difference was observed in blood loss, progression or perceived difficulty of the operation. In the low-pressure group, there was significantly improved cumulative pain scores after 72 h for the deep intraabdominal (11 versus 7.5 p = 0.027) and referred shoulder pain (4.2 versus 1.8 p = 0.049) categories. No significant difference for the remaining post-operative parameters was demonstrated (including nausea score, complications, and SF-36). The complications included 1 haematoma in the standard pressure group and a pneumothorax and postoperative pneumonia in the low-pressure group. The pneumothorax occurred in a patient with severe peri-renal fibrosis where unblinding occurred intraoperatively. Despite this an iatrogenic diaphragmatic injury was the most likely cause of the pneumothorax. As such Warlé and colleagues concluded that live donor nephrectomy is safe at low pressure pneumoperitoneum and the low pressure may confer postoperative benefits.
Brunschot and colleagues (2017) performed a randomised and blinded study on live donor nephrectomy cases comparing PNPs of 6 mmHg and 12 mmHg [12]. A group of 64 patients were randomly allocated, using a computer-generated code, to the two arms of their trial, with 33 and 30 patients in the 6 mmHg and 12 mmHg groups, respectively. Gender and side of donor kidney were taken account of, to reduce confounding factors, however, no comment was made on the number of renal arteries or veins [12]. All surgeons and members of the research team were blinded during the operation. Every 15 min surgical conditions were assessed using the ‘Surgical Rating Score’ (SRS) on a scale of 1–5 (extremely poor, poor, adequate, good, and optimal) described by Martini et al. [13]. Where conditions were less than or equal to three, PNP was increased stepwise by 2 mmHg to a maximum of 12 mmHg. Where the pressure was already 12 mmHg, nurses were asked to pretend to increase the PNP pressure. The primary surgeon was asked to guess which arm of the experiment the patient belonged to at the end of each operation and in 82.5% of cases they were able to guess correctly. The ability to blind surgeons intraoperatively in challenging.
The primary outcome was the Quality of Recovery (QOR) which was measured using the patient reported ‘QOR-40 score’ on post-operative day 1. The QOR-40 score was further subdivided into the following domains: physical comfort, emotional status, physical independence, support, and pain. Secondary outcomes included analgesia requirements, operative time, blood loss and complication rates.
Intraoperatively 23 of the original 33 low pressure operations were completed at PNP 6 mmHg. In 2 cases the PNP pressure was increased to 8 mmHg, 2 were increased further to 10 mmHg and 6 were increased to the maximum 12 mmHg, thereby converting to standard pressure. The intraoperative timings of these pressure increases were not clear. The most relevant intraoperative complication that occurred was an iatrogenic bladder injury in a low pressure allocated patient; however, this patient had been increased to 10 mmHg prior to the injury and therefore it is difficult to attribute this to being secondary to low pressure.
No significant difference in the overall QOR-40 score was found between the groups from day 1 to day 7. However, on analysis of the specific dimensions, the low-pressure group had significantly better scores regarding physical support at day 1 (21.9 versus 19.9 p = 0.01), emotional status at day 1 (48.4 versus 46.3 p = 0.03) and physical independence (21.3 versus 19.7 p = 0.01) at day 2. No significant difference in analgesia consumption was observed between the low- and standard-pressure PNP group; however, the deep intra-abdominal pain component was significantly lower at postoperative day 2 (0.8 versus 1.8 p = 0.02) in patients allocated to the low-pressure group.
Partial nephrectomy
Desroches and colleagues studied 202 patients from three high volume centres to assess the safety of the Airseal Insufflation System (AIS) at different PNP pressures compared to a Conventional Insufflation System (CIS) at 15 mmHg [14]. The patients were randomised between three study arms, a 12 mmHg AIS, 15 mmHg AIS and 15 mmHg CIS. No mention is made regarding the method of randomisation or the number of surgeons undertaking these procedures across the three multicentre sites.
Primary outcome was the rate of subcutaneous emphysema. Secondary outcomes were additional postoperative complications including pneumothorax, pneumomediastinum, length of stay and postoperative pain. A secondary analysis was also undertaken into surgical approach due to the high number of retroperitoneal approaches used.
Rates of subcutaneous emphysema were reduced in the 12 mmHg AIS group regardless of the surgical approach when compared to the CIS 15 mmHg (4 versus 7 p = 0.003). No statistically significant difference was observed in secondary outcomes across the groups. The paper found AIS to be non-inferior to CIS and concluded that there may be benefits derived from a reduction in PNP pressure when used in conjunction with AIS.
Feng T and colleagues performed a study on 93 patients, divided into three groups. They varied both the insufflation pressures in addition to the insufflation device, between a conventional gas insufflator (CIS) and an Airseal insufflator (AIS) [15]. Each arm of their study had 31 patients randomly assigned to it by a computer-generated code. The arms were AIS 12 mmHg, AIS 15 mmHg and CIS 15 mmHg. Blinding was attempted by using envelopes, which contained the pressures at which the operations were to be undertaken. Both transperitoneal and retroperitoneal approaches were used within all arms. Approach was decided based on tumour location with posterior and lateral masses removed by retroperitoneal approach whilst anterior and medial masses were removed trans-peritoneally. Mention is not made of the laterality of the kidney operated on. The ratio of males to females in each group was, however, accounted for.
Primary outcome was the rate of subcutaneous emphysema measured intraoperatively with examinations every 30 min, with a postoperative chest plain radiograph. Secondary outcomes included rates of pneumothorax, pneumomediastinum, shoulder pain scores and overall pain scores measured using a visual analogue scale (VAS), pain medication usage, insufflation time, recovery room time, length of stay and impact of surgical approach.
The incidence of subcutaneous emphysema was significantly lower in the AIS 12 mmHg group compared to the CIS 15 mmHg group (19% versus 48% p = 0.03). In addition, mean pain score was less in AIS 12 mmHg compared to the CIS 15 mmHg group (3.1 versus 4.4 p = 0.03). No significant difference was demonstrated between morphine equivalent use, insufflation time, recovery room time and length of hospital stay. A multivariable regression analysis determined that use of the AIS at 12 mmHg and a transperitoneal approach were the only significant predictors for lower risk of developing subcutaneous emphysema. From the data, there is an inferred benefit to performing partial nephrectomy at a lower pressure and using the AIS system, as pain and subcutaneous emphysema rates are lower.
Mixed upper tract operations
Akkoc A et al. reviewed 76 mixed upper urinary tract operations performed over a 33-month period. For their study they used three arms, a 10 mmHg, 12 mmHg and 14 mmHg [16]. These were allocated as per the table below.
Akkoc A et al. reviewed 76 mixed upper urinary tract operations performed over a 33-month period. For their study they used three arms, a 10 mmHg, 12 mmHg and 14 mmHg (16). These were allocated as per the table below.
Inclusion | Exclusion |
|---|---|
Operations on the Genitourinary system | Primary/Secondary Outcomes: Peri-Operative or Physiological Variables |
Primary or Secondary Outcomes: Post-Operative | Non-human models used |
Methodology flowchart below:

Tables below outline bias:

Table below for the Mixed Upper Tract Akoc A section.
Operation | Group 1 10 mmHg | Group 2 12 mmHg | Group 3 14 mmHg |
|---|---|---|---|
Simple Nephrectomy (LSN) n = 28 | 9 | 9 | 10 |
Renal cyst decortications (LRCD) n = 28 | 9 | 9 | 10 |
Ureterolithotomies (LUL) n = 8 | 2 | 3 | 3 |
Pyelolithotomies (LPL) n = 6 | 2 | 2 | 2 |
Pyeolplasties (LPP) n = 6 | 2 | 2 | 2 |
Their primary outcome was postoperative pain measured at 6, 12, and 24 h postoperatively using a visual analogue scale (VAS), ranging from 0 to 10 (0, no pain; 10, the most severe pain). Patients were asked to disregard localised and sharp pain around the port incision to exclude parietal pain. The patients were instructed by the physician to complete the VAS, to evaluate any diffuse, dull aching pains in the abdomen or shoulder, representing visceral and referred visceral pains. Secondary outcomes were duration of surgery, intraoperative bleeding volume and length of hospital stay.
No randomisation or blinding methods were used in their study. Multiple different operations were grouped together for comparison with unequal numbers in each group. The operations were performed by four different surgeons whose experience was not mentioned or accounted for. The study was undertaken over a 33-month period, during which also gives rise to the possibility of a considerable learning curve difference. The text mentions that “when necessary, an additional 5 mm fourth trocar was selectively used for proper exposure or traction”. Where this was used it could be inferred that more postoperative pain may be experienced; however, this was not accounted for or mentioned in which operations it was used. Finally, the VAS system used was highly subjective, asking patients to ignore parietal pain and only report deep pain and shoulder tip pain.
Taking account of the considerable bias present in the method, the mean VAS score at 6 h was significantly reduced in the low-pressure group compared with the 14 mmHg group (4.13 versus 5.14 p = 0.011). However, no significant difference in the mean VAS scores at 24 h between the three groups was observed. The mean intraoperative bleeding volume was significantly higher in the low-pressure group compared with the higher-pressure groups (115.42 versus 85.2 versus 79.25 (p = 0.03 and p = 0.06). Mean operation time was longer in the 10 mmHg group than the higher-pressure groups, but this was not statistically significant. They concluded that Lower insufflation pressures were deemed to be associated with lower postoperative pain scores in the early postoperative period, however, as discussed, considerable bias was present within the methodology.
Discussion
To date, studies investigating the effect of pneumoperitoneum pressures during urological procedures are relatively lacking when compared to general surgery and gynaecology. The available literature is divided mostly between papers discussing prostatectomy and live donor nephrectomy with only three other papers identified that discuss partial nephrectomy and other mixed operations. Within this, the papers are divided between those discussing anaesthetic parameters such as the effects of PNP pressure on intraoperative mean arterial pressure and those that were included in this review that discuss surgical and post-operative clinical outcomes.
Though limited, the papers discussing the effects of PNP pressure on clinical outcomes in urological surgery agreed that low pressure pneumoperitoneum was non-inferior to standard pressure PNP. Some papers identified significant benefits associated with the use of low pressure PNP. Several papers identified a reduction in postoperative pain and ileus rates by using lower pressures. These result in reduced hospital stays and one paper had established parameters for discharging low-pressure prostatectomy patients the same day as operating. This aids patient satisfaction and reduces costs associated with overnight hospital stays and their complications.
Low pressure PNP does appear to be associated with significantly longer operating times. This may be secondary to impaired visualisation that can hamper progression. However, despite investigator blinding, patient allocation to a ‘low pressure’ may be strongly suspected intra-operatively by the surgeon and this will likely influence the time taken at critical operative steps. Moreover, several papers didn’t use any blinding and were retrospective studies where the same caution applies.
The anaesthetic and physiological implications of lower pressure pneumoperitoneum have been demonstrated by multiple studies. These include reduced lactate levels and more favourable cytokine responses [17,18,19,20,21]. These findings have a presumptive benefit, however, how they translate to reduced complication rates and reduced morbidity and mortality is to date undemonstrated. The benefits may lie in operating on patients with multiple comorbidities where small adjustments in the PNP pressure may make anaesthesia safer and thereby possible.
By starting at lower PNP pressures, that still produce a clear and safe visual field, surgeons can mitigate the potentials disadvantages, as outlined above, with higher PNP pressures. The option of increasing to higher PNP pressures is available, for example, to apply compression in the context of haemorrhage. This technique is already employed by some surgeons during prostatectomy to aid in the dissection of the dorsal venous complex to reduce ooze.
Research is required on the feasibility and safety of performing nephrectomies and cystectomies, at lower pressures. Whether any advantage such as reduced rates of ileus, a common complication following cystectomy, is achievable in all urological procedures is yet to be demonstrated in the literature. Most studies investigated peri-operative anaesthetic parameters, and few assessed the post-operative outcomes, including morbidity and mortality, as their primary outcome.
Conclusion
On review of the published literature, performing laparoscopic urological operations under lower pressure pneumoperitoneum appears safe and non-inferior to standard and high pressures. There is some early evidence to suggest benefits to clinical outcomes of using low pressure PNP but higher-powered randomised trials are required to corroborate this. Further research should include both low pressure pneumoperitoneum during nephrectomy and cystectomy where to date, there is no literature.
References
Sodha S, Nazarian S, Adshead JM, Vasdev N, Mohan-S G (2015) Effect of pneumoperitoneum on renal function and physiology in patients undergoing robotic renal surgery. Curr Urol 9(1):1–4
Vigneswaran Y, Prachand VN, Posner MC, Matthews JB, Hussain M (2020) What is the appropriate use of laparoscopy over open procedures in the current COVID-19 climate? J Gastrointest Surg Off J Soc Surg Aliment Tract 24(7):1686–1691
Özdemir-van Brunschot DMD, van Laarhoven KCJHM, Scheffer GJ, Pouwels S, Wever KE, Warlé MC (2016) What is the evidence for the use of low-pressure pneumoperitoneum? A systematic review. Surg Endosc 30(5):2049–2065
Mazzinari G, Diaz-Cambronero O, Serpa Neto A, Martínez AC, Rovira L, Argente Navarro MP et al (2021) Modeling intra-abdominal volume and respiratory driving pressure during pneumoperitoneum insufflation-a patient-level data meta-analysis. J Appl Physiol 130(3):721–728
Gurusamy KS, Samraj K, Davidson BR (2009) Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev 2:CD006930
Hinneburg I (2017) ROBINS-1: a tool for assessing risk of bias in non-randomised studies of interventions. Med Monatsschr Pharm 40(4):175–177
Christensen CR, Maatman TK, Maatman TJ, Tran TT (2016) Examining clinical outcomes utilizing low-pressure pneumoperitoneum during robotic-assisted radical prostatectomy. J Robot Surg 10(3):215–219
Rohloff M, Cicic A, Christensen C, Maatman TK, Lindberg J, Maatman TJ (2019) Reduction in postoperative ileus rates utilizing lower pressure pneumoperitoneum in robotic-assisted radical prostatectomy. J Robot Surg 13(5):671–674
Rohloff M, Peifer G, Shakuri-Rad J, Maatman TJ (2020) The impact of low pressure pneumoperitoneum in robotic assisted radical prostatectomy: a prospective, randomized, double blinded trial. World J Urol 39:2469–2474
Ferroni MC, Abaza R (2019) Feasibility of robot-assisted prostatectomy performed at ultra-low pneumoperitoneum pressure of 6 mmHg and comparison of clinical outcomes vs standard pressure of 15 mmHg. BJU Int 124(2):308–313
Warlé MC, Berkers AW, Langenhuijsen JF, van der Jagt MF, Dooper PM, Kloke HJ et al (2013) Low-pressure pneumoperitoneum during laparoscopic donor nephrectomy to optimize live donors’ comfort. Clin Transplant 27(4):E478–E483
Özdemir-van Brunschot DMD, Scheffer GJ, van der Jagt M, Langenhuijsen H, Dahan A, Mulder JEEA et al (2017) Quality of recovery after low-pressure laparoscopic donor nephrectomy facilitated by deep neuromuscular blockade: a randomized controlled study. World J Surg 41(11):2950–2958
Martini CH, Boon M, Bevers RF, Aarts LP, Dahan A (2014) Evaluation of surgical conditions during laparoscopic surgery in patients with moderate vs deep neuromuscular block. Br J Anaesth 112(3):498–505
Desroches B, Porter J, Bhayani S, Figenshau R, Liu P-Y, Stifelman M (2021) Comparison of the safety and efficacy of valveless and standard insufflation during robotic partial nephrectomy: a prospective, randomized, multi-institutional trial. Urology 153:185–191
Feng TS, Heulitt G, Islam A, Porter JR (2021) Comparison of valve-less and standard insufflation on pneumoperitoneum-related complications in robotic partial nephrectomy: a prospective randomized trial. J Robot Surg 15(3):381–388
Akkoc A, Topaktas R, Aydin C, Altin S, Girgin R, Yagli OF et al (2017) Which intraperitoneal insufflation pressure should be used for less postoperative pain in transperitoneal laparoscopic urologic surgeries? Int Braz J Urol 43(3):518–524
Aditianingsih D, Mochtar CA, Lydia A, Siregar NC, Margyaningsih NI, Madjid AS et al (2020) Effects of low versus standard pressure pneumoperitoneum on renal syndecan-1 shedding and VEGF receptor-2 expression in living-donor nephrectomy: a randomized controlled study. BMC Anesthesiol 20(1):37
Hawasli A, Oh H, Schervish E, Frontera R, Gonsherova I, Khoury H (2003) The effect of pneumoperitoneum on kidney function in laparoscopic donor nephrectomy. Am Surg 69(4):300–303 (discussion 303)
Mertens zur Borg IM, Lim A, Verbrugge SC, IJzermans JM, Klein J (2004) Effect of intraabdominal pressure elevation and positioning on hemodynamic responses during carbon dioxide pneumoperitoneum for laparoscopic donor nephrectomy: a prospective controlled clinical study. Surg Endosc 18(6):919–923
Ciko P, Widia F, Hamid ARAH, Wahyudi I, Mochtar CA (2019) Effect of pneumoperitoneum on renal resistive index and renal function in patients who have undergone laparoscopic living donor nephrectomy: a pilot study. Transplant Proc 51(6):1727–1731
Vodopija N, Ovcak Z, Zupancic M, Korsic L, Kramer F, Krstanoski Z et al (2009) Tissue ischemia due to CO2 pressure during laparoscopic radical prostatectomy. Coll Antropol 33(1):77–82
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
West, A., Hayes, J., Bernstein, D.E. et al. Clinical outcomes of low-pressure pneumoperitoneum in minimally invasive urological surgery. J Robotic Surg 16, 1183–1192 (2022). https://doi.org/10.1007/s11701-021-01349-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-021-01349-7